Brief explanation of Glaucoma
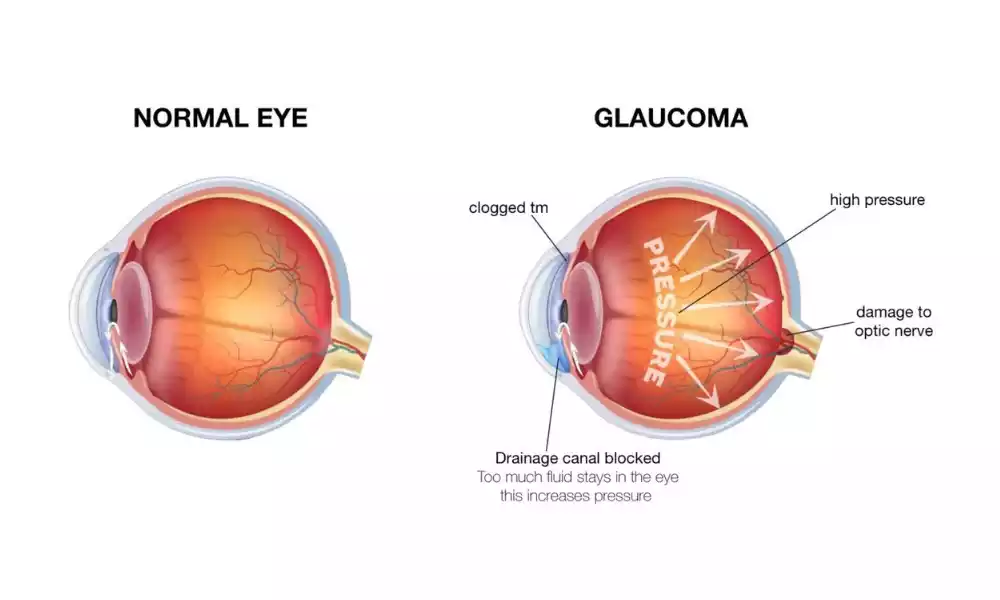
Glaucoma is a chronic eye condition characterized by damage to the optic nerve, which is responsible for transmitting visual information from the eye to the brain. This damage is often associated with elevated intraocular pressure (IOP), but it can occur even when IOP is within the normal range. Glaucoma typically progresses slowly and can lead to gradual vision loss, starting with peripheral vision and eventually affecting central vision.

There are different types of glaucoma, but the most common is open-angle glaucoma, which develops gradually and often goes unnoticed until significant vision loss occurs. Angle-closure glaucoma, another type, is less common but can develop suddenly and cause rapid vision impairment.
Early detection through regular eye exams is crucial for managing glaucoma, as it can be treated to slow or prevent further vision loss. However, because glaucoma often presents without noticeable symptoms in its early stages, routine eye check-ups are essential, especially for individuals with risk factors such as a family history of the condition, older age, or specific ethnic backgrounds.
Types of glaucoma
There are several types of glaucoma, each with its own characteristics, causes, and treatment approaches. The main types of glaucoma include:
- Primary Open-Angle Glaucoma (POAG):
- Also known as chronic open-angle glaucoma, this is the most common type.
- It develops slowly over time.
- The drainage angle of the eye appears normal, but there is gradual blockage of the trabecular meshwork, which results in increased intraocular pressure (IOP).
- Often asymptomatic in its early stages.
- Vision loss typically starts with peripheral vision and progresses to central vision.
- Angle-Closure Glaucoma:
- Also called acute glaucoma or narrow-angle glaucoma.
- This type develops suddenly and requires immediate medical attention.
- It occurs when the drainage angle of the eye becomes blocked or closed, leading to a rapid increase in IOP.
- Normal-Tension Glaucoma (NTG):
- In NTG, optic nerve damage and visual field loss occur despite having IOP within the normal range.
- The exact cause of this type of glaucoma is not fully understood.
- Treatment aims to lower IOP to levels even lower than normal to slow down or halt the progression of the disease.
- Secondary Glaucoma:
- This type of glaucoma is a result of other eye conditions or factors.
- Secondary glaucoma can be caused by various factors, such as eye injuries, certain medications (steroids), eye tumors, uveitis, or elevated eye pressure due to other medical conditions.
- Congenital Glaucoma:
- Present at birth or develops in infancy.
- Typically caused by a structural abnormality in the eye’s drainage system.
- Symptoms may include enlarged eyes, excessive tearing, light sensitivity, and cloudiness of the cornea.
Each type of glaucoma requires specific diagnostic and treatment approaches. Early detection and appropriate management are crucial for preserving vision and preventing further damage. Regular eye exams are essential, especially for individuals at higher risk due to factors like age, family history, or specific medical conditions.
A brief explanation of Ocular hypertension
Ocular hypertension refers to elevated intraocular pressure (IOP) within the eye, but it is distinct from glaucoma. In ocular hypertension, there is increased pressure inside the eye, which can be a risk factor for developing glaucoma but does not necessarily cause optic nerve damage or vision loss on its own.

People with ocular hypertension typically do not experience noticeable symptoms, and their vision remains normal. However, the elevated IOP can increase the risk of developing glaucoma over time, especially if other risk factors like age, family history, or a thin cornea are present.
Monitoring and regular eye exams are essential for individuals with ocular hypertension to detect any early signs of glaucoma. Some cases of ocular hypertension may require treatment, often in the form of eye drops or other medications, to lower IOP and reduce the risk of developing glaucoma. However, not everyone with ocular hypertension will develop glaucoma, and the condition may remain stable without progressing to more serious eye problems.
Prognosis and management
The prognosis and management of glaucoma depend on several factors, including the type of glaucoma, the stage at which it is diagnosed, the effectiveness of treatment, and the patient’s compliance with treatment and follow-up care.
Here is an overview of the prognosis and management of glaucoma:
Prognosis:
- Early Detection: The prognosis for glaucoma is generally better when the condition is detected in its early stages. Regular eye exams are crucial for early detection, as many types of glaucoma are asymptomatic until vision loss has occurred.
- Treatment Effectiveness: The effectiveness of treatment in lowering intraocular pressure (IOP) plays a significant role in the prognosis. Lowering IOP can slow down or halt the progression of the disease and preserve vision.
- Adherence to Treatment: Patient compliance with treatment, including taking prescribed medications and attending regular follow-up appointments, is essential for a positive prognosis. Poor adherence can lead to uncontrolled IOP and an increased risk of vision loss.
- Type of Glaucoma: The prognosis can vary depending on the type of glaucoma. For example, angle-closure glaucoma often presents suddenly and requires immediate treatment to prevent severe vision damage, while primary open-angle glaucoma progresses slowly over time.
Management:
- Medications: The primary treatment approach for glaucoma involves medications, such as eye drops, that lower IOP. Different classes of eye drops can be prescribed, including prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors. These medications work to reduce the production of aqueous humor (the fluid inside the eye) or increase its outflow.
- Laser Therapy: Laser treatments like selective laser trabeculoplasty (SLT) or laser peripheral iridotomy (LPI) can be used to help lower IOP. These procedures are often considered when medications alone are insufficient.
- Surgical Procedures: When medications and laser therapy do not adequately control IOP, surgical options may be recommended. These can include trabeculectomy, tube shunt implantation, or minimally invasive glaucoma surgery (MIGS).
- Lifestyle Modifications: Lifestyle changes can help manage glaucoma. Patients are often advised to maintain a healthy lifestyle, avoid smoking, and manage conditions like diabetes and high blood pressure, which can exacerbate glaucoma.
- Regular Monitoring: Regardless of the treatment method, ongoing monitoring of IOP and regular eye exams are essential. This allows healthcare providers to assess the effectiveness of treatment and make necessary adjustments.
while glaucoma is a chronic condition, with proper management and early intervention, many individuals can maintain good vision and prevent further damage. However, because glaucoma is often asymptomatic until later stages, regular eye exams are fundamental to its effective management and preserving vision.
Glaucoma and Ocular Hypertension Comparative chart
Here’s a comparative chart highlighting the key differences between glaucoma and ocular hypertension:
| Characteristic | Glaucoma | Ocular Hypertension |
|---|---|---|
| Definition | Chronic eye condition with optic nerve damage | Elevated intraocular pressure (IOP) without optic nerve damage |
| Vision Loss | This can lead to gradual vision loss | Typically no vision loss or symptoms |
| Symptoms | Often presents with symptoms like peripheral vision loss, halos around lights | Usually asymptomatic, but may cause occasional eye discomfort |
| Diagnosis | Confirmed by detecting optic nerve damage and elevated IOP | Diagnosed by measuring elevated IOP through tonometry |
| Risk for Glaucoma | Patients already have glaucoma | Patients at risk of developing glaucoma |
| Causes | Increased IOP, age, family history, race, ethnicity | Age, family history, high myopia, thin cornea, among others |
| Treatment | Requires treatment to lower IOP and prevent further damage | May require treatment to lower IOP and reduce the risk of glaucoma |
| Prognosis | Lifelong condition requiring ongoing management | The risk of developing glaucoma necessitates regular monitoring |
| Lifestyle Modifications | Encouraged to lead a healthy lifestyle, avoid smoking, and manage comorbid conditions | Similar lifestyle modifications as in glaucoma |
| Medications and Surgery Options | Medications, laser therapy, and surgical procedures may be necessary | Medications and laser therapy may be used, surgery is less common |
| Regular Monitoring | Regular eye exams and IOP measurements essential | Ongoing monitoring to detect any progression or signs of glaucoma |
| Vision Preservation | Early intervention is crucial for preserving vision | Early intervention to lower IOP reduces the risk of developing glaucoma |
| Common Types | Open-angle, angle-closure, secondary, congenital, and more | Typically a risk factor rather than a distinct type |
| Preventive Measures | Focus on preventing further vision loss and managing symptoms | Focus on reducing IOP to lower the risk of developing glaucoma |
This chart provides a concise comparison between glaucoma and ocular hypertension, highlighting their differences in terms of definition, symptoms, diagnosis, risk factors, treatment, and prognosis.
Similarities between glaucoma and Ocular Hypertension
Similarities between Glaucoma and Ocular Hypertension:
- Elevated Intraocular Pressure (IOP): Both conditions involve elevated pressure inside the eye, with increased IOP being a common factor.
- Risk for Glaucoma: Ocular hypertension is a significant risk factor for developing glaucoma. Individuals with ocular hypertension have an increased likelihood of progressing to glaucoma.
- Regular Monitoring: Both conditions require regular eye exams and IOP measurements to detect changes and assess the need for treatment or management.
- Lifestyle Modifications: Lifestyle changes, such as avoiding smoking and managing other health conditions, are encouraged for individuals with both conditions to support eye health and reduce the risk of complications.
- Management Options: While the treatment approaches differ, both conditions can benefit from management strategies aimed at lowering IOP and preventing or delaying the onset of glaucoma.
Final word
Understanding the differences and similarities between glaucoma and ocular hypertension is crucial for maintaining eye health. Glaucoma is a chronic condition characterized by optic nerve damage and vision loss, often requiring ongoing treatment and monitoring.
Ocular hypertension, on the other hand, involves elevated intraocular pressure without immediate vision loss but is a significant risk factor for developing glaucoma. Both conditions necessitate regular eye exams, lifestyle modifications, and, in some cases, treatment to preserve vision and reduce the risk of complications. Early detection and proper management are key to ensuring the best possible outcomes for individuals affected by these eye conditions.