Definition of Heel Spurs and Plantar Fasciitis
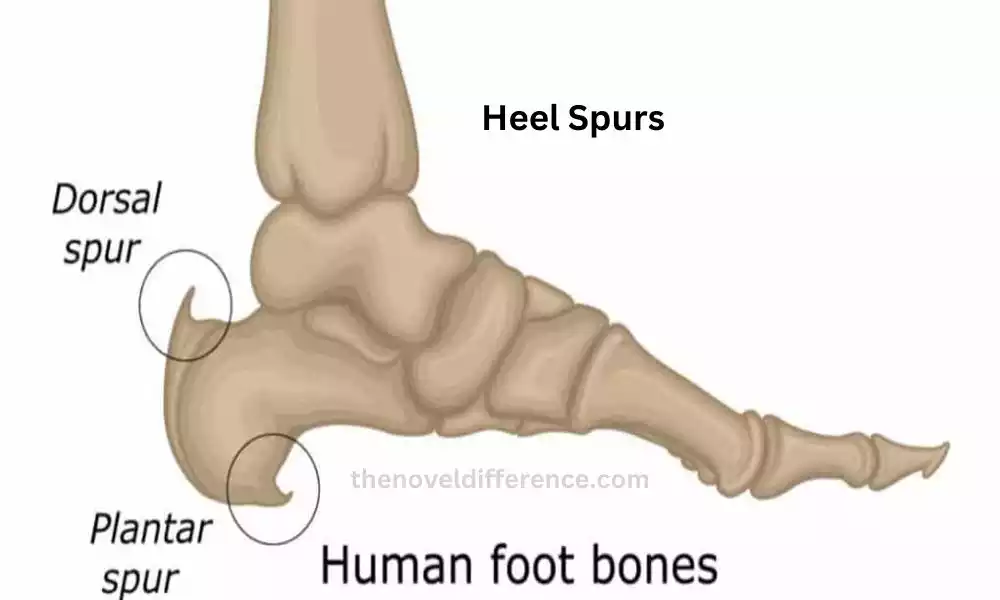
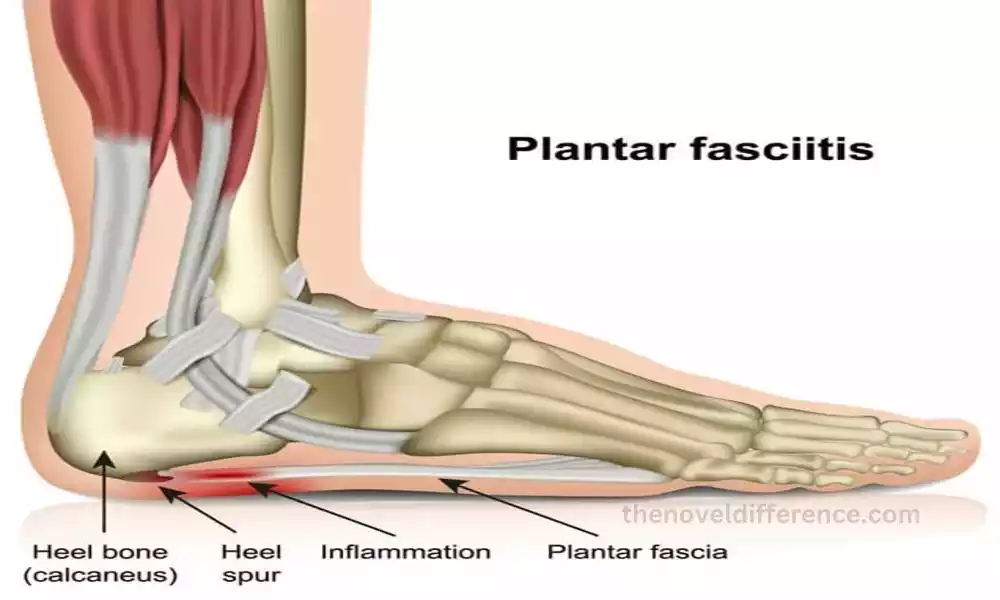
Heel spurs: Heel spurs, also known as calcaneal spurs, are bony growths that form on the bottom or back of the heel bone (calcaneus). Plantar fasciitis, although they can occur independently. Heel spurs develop as a result of calcium deposits that gradually accumulate over time.
These calcium deposits usually form in response to chronic strain or inflammation in the plantar fascia, a thick band of connective tissue that supports the arch of the foot.
When exposed to repeated strain, tension, or stress on the plantar fascia, your body may respond by depositing calcium at its source. Over time, these deposits can develop into small, bony protrusions, creating the heel spur.
Noting the heel spur itself does not necessarily result in pain or discomfort, nor must it necessarily lead to ongoing problems for its wearer. In fact, many people with heel spurs are asymptomatic.
When the spurs irritate the surrounding soft tissues or press against nerves, they can lead to heel pain, particularly during weight-bearing activities such as walking or standing.
Diagnosing heel spurs usually involves physical examination by a healthcare provider who may also order imaging tests such as x-rays or ultrasounds to confirm their existence.
Treatment for heel spurs generally focuses on managing the underlying causes of inflammation and relieving associated pain. This may include rest, activity modification, ice therapy, anti-inflammatory medications, stretching exercises, physical therapy, and the use of supportive devices like custom orthotic inserts or heel cups.
More advanced treatments such as extracorporeal shockwave therapy (ESWT) or surgery may be considered if conservative measures do not provide sufficient relief.
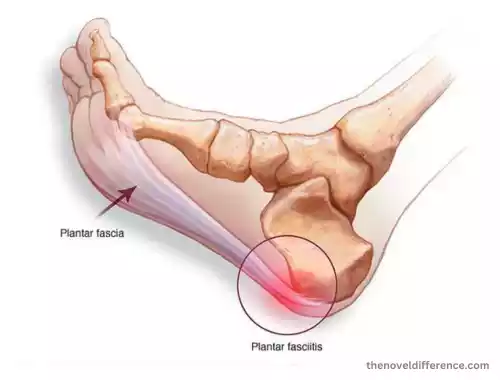
Plantar fasciitis: Plantar fasciitis refers back to inflammation of the plantar facia which is a large stretch of connective tissue through the sole of your foot, starting from the heel bone (calcaneus) until your toes. The plantar fascia acts as a supportive structure for the arch of the foot and helps absorb shock during walking and running.
Plantar fasciitis typically develops when the plantar fascia becomes overstretched or experiences excessive strain. Foot pain may result from several sources, including activities that repetitively place stress on them such as running, jumping, and prolonged standing.
Other contributing factors may include foot abnormalities, improper footwear, sudden weight gain, tight calf muscles, or changes in foot mechanics.
Plantar fasciitis can be identified by excruciating heel pain on its underside – typically found near where your arch would normally rest. The pain is often described as a stabbing or sharp sensation and is usually more pronounced in the morning or after periods of rest.
As the affected person starts to move and walk, the pain tends to decrease but may return after prolonged activity.
Plantar fasciitis can usually be diagnosed through physical examination by healthcare providers who will look out for signs such as swelling, tenderness or limited movement of the foot affected.
The clinical history and the characteristic pattern of pain also play a significant role in the diagnosis. Imaging tests such as X-rays or magnetic resonance imaging (MRI) may be undertaken in certain instances to rule out other potential causes of heel pain.
Treatment for plantar fasciitis should focus on decreasing inflammation, soothing discomfort, and encouraging healing.
It often includes a combination of conservative measures, such as rest and activity modification, applying ice to the affected area, using over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), wearing supportive footwear or orthotic inserts, and performing stretching and strengthening exercises for the foot and calf muscles.
When conservative treatments do not bring sufficient relief, additional options such as corticosteroid injections or extracorporeal shockwave therapy (ESWT), or, in extreme circumstances, surgical intervention could be considered.
Early intervention and effective management are vitally important to effectively treating plantar fasciitis and preventing its chronic development. It is recommended to seek medical advice if persistent heel pain is experienced.
Overview of common foot conditions
The feet are complex structures that support the weight of the body and facilitate movement. Several common foot conditions can affect the feet, causing discomfort, pain, and mobility issues.

Here is an overview of some of the most prevalent foot conditions:
Plantar Fasciitis: This condition refers to an inflammation in the plantar fascia, an area connecting your heel bone to each toe that connects you directly. It causes heel pain, especially during the first steps in the morning or after periods of rest.
Heel Spurs: Heel spurs are bony growths that develop on the heel bone. Plantar fasciitis can lead to heel pain and discomfort when performing weight-bearing activities such as walking.
Bunions: Bunions are bony bumps that form at the base of the big toe. They result from the misalignment of the joint, causing the big toe to lean toward the other toes. Bunions can be painful and lead to difficulties in finding properly fitting footwear.
Corns and Calluses: Corns and calluses are thickened areas of skin that develop due to repeated friction or pressure. Corns are usually small and develop on the toes, while calluses are larger and typically form on the soles of the feet. They can cause discomfort and pain if they become too thick.
An Ingrown Nail: When nails grow into the surrounding skin and penetrate deeply enough, an ingrown toenail may develop, leading to pain, redness, swelling, and possible infection. Improper nail trimming, tight footwear, or injury can contribute to ingrown toenails.
Morton’s Neuroma: Morton’s neuroma is a thickening of the tissue around a nerve leading to the toes, often between the third and fourth toes. Painful blisters on the toes may result in sharp, burning pain as well as tingling or numbness in those toes.
Achilles Tendinitis: Achilles tendinitis refers to inflammation in the Achilles tendon that joins calf muscles with the heel bone. It commonly occurs due to overuse or repetitive strain and causes pain, stiffness, and swelling in the back of the leg, just above the heel.
Flat Feet: Flat feet, also known as fallen arches, occur when the arches of the feet collapse, causing the entire sole to touch the ground. It can lead to foot pain, instability, and difficulty with certain activities.
Hammer Toe: Hammer’s toe is a deformity of the toes, characterized by an abnormal bend in one or more joints. Ankle pain typically involves the second, third, and fourth toes resulting in swelling, discomfort, and difficulty wearing certain footwear.
Plantar Warts: Plantar warts are caused by an infection with viruses infecting your skin – specifically on the soles of your feet. They can be painful and may appear as small, rough growths with black dots in the center.
It’s important to note that proper diagnosis and treatment by a healthcare professional or podiatrist are crucial for these foot conditions. They can provide personalized advice and recommend appropriate treatment options to alleviate symptoms and improve foot health.
Heel Spurs
Heel spurs are bony growths that develop on the bottom or back of the heel bone (calcaneus). Plantar fasciitis and heel spurs tend to occur simultaneously; however, both can exist separately and independently. Heel spurs are formed as a result of calcium deposits gradually accumulating over time.
Heel spurs are usually caused by strain or inflammation of the plantar fascia – an interwoven band of connective tissue that serves to support the arch of your foot.
When exposed to repetitive strain, or stress on the plantar fascia, the body reacts by depositing calcium at its point of strain. Over time, these deposits can form into bony protrusions, resulting in heel spurs.
It’s important to note that heel spurs themselves may not always cause symptoms or pain. Many people with heel spurs are asymptomatic and are unaware of their presence.
When the spurs irritate the surrounding tissues or press against nerves, they can lead to heel pain, particularly during weight-bearing activities such as walking or standing.
The diagnosis of heel spurs typically involves a physical examination by a healthcare professional or podiatrist. They may assess the foot for tenderness, swelling, or other signs of inflammation. Imaging tests such as X-rays or ultrasound may be ordered to confirm the presence of the bony growths.
Treatment for heel spurs primarily focuses on managing the underlying inflammation and providing pain relief. This often includes a combination of conservative measures, such as rest, activity modification, ice therapy, and over-the-counter anti-inflammatory medications.
Stretching exercises and physical therapy may be prescribed in order to increase flexibility and alleviate strain on the plantar fascia.
Orthotic devices, such as custom shoe inserts or heel cups, can help provide cushioning and support to alleviate discomfort. In some cases, extracorporeal shockwave therapy (ESWT) may be utilized to stimulate healing and reduce inflammation.
Surgical intervention is rarely necessary and is typically considered only when conservative treatments fail to provide relief.
People experiencing persistent or severe heel pain must consult with a healthcare professional or podiatrist in order to receive an accurate diagnosis and personalized treatment plan designed specifically for their situation.
Plantar Fasciitis
Plantar fasciitis, also known as heel spur syndrome, is an extremely prevalent foot condition characterized by inflammation of the plantar facia tissue located along the bottom of your foot and connecting your heel bone (calcaneus) and toes.
The plantar fascia offers support for the arches of your feet and also acts in the role of absorbing shock while running and walking. The precise causes of plantar fasciitis are typically multifactorial, however, it usually results from repeated strain or excessive use in the plantar fascia.
The most common causes that contribute to the formation of plantar fasciitis are:
Repetitive or excessive use: Engaging in repetitive or prolonged use Activities that place excessive strain on the feet such as jumping, running, or standing for extended periods such as jumping can result in pain and strain to ligaments of the plantar fascia and cause further strain to its ligaments.
foot mechanics: Foot mechanics that are not normal like low arches (fallen arches) or arches with high arches could alter the weight distribution and put more stress on the plantar fascia.
Shoes that are not properly fitted: Wearing shoes with poor arch support or cushioning, as well as poor fitting can lead to the development of plantar fasciitis.
The weight and the age of an individual: Plantar fasciitis is more prevalent in middle-aged people or those obese or overweight due to pressure that is increased on the feet.
The main sign of plantar fasciitis is heel pain, especially near the heel’s bottom. The pain is usually acute and sharp and is usually particularly painful in the mornings when you are taking your first steps or following a time of relaxation. When the foot is warm and expands during the course of the day discomfort may ease, but it can recur after a prolonged period of activity.
The diagnosis of plantar fasciitis is typically based on a physical examination conducted by a medical professional or podiatrist. They’ll examine your foot to look for swelling, tenderness, and indications of inflammation. Imaging tests like X-rays and magnetic resonance images (MRI) are not usually needed, but they may be required to rule out possible causes of heel pain.
The treatment for plantar fasciitis seeks to decrease inflammation, and pain and speed up healing. These are the most common methods of treatment:
Rest and modification of activities: Avoid activities that cause more discomfort and permit the plantar fascia to heal.
Therapy with Ice: Apply ice on the area of concern to help reduce inflammation and pain.
Exercising for stretch: Performing specific stretching exercises to stretch and build the plantar fascia and its surrounding muscles.
Devices for orthotics: Wearing shoe inserts or orthotic devices that are custom-made to help support arch posture and cushioning.
Nonsteroidal Anti-Inflammatory Medication (NSAIDs): Over-the-counter remedies such as naproxen and ibuprofen can provide temporary relief by acting to lower inflammation levels and decrease discomfort levels.
Corticosteroid injections: Corticosteroid injections can be suggested to ease acute discomfort and inflammation.
Therapy for physical injuries: Working with a physical therapist, you will receive specific treatments, manual therapy, and other therapies to aid in recovery and improve the foot’s mechanics.
Surgery is generally considered to be an option last resort and only suggested if conservative treatments have failed for a long time or when there is a structural problem that is causing the problem.
People experiencing chronic or increasing heel pain should consult a medical provider such as a physician or podiatrist in order to obtain an accurate diagnosis and tailored treatment program that suits their unique health status. Early intervention and proper management will often result in the successful treatment of plantar fasciitis symptoms.
Differences Between Heel Spurs and Plantar Fasciitis
Though plantar fasciitis and heel spurs are often related and occur together, However, these are distinct ailments with distinct characteristics.
These are the major distinctions between heel spurs and plantar fasciitis:
Site: Heel spurs refer to bony growths that grow at the back or bottom of the heel bone (calcaneus). Plantar fasciitis, on the contrary, is a complication that causes inflammation in the plantar fascia (an important anatomical layer that connects the heel with the big toe).
Cause and the reason for it: Heel spurs are mostly caused by inflammation and strain on the foot, specifically in the plantar fascia. The constant stress causes the deposition of calcium as well as the formation of a bony spur. However plantar fasciitis is a swelling of the plantar facia, mostly due to micro-tears, or even overuse. Heel spurs are often an outcome of chronic plantar fasciitis. However, they may also occur on their own.
Signs and symptoms: Heel spurs may cause symptoms or not. If there is a problem, their most common indication is heel pain particularly during activities that require weight, such as sitting or walking. The pain is typically described as a stabbing or sharp sensation that occurs in the heel. Plantar fasciitis, on the contrary, is usually manifested as severe heel pain, especially after waking up in the morning or after long intervals of relaxation. The pain is likely to ease as you move but can recur following activities.
Diagnostics and imaging: Diagnosis of plantar fasciitis and heel spurs typically requires a physical examination by a health specialist or podiatrist. However, determining the cause of heel spurs is usually based on imaging tests, such as X-rays or ultrasounds.
The bony growths are visible on X-rays, however, plantar fasciitis diagnosis is usually by a clinical examination and symptoms. Imaging can be utilized in the case of plantar fasciitis to rule out other possible causes of pain in the heel.
Treatment strategies: While there is some overlap in treatment strategies for both ailments, however, there are some slight distinctions. The treatment for heel spurs is focused on managing inflammation and the strain on the heel and easing pain.
It could involve rest treatment, ice therapy or stretching exercises, anti-inflammatory drugs as well as using orthotic devices. Treatment for plantar fasciitis typically aims to decrease inflammation, alleviate pain and speed up fascial repair.
Stretching exercises, relaxation exercises orthotic devices, and nonsteroidal anti-inflammatory medications (NSAIDs) can all play an essential role in easing back pain. in certain situations, corticosteroid injections and physical therapy may also aid.
Notably, plantar fasciitis and heel spurs often co-occur, so treating one may help alleviate symptoms associated with both. Consultations with medical professionals or podiatrists may provide accurate diagnoses and customized therapy solutions tailored specifically to each individual’s health issue.
What are the similarities between Heel Spurs and Plantar Fasciitis?
Heel spurs and plantar fasciitis are closely related conditions that often occur together. While heel spurs and plantar fasciitis differ significantly, there are also numerous similarities.
Here are the main similarities:
Association: Heel spurs and plantar fasciitis are commonly associated with each other. Heel spurs often develop as a result of long-standing plantar fasciitis. Chronic inflammation and strain on the plantar fascia can lead to the formation of bony growths (heel spurs) on the heel bone.
Symptoms: Both conditions can cause heel pain. Heel spurs and plantar fasciitis are often present with similar symptoms, including sharp or stabbing pain in the heel. Pain typically worsens during weight-bearing activities like walking or standing and may increase after periods of rest or in the morning.
Contributing Factors: Certain factors can contribute to the development of both conditions. These include repetitive strain or overuse of the feet, such as running or standing for long periods. Poor foot mechanics such as flat feet or high arches increase the risk of heel spurs and plantar fasciitis.
Diagnosis: Diagnosing heel spurs and plantar fasciitis requires a physical exam by either a healthcare provider or podiatrist. Both conditions are often diagnosed based on clinical evaluation, symptom assessment, and the presence of heel pain. Imaging tests such as X-rays or ultrasounds may be utilized in order to confirm or eliminate other potential causes of heel pain.
Treatment Approach: The initial treatment approaches for heel spurs and plantar fasciitis overlap to a significant extent. Conservative measures are often recommended as the first line of treatment for both conditions. These may include rest, activity modification, ice therapy, stretching exercises, and the use of supportive devices like orthotic inserts. Nonsteroidal anti-inflammatory drugs (NSAIDs) may help to both decrease inflammation and relieve discomfort in both instances.
Plantar fasciitis and heel spurs share many symptoms; however, not all instances of plantar fasciitis correspond with heel spurs; all heel spurs should be treated equally. Therefore, seeking an expert medical diagnosis to properly identify what’s causing heel pain will provide more effective care plans tailored to each patient’s needs.
Heel Spurs vs Plantar Fasciitis in Tabular Form
Sure! Here’s a comparison of heel spurs and plantar fasciitis in tabular form:
| Aspect | Heel Spurs | Plantar Fasciitis |
|---|---|---|
| Definition | Bony growths on the heel bone | Inflammation of the plantar fascia |
| Location | Bottom or back of the heel bone | Plantar fascia, primarily at the heel |
| Cause | Calcium deposits, often associated with strain or inflammation of the plantar fascia | Overuse, injury, or biomechanical factors |
| Symptom | Heel pain, especially during weight-bearing activities | Intense heel pain, particularly in the morning or after rest |
| Diagnosis | Physical examination, imaging tests (X-ray, ultrasound) | Physical examination, clinical history, symptom assessment, imaging tests (rarely) |
| Treatment | Rest, ice therapy, anti-inflammatory medications, stretching exercises, orthotic inserts, shockwave therapy, surgery (rare cases) | Rest, stretching exercises, orthotic inserts, NSAIDs, corticosteroid injections (severe cases), shockwave therapy, surgery (rare cases) |
It’s important to note that while there are similarities and overlaps between the two conditions, each person’s case may vary. Consultation with a health practitioner or podiatrist is highly advised for accurate diagnosis and tailored treatments.
Conclusion
Heel spurs and plantar fasciitis are related foot conditions, but they have distinct differences. Heel spurs are bony growths that develop on the bottom or back of the heel bone, often associated with chronic strain and inflammation of the plantar fascia.
Plantar fasciitis refers to inflammation of the plantar fascia caused by overuse, injury, or biomechanical issues.
Both conditions can cause heel pain, with heel spurs often occurring alongside plantar fasciitis. Diagnosing usually includes physical examination and, when necessary, imaging tests.
