Brief overview of depression and schizophrenia as significant mental health disorders
Here’s a short description of schizophrenia and depression two of the most significant mental health conditions:

Defined: Depression, clinically called MDD, or Major Depression Disorder (MDD) is a disorder of the mood characterized by constant feelings of despair, sadness, and an absence of enjoyment or interest during daily routine activities.
The prevalence: Depression has been identified as among the top frequent mental health issues in the world. As per the World Health Organization (WHO), there are more than 265 million people, of all ages, are suffering from depression worldwide.
The impact: It can significantly hinder an individual’s ability to perform at work, school, and in social situations. Depression can be a trigger for suicidal ideas and actions which makes it a major factor in disability across the globe.
The most important features: Symptoms may include an increase in energy levels and changes in appetite, insomnia, feelings of feeling of worthlessness, and trouble in concentrating. Everyone feels depressed or sad at times, depression can be characterized by prolonged periods (typically 2 weeks or more) of these signs.
Schizophrenia:
Defined: Schizophrenia is a grave mental disorder that impacts the way a person thinks, experiences, and behaves. It manifests itself as mental distortions, impairments of perception of emotions and language, self-esteem, and behavior.
Incidence: Schizophrenia is the cause of one percent of the population. It is most often seen during late adolescence, or the early years of adulthood. It is likely to be present throughout life.
The impact: Schizophrenia can lead to a significant disability that can affect everyday functioning. People with schizophrenia may face issues in relationships, employment as well as independent living. Because of misconceptions about the condition the stigma they face is often a source of discrimination.
The most important features: Symptoms are typically classified into three groups Positive symptoms (hallucinations or delusions, as well as thought disorders) and adverse manifestations (lack in emotion diminished emotions, decreased speaking) and cognitive symptoms (impaired memory, issues with attention difficulties in making decisions).
Both schizophrenia and depression are complicated conditions that are affected by a variety of biological, genetic, and environmental elements. A timely diagnosis and a proper treatment can enhance the outcome for patients suffering from either.
Depression and Schizophrenia in the comparison chart
A comparison chart is a concise way to understand the differences and similarities between depression and schizophrenia.
Here’s a comparative breakdown in chart form:
Comparison Chart: Depression vs. Schizophrenia
| Criteria | Depression | Schizophrenia |
|---|---|---|
| Definition | A mood disorder with persistent sadness, hopelessness, and lack of interest. | A severe mental disorder with distorted thinking, perceptions, and emotions. |
| Primary Symptoms | – Persistent sadness – Loss of interest – Fatigue – Sleep disturbances – Feelings of worthlessness – Thoughts of death or suicide |
– Hallucinations (often auditory) – Delusions – Disorganized thinking and speech – Blunted emotions – Social withdrawal |
| Onset | Can occur at any age, often in late adolescence or early adulthood. | Symptoms typically surface between late adolescence and early adulthood. |
| Causes | Combination of: – Biological – Genetic – Environmental – Psychological |
Combination of: – Genetic – Brain abnormalities – Neurochemical imbalances – Environmental factors |
| Treatment | – Antidepressant medications – Psychotherapy (e.g., CBT) – Lifestyle modifications – Electroconvulsive therapy (in severe cases) |
– Antipsychotic medications – Psychotherapy – Social and vocational skills training – Family support |
| Duration | Episodes can be short-term or recurrent throughout life. | Typically a chronic condition, but symptoms can be managed with treatment. |
| Prevalence | More than 264 million people are affected worldwide. | Affects about 1% of the global population. |
| Complications if Untreated | – Chronic pain – Substance abuse – Increased risk of suicide |
– Difficulty in social and occupational functioning – Increased risk of suicide – Health issues due to neglect |
Importance of understanding the differences
Understanding the difference between schizophrenia and depression is crucial for a variety of reasons, such as:
Accurate Diagnosis:
-
- It is crucial to distinguish between the symptoms of schizophrenia and depression is essential for making an appropriate diagnosis.
Effective Treatment:
-
- The two disorders have distinct treatment strategies. Antidepressants are the most common method of therapy for depressive disorders, they are also the primary treatment option for schizophrenia. Utilizing the wrong treatment approach can cause a worsening of symptoms or undesirable negative side consequences.
Reducing Stigma:
-
- Mental health issues are frequently ignored, leading to stigmatization. When we understand the unique aspects of each disorder it is possible to promote more compassionate and educated views by reducing misperceptions and prejudices.
Support Systems:
-
- Family members and caregivers require different options and strategies for coping based on the specific condition. For instance, assisting those suffering from schizophrenia who experience hallucinations is a different strategy than caring for someone suffering from depressive episodes.
Public Health and Policy:
-
- Understanding the difference aids policymakers in distributing resources efficiently. For instance, the infrastructure requirements of a Depression Helpline could differ from a crisis center that is designed for those who suffer from severe schizophrenic episodes.
Research Purposes:
-
- In the field of research into mental health, it is crucial to identify disorders accurately in order to research their causes, impact, and treatment options effectively.
Personal Empowerment:
-
- For those who are suffering from symptoms, knowing the subtleties between ailments can allow individuals to seek the appropriate assistance in order to advocate for their well-being.
Prevention and Early Intervention:
-
- Being aware of the early signs of each disorder may help in timely interventions that can enhance the long-term outcome. For instance, the early signs of schizophrenia, like the withdrawal of social interaction or strange beliefs are distinct from typical symptoms of depression.
Education:
-
- People working in different areas from teachers to employers benefit by knowing these differences in order to be able to accommodate and help people who are affected by these issues in diverse environments.
Safety:
- Certain signs, such as suicidal ideas in depression, or extreme schizophrenia-related delusions, may present safety hazards. Recognizing these specific symptoms will ensure that patients receive the needed safeguards and treatments.
The distinction between schizophrenia and depression isn’t just a simple academic test. It is a major issue for the treatment of patients, social perceptions, policies as well as the overall health of millions of people around the world.
Primary Symptoms of Depression and Schizophrenia
Both disorders have distinct symptoms of schizophrenia. Here’s the breakdown:
Depression (Major Depressive Disorder):
- Persistent Sadness: Persistent feelings of sadness that are prevalent in all aspects of our lives.
- Anhedonia: A reduced or total lack of enthusiasm for things that used to be fun.
- Fatigue: Feeling of fatigue or fatigue even if one has received enough sleep.
- Sleep disturbances: This could manifest as insomnia (difficulty getting or staying at night) and excessive sleepiness (excessive sleep).
- Food and weight changes: It could be increased or decreased appetite which can lead to weight loss or gain.
- Feelings of Inadequacy or excessive guilt: Persistent feelings of guilt or inadequacy over perceived errors or shortcomings.
- Trouble Concentrating: Problems focusing on things or making decisions.
- Psychomotor Retardation or Agitation: It could be restlessness (pacing or hand-wringing) or slowing of speech and movements.
Schizophrenia:
- hallucinations: Feeling that things do not exist. The most frequent form is hearing voices (auditory hallucinations) however hallucinations could be experienced through any sense.
- Delusions: Strongly held false belief systems that aren’t based on reality. For instance, the belief that someone has special powers or that forces from outside control one’s thoughts.
- Unorganized Thoughts: The symptoms can include rambling or disjointed speech. The thoughts may be scattered or unlogical.
- Disordered or Abnormal Motor Behavior: It can vary from catatonia to agitation. It can manifest as unpredictability in behavior, inability to respond, or postures that are not correct.
- Negative symptoms: This refers to the loss or lack of capabilities. Examples include:
-
- Affective Flattening: A reduction in emotional expression by vocal tone, facial expression, or gestures.
- Analogia: Speech content or reduced speech production.
- Anhedonia: Decreased ability to feel pleasure.
- Asociality The social world is less interesting.
- The Avolition: Reduced desire to start meaningful actions.
While they are primary symptoms, their presentation may differ significantly among individuals. Furthermore, even though certain symptoms may overlap (e.g. anhedonia, for instance) the background, symptoms that accompany them, and the overall picture of the patient will aid in identifying the different conditions.
Causes and Risk Factors of Depression and Schizophrenia
The causes behind schizophrenia and depression aren’t completely understood, however, both are believed to stem from a mix of biological, genetic as well as environmental elements.
Here’s a list of well-known risks and causes for each
Depression (Major Depressive Disorder):
Biological Factors:
-
- Neurotransmitter imbalances: Serotonin, norepinephrine, and dopamine are neurotransmitters that play an important function in the regulation of mood and imbalances may contribute to depression.
- Hormonal Imbalances: changes in the hormonal balance in the body for example, during menopausal, pregnancy or thyroid issues, can be a cause of depression.
Genetic Predisposition:
-
- People with a family background of depressive disorders are at greater risk of developing depression, which suggests that there is a genetic factor.
Environmental Triggers:
-
- Chronic stress, traumatizing events as well as childhood trauma, and other major life events can cause the onset of depression.
Psychological Factors:
-
- People who are more susceptible to despair lack self-esteem or tend to be stressed may be at a higher risk.
Medical Conditions:
-
- Chronic illnesses such as diabetes, chronic pain, or cardiovascular diseases can increase the likelihood of developing depression.
Substance Abuse:
-
- The use of alcohol or dependence on other drugs could make it more likely for depression to develop.
Schizophrenia:
Genetic Factors:
-
- If you have a family member suffering from schizophrenia is a risk factor for being diagnosed with the condition. Certain genes are thought to be responsible, however, there is no one gene that is believed to be responsible.
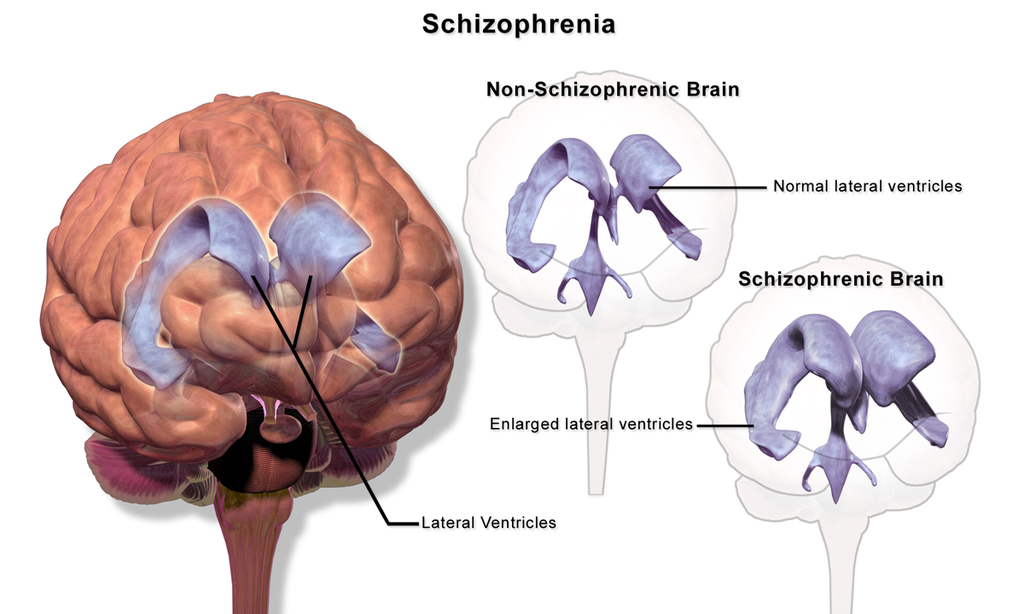
Brain Structure Abnormalities:
-
- Certain studies reveal changes in the shape of specific brain regions, or in their connections in those suffering from schizophrenia.
Neurochemical Imbalances:
-
- Unbalances in neurotransmitters, such as glutamate and dopamine could be a contributing factor to schizophrenia.
Pregnancy and Birth Complications:
-
- Things like malnutrition in birth, early labor, or a low birth weight that is low could increase the chance of schizophrenia in the offspring.
Environmental Factors:
-
- Stressful circumstances and exposure to viruses or malnutrition prior to birth, or psychological factors can cause or worsen symptoms in people who are vulnerable.
Drug Abuse:
-
- Consumption of certain substances, particularly in teen years or early adulthood, may increase the risk of developing schizophrenia. The use of marijuana as well as LSD have been associated with the growth of schizophrenia in people who are predisposed.
Although these variables provide information about the possible causes and dangers, however, it’s important to understand that the causes of any condition in a particular individual could be multifaceted and distinct. Additionally, the presence of any one or more of the risk factors doesn’t mean that someone will develop schizophrenia or depression It simply increases the risk.
Can you have schizophrenia and depression?
A person can be diagnosed with both depression and schizophrenia at the same time. When someone who has schizophrenia suffers symptoms of major depression disorder, it is usually described as “schizoaffective disorder” or, more specifically, “depressive episodes” or “depressive episodes” within the context of schizophrenia.
Here’s a more detailed review of this cross-over:
Schizoaffective Disorder:
Schizophective disorders are a psychological issue that is characterized by a mixture of schizophrenia-related symptoms like hallucinations or delusions, as well as mood disorder symptoms, which can be manic or depressive. There are two kinds of schizoaffective disorder.
- Bipolar kind: This type includes periods of mania, and occasionally major depression.
- Type of depression: This type includes only major depressive episodes.
In order to be diagnosed as a schizophrenia-related schizoaffective disorder, both symptoms of schizophrenia, as well as major mood episodes (depression or manic), are required to be present in a significant proportion of the disorder.
Depressive Episode in Schizophrenia:
In addition to schizoaffective disorders and schizoaffective disorder, it is also common for those suffering from schizophrenia to suffer from episodes of depression. Depression symptoms could be an integral part of schizophrenia, a consequence of the psychological stressors and problems caused by the illness or as an adverse effect of certain antipsychotic medication.
Importance of Identification and Treatment:
Recognizing and treating symptoms of depression for people suffering from schizophrenia is vital for many reasons:
- Suicide risk: Individuals with schizophrenia who are also depressed are more at the chance of committing suicide.
- functional impairment: A combination of depression and other disorders can also affect everyday functioning, making chores as well as social interactions more difficult.
- Qualities of life: Addressing and managing depression symptoms can greatly enhance the quality of life of those suffering from schizophrenia.
Treatment usually involves a mix of antipsychotic drugs and antidepressants. Psychotherapy and psychosocial interventions may also play an important role in the treatment of both disorders.
It is possible for a person to be affected by both depression and schizophrenia, and it’s crucial for therapists to be aware of and address both types of symptoms in order to improve treatment outcomes.
Treatment Options for Depression and Schizophrenia
Treatment for schizophrenia and depression differs in significant ways due to the unique features and signs of each. Both conditions typically are treated with a combination of psychotherapy, medication, and other therapies.
Here’s a list of the most frequently used treatments for each of the following:
Depression (Major Depressive Disorder):
Antidepressant Medications:
-
- Examples include Selective Serotonin Reuptake Inhibitors (SSRIs) like fluoxetine (Prozac) and citalopram (Celexa), and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) like venlafaxine (Effexor XR) and duloxetine (Cymbalta).
Psychotherapy:
-
- CBT: Cognitive Behavior Therapy (CBT): Focuses on the identification and challenge of negative thinking patterns and behavior.
- Interpersonal Therapy (IPT): Addresses interpersonal issues and assists in improving communication abilities.
- Problem-Solving Therapy: The therapy helps individuals build the skills to deal with and solve problems in their lives.
Electroconvulsive Therapy (ECT):
-
- A common treatment for severe depression that isn’t responding to other treatments. It involves transferring electrical signals through the brain, triggering the brain to experience brief seizures.
Repetitive Transcranial Magnetic Stimulation (rTMS):
-
- Utilizes magnetic fields to stimulate neurons in the brain. This helps to reduce depression symptoms.
Lifestyle and Home Remedies:
-
- Regular fitness, a healthy diet, staying away from drinking, and using methods for reducing stress are a good complement to the medical treatment.
Support Groups:
-
- Sharing your experiences and feelings can be an effective part of treatment.
Schizophrenia:
Antipsychotic Medications:
-
- These are the most common methods of treatment that help to control delusions, hallucinations, and disordered thinking. Some examples include risperidone (Risperdal), olanzapine (Zyprexa) as well as clozapine (Clozaril).
Psychotherapy:
-
- Individual Therapy: Patients are taught how to manage stress and to recognize early warning symptoms of the possibility of relapse.
- Cognitive Behavioral Therapy (CBT): Can assist in addressing specific issues such as hallucinations or delusions of thought.
- Family Therapy: Family Therapy educates parents about their condition and assists them in helping their loved ones.
Social Skills Training:
-
- It focuses on improving social interaction and communication.
Vocational Rehabilitation and Supported Employment:
-
- Assists people suffering from schizophrenia in preparing for, locating, and holding jobs.
Hospitalization:
-
- In the event of a crisis or a severe episode the need for hospitalization is often necessary to ensure security, adequate nutrition, sufficient sleep and basic hygiene.
Assertive Community Treatment (ACT):
-
- This requires the use of a team-based approach for intensive case management for those who require assistance on a regular basis.
It is important to note that people suffering from any of the conditions may need to test various treatments and combinations in order to discover the best treatment for their particular situation. Additionally, the earlier detection, as well as intervention, could greatly improve the chances of recovery for both schizophrenia and depression. Regular check-ups with health professionals and adherence to treatment protocols prescribed by doctors are vital to managing both disorders successfully.
Misconceptions and Myths
Both schizophrenia and depression are complex mental health issues that have been covered by many myths and misconceptions. A discussion of these issues can help to create an understanding of the condition and decrease the stigma that surrounds these illnesses.
Depression (Major Depressive Disorder):
“It’s just sadness. “
-
- Real: Depression is more than being sad. It’s a long-lasting and complex mood disorder that affects feelings, thoughts physical health, as well as everyday functioning.
“You can just snap out of it. “
-
- Realities: Depression isn’t an option or a sign of weakness. It’s a medical issue that usually requires long-term care and care.
“Only women get depressed. “
-
- Real: While depression may be more frequently diagnosed for women, men too suffer from it, even though they may experience or cope with their depression in different ways.
“Antidepressants will change your personality. “
-
- Real: Antidepressants aim to restore brain chemistry and ease symptoms but do not alter the person’s personality.
“Talking about depression makes it worse. “
-
- Realism: Talking about depression is therapeutic and crucial in the process of recovery. Communication that is open can offer assistance, understanding, and possible solutions.
Schizophrenia:
“People with schizophrenia have multiple personalities. “
-
- Real: Schizophrenia is a condition of psychosis that causes that there is a change in thought and perception. It’s not as common as Dissociative Disorder. Disorder (formerly also known as Multiple personality disorders).
“All individuals with schizophrenia are violent or dangerous. “
-
- Real: While some people who suffer from schizophrenia may exhibit aggressive behavior, most often during episodes of acute onset, however, the majority of them aren’t violent. The people who suffer from schizophrenia tend to be victims rather than violent perpetrators.
“Schizophrenia only involves hallucinations. “
-
- Real: Hallucinations are just one of the possible symptoms. Other symptoms include delusions, poor thoughts, negative symptoms, and cognitive impairments.
“Schizophrenia is caused by bad parenting or personal failures. “
-
- Realism: Schizophrenia is a complex disorder that has biological, genetic, and environmental triggers playing a part in its development. It’s not a result of individual weaknesses or adolescence.
“People with schizophrenia can’t lead normal lives. “
-
- Realities: With the right care and support, a large number of people with schizophrenia enjoy fulfilling lives, build jobs, and keep relationships. The extent and severity of the disorder varies among people.
Refuting these myths and misconceptions is vital to increasing compassion, understanding, and a proper support system for people suffering from schizophrenia or depression.
Conclusion
Schizophrenia and depression a distinct sets of mental issues with distinct symptoms that require specialized treatment. The dispelling of myths and misinformation about the two disorders is vital to fostering understanding and compassion. A proper education and awareness program will result in better care and better outcomes for those who are affected.
