Overview of Biopsy and Pap Smear
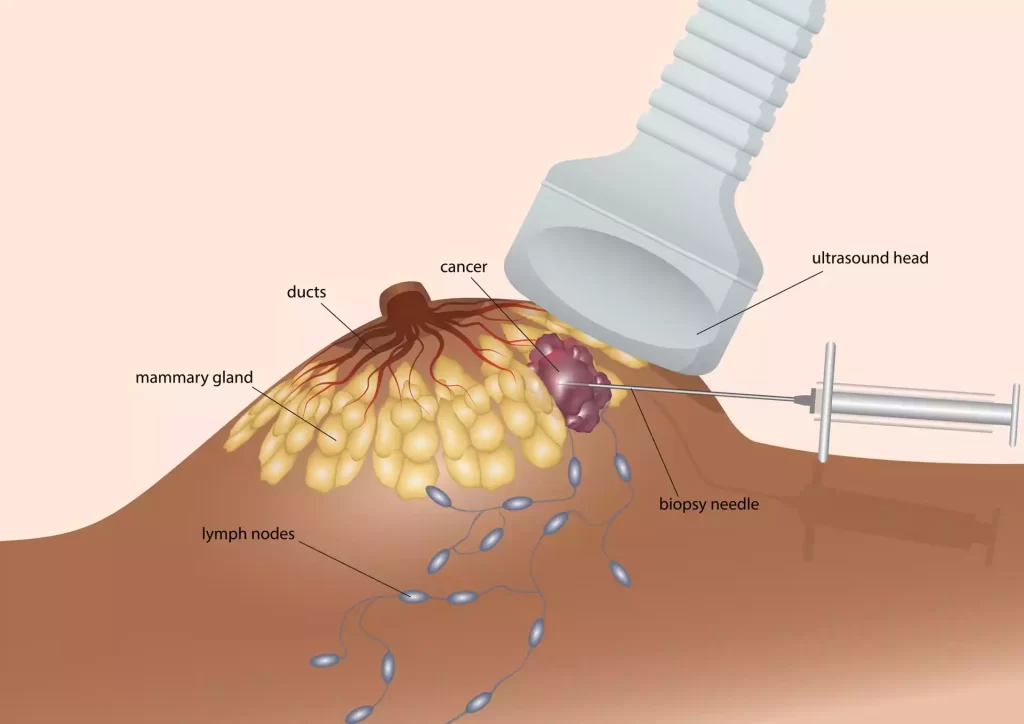
A biopsy is a medical procedure that involves the removal of tissue or cells from the body, which is then examined under a microscope. This is done to determine the presence, cause, or extent of a disease, especially cancer. Biopsies can be performed on almost any part of the body and are the most definitive way to diagnose or rule out cancer. Depending on the location and nature of the suspected disease, there are various types of biopsies, such as needle biopsy, incisional biopsy, and excisional biopsy.
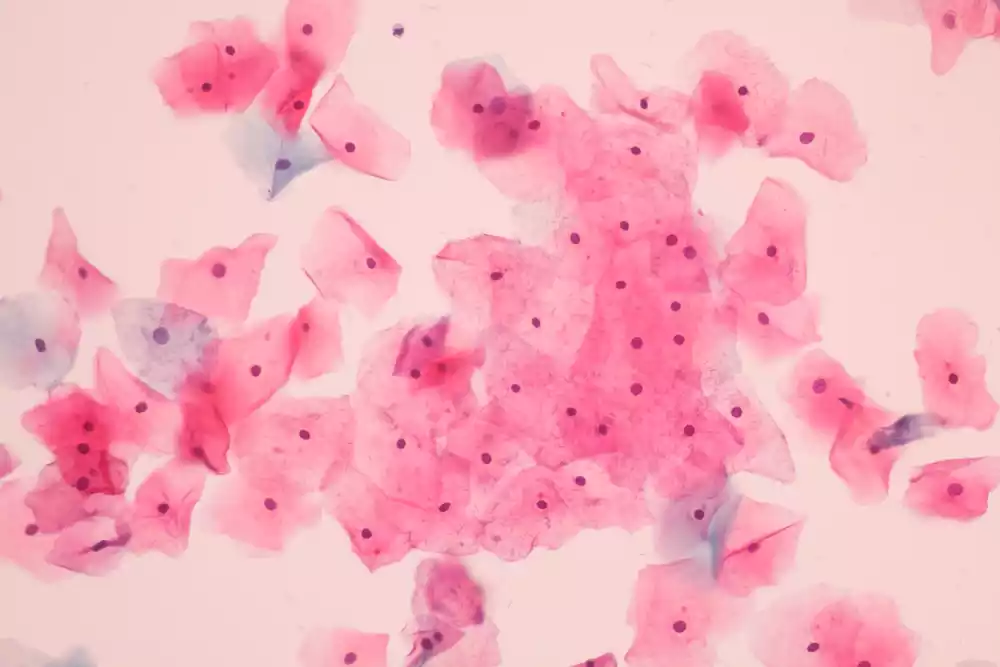
A Pap smear, or Pap test, is a screening procedure for cervical cancer. It is the process of collecting cell from the cervical region. which is the lower portion of the uterus which connects with vagina. This test is specifically designed to identify precancerous or cancerous changes in the cervical cells, often caused by persistent human papillomavirus (HPV) infection.
Brief overview of medical diagnostic tests
Medical Diagnostic Tests: A Brief Overview
Medical diagnostic tests are procedures used by healthcare professionals to detect, diagnose, and monitor diseases, conditions, and infections. They play a crucial role in helping doctors determine the right treatment for patients.
Here’s a concise overview
- Purpose of Diagnostic Tests:
-
- Detection: Identify the presence of a disease or condition, often before symptoms appear.
- Diagnosis: Determine the exact nature and cause of an illness, based on the symptoms presented and the results of the tests.
- Monitoring: Track the progress of a disease or condition over time and evaluate the efficacy of treatments.
- Types of Diagnostic Tests:
-
- Laboratory Tests: These include blood tests, urinalysis, and cultures where samples are analyzed in a laboratory. Examples are complete blood count (CBC), blood glucose testing, and throat cultures.
- Radiologic Imaging: This includes X-rays, CT scans, MRI scans, and ultrasounds. These tests provide images of the inside of the body, allowing physicians to visualize structures and possible abnormalities.
- Functional and Stress Tests: Used mostly in cardiology, these tests evaluate the function of the heart and other organs under stress. The treadmill stress test is a popular example.
- Endoscopy: This involves inserting a camera into the body to directly view certain areas, like the digestive tract in a colonoscopy or the bronchi in a bronchoscopy.
- Biopsy: A procedure where a small sample of tissue is taken from the body to be examined under a microscope. This is often done to diagnose cancers.
- Genetic Testing: Used to identify changes in DNA that could indicate genetic disorders or predisposition to certain diseases.
- Specialized Scans: Such as PET scans, can help detect areas of the body affected by conditions like cancer, heart disease, and neurological disorders.
- Interpreting Results:
-
- Results can be quantitative (giving a specific measurable number), qualitative (providing a positive or negative result), or descriptive (like the findings of an imaging study).
- Reference ranges are often used in lab tests to determine what’s considered “normal.” However, what’s normal for one person might not be for another, so context and clinical judgment are essential.
- Benefits and Risks:
-
- Benefits: Early detection and diagnosis, informed medical decisions, personalized treatment plans, and monitoring of disease progression or treatment efficacy.
- Risks: Vary depending on the test. Some tests might expose patients to radiation, while others could pose risks of infection or complications.
- Conclusion: Diagnostic tests are foundational in modern medicine, offering invaluable insights into patient health. While they provide crucial data for decision-making, clinical judgment, patient history, and other diagnostic information are also vital components of comprehensive healthcare.
While diagnostic tests are tools to guide decisions, the dialogue between healthcare providers and patients is essential for understanding and interpreting these results in the context of individual health needs.
Importance of early detection in medical conditions
Early detection of medical conditions, especially chronic diseases and cancers, is a pivotal aspect of modern medicine.
Detecting diseases at an early stage can lead to better outcomes for patients in various ways:
- Improved Prognosis and Survival Rates:
-
- Many medical conditions, particularly certain types of cancer, have significantly higher survival rates when detected early. For instance, early detection of breast cancer or melanoma can lead to treatments that are more effective, leading to increased chances of survival.
- Less Aggressive Treatments:
-
- Early-stage diseases often require less aggressive treatments than advanced-stage diseases. Patients might benefit from simpler surgeries (lumpectomy instead of mastectomy for breast cancer, for example), or they might avoid chemotherapy or radiation in certain scenarios.
- Cost-effective Care:
-
- Treating a disease in its early stages often proves less costly in the long run compared to the extended care required for advanced-stage diseases, which might need more intensive treatments, prolonged hospital stays, or long-term care.
- Prevention of Complications:
-
- Early detection can prevent the progression of diseases that can lead to complications. For instance, controlling diabetes in its early stages can prevent or delay complications like neuropathy, retinopathy, or cardiovascular diseases.
- Limiting Disease Spread:
-
- In the context of infectious diseases, early detection can lead to timely interventions that prevent the spread of the disease to others, aiding in controlling potential outbreaks.
- Better Quality of Life:
-
- Early detection and intervention can lead to better disease management, preserving the patient’s quality of life. It can prevent or reduce symptoms, physical limitations, or the need for palliative care.
- Increased Awareness and Behavioral Change:
-
- Detecting risk factors early, like high blood pressure or cholesterol, can lead to lifestyle and behavioral changes that can prevent the onset of diseases.
- Psychological Benefits:
-
- Knowing about a condition early can reduce the anxiety and uncertainty of unexplained symptoms. While a diagnosis might bring its own set of worries, early detection allows for proactive planning and coping strategies.
- Facilitation of Research:
-
- When diseases are detected early, it provides researchers with valuable data about the initial stages of the disease, enabling them to study its natural progression and develop more effective interventions.
- Public Health Implications:
- On a broader scale, early detection can lead to reduced morbidity and mortality rates in populations, leading to a healthier society. Public health campaigns that promote early screening, like mammograms or colonoscopies, play an essential role in this.
Early detection is a cornerstone of preventive medicine. It empowers patients and healthcare providers to take timely and effective actions, leading to improved health outcomes, reduced healthcare costs, and overall better quality of life. Regular check-ups, awareness campaigns, and access to screening tests are vital tools in achieving these benefits.
What is Biopsy?
A biopsy is a medical procedure that involves the removal of a small sample of tissue or cells from the body for examination under a microscope. It’s a diagnostic test primarily used to determine the presence, cause, or extent of a disease, especially cancer.
Here’s a detailed breakdown:
- Purpose of a Biopsy:
-
- Diagnosis: A biopsy can confirm or rule out whether a suspicious area might be cancerous or determine the nature of an unidentified lump.
- Type and Grade: In cases of cancer, a biopsy can help determine its type (e.g., adenocarcinoma, squamous cell carcinoma) and its grade (how abnormal the cells look and how quickly they are likely to grow and spread).
- Other Diseases: Biopsies are not limited to diagnosing cancer. They can also identify other conditions like infections or inflammatory and autoimmune disorders.
- Types of Biopsies:
-
- Needle Biopsy: A needle is used to remove a sample of tissue or fluid. This includes fine-needle aspiration (FNA) and core needle biopsy.
- Incisional Biopsy: A small cut is made in the skin, and a part of the suspicious area is removed.
- Excisional Biopsy: The entire lump or suspicious area is removed, often including a small amount of surrounding tissue.
- Endoscopic Biopsy: Using an endoscope (a flexible tube with a light and camera), tissue samples can be taken from the stomach, colon, or lung, among other areas.
- Punch Biopsy: A special tool removes a circular section of skin, often used to diagnose skin conditions.
- Bone Marrow Biopsy: A sample of bone marrow, usually from the hip bone, is removed to diagnose blood disorders like leukemia or lymphoma.
- Surgical Biopsy: Conducted during a surgical procedure, usually when a needle biopsy is inconclusive or can’t be used.
- Procedure:
-
- The exact procedure varies based on the type of biopsy. Most biopsies involve using a needle, scalpel, or other tool to remove a small amount of tissue.
- The area is usually numbed with a local anesthetic, although general anesthesia might be used for more extensive biopsies.
- Risks and Recovery:
-
- While generally considered safe, biopsies can pose some risks, including infection, bleeding, or bruising at the biopsy site.
- Recovery is typically quick, especially for non-surgical biopsies. Some soreness or pain might be experienced at the biopsy site.
- Results Interpretation:
-
- The results can confirm whether the cells are benign (non-cancerous), precancerous, or malignant (cancerous). The findings can also provide information about the cell’s origin, type, and other characteristics.
A biopsy is a vital diagnostic tool that provides definitive evidence of the presence or absence of disease, guiding subsequent medical decisions and treatment plans. If a biopsy is recommended, it’s crucial to discuss any concerns or questions with the healthcare provider to understand its significance and implications.
What is Pap Smear?
A Pap smear, also known as a Pap test, is a medical procedure used primarily to screen for cervical cancer in women. It involves collecting cells from the cervix, the lower, narrow end of the uterus that connects to the vagina.
Here’s a detailed overview:
- Purpose of a Pap Smear:
-
- Cervical Cancer Screening: The primary aim is to detect abnormal cells that might indicate cervical cancer or its precursors.
- Human Papillomavirus (HPV) Detection: Some Pap tests can also identify infection with certain high-risk types of HPV, a virus that can cause cervical cancer.
- Procedure:
-
- During a pelvic examination, a doctor or nurse inserts a speculum into the vagina to widen it and access the cervix.
- A soft brush or spatula is used to gently scrape off cells from the cervix.
- The collected cells are then preserved in a solution and sent to a laboratory for examination under a microscope.
- Results Interpretation:
-
- Normal (Negative): No abnormal cells were detected.
- Abnormal (Positive): Abnormal cells were found. Depending on the type and extent of abnormalities, further tests or procedures may be recommended. Common classifications of abnormal results include Atypical Squamous Cells of Undetermined Significance (ASC-US), Low-Grade Squamous Intraepithelial Lesions (LSIL), and High-Grade Squamous Intraepithelial Lesions (HSIL).
- Follow-Up and Further Testing:
-
- Depending on the results, a woman might be asked to return for another Pap test in a few months, undergo an HPV test, or have a colposcopy (a procedure to closely examine the cervix, vagina, and vulva for signs of disease).
- If high-grade changes or suspicious areas are found during colposcopy, a biopsy of the cervix might be performed.
- Frequency of Screening:
-
- Recommendations for the frequency of Pap tests vary based on age, medical history, and prior test results. Generally:
-
-
- Women aged 21-29: Every 3 years.
- Women aged 30-65: Every 3 years or every 5 years if combined with an HPV test.
-
-
- Women over 65 or those who’ve had a hysterectomy (with the cervix removed) and have no history of cervical dysplasia or cancer may not need regular Pap smears.
- Benefits and Limitations:
-
- Benefits: Pap smears have significantly reduced the incidence and mortality of cervical cancer in countries where regular screening is conducted. Early detection allows for timely and effective interventions.
- Limitations: While highly beneficial, Pap tests are not infallible. There might be false negatives (abnormal cells are present, but the test doesn’t detect them) or false positives (the test indicates abnormal cells, but they aren’t of concern).
A Pap smear is a vital screening tool in women’s healthcare, playing a significant role in reducing cervical cancer’s morbidity and mortality. Regular screenings and follow-up are crucial components of preventative care, ensuring early detection and intervention when necessary.
Biopsy and Pap Smear in the comparison chart
Biopsy vs. Pap Smear Comparison Chart
| Criteria | Biopsy | Pap Smear |
|---|---|---|
| Definition | A medical test involves the extraction of sample cells or tissues for examination to determine the presence or extent of a disease. | A procedure to test for cervical cancer in women involves the collection of cells from the cervix. |
| Primary Purpose | Diagnosis of various diseases, especially cancer, by studying tissue samples. | Screening for cervical cancer and pre-cancerous changes. |
| Procedure | Depends on the type: needle, incisional, excisional, etc. Generally involves the removal of tissue for lab analysis. | A swab or brush is used to collect cells from the cervix, which are then spread on a microscope slide or in a liquid solution for examination. |
| Indications | Suspicion of cancer, infections, or inflammatory conditions in various body parts. | Primarily for women, especially those aged 21-65, to screen for cervical abnormalities. |
| Frequency | Usually done once, unless further examination or repeated sampling is required. | Typically recommended every 3 years for women aged 21-29 and every 5 years (with HPV testing) for women aged 30-65, unless otherwise indicated. |
| Benefits | Accurate and definitive diagnosis. Allows for targeted treatment. | Early detection of cervical cancer, reducing mortality. |
| Limitations/Risks | Invasive. Risk of infection, bleeding, or other complications. May not always capture the diseased area. | Might not detect all cervical cancers (false negatives). Possibility of false positives leading to unnecessary treatments. Does not screen for other gynecological cancers. |
| Recovery Time | Varies. Some biopsies may require stitches and a few days of recovery. | Minimal to none. Some women might experience light spotting or discomfort briefly after the test. |
| Result Timeframe | Generally takes a few days to a couple of weeks, depending on the type and complexity. | Usually within a week to a few weeks. |
| Follow-Up | Based on biopsy results. Treatment, further testing, or monitoring may be recommended. | If abnormal cells are found, further tests (like colposcopy or a biopsy) may be necessary. |
What are the similarities between Biopsy and Pap Smear?
While biopsies and Pap smears are distinct procedures with their own specific indications and methodologies, they share several similarities in terms of their role in medical diagnostics:
- Diagnostic Purpose:
-
- Both procedures are primarily used to detect and diagnose diseases. While biopsies can be used for various conditions, including many types of cancers, Pap smears are primarily for detecting cervical abnormalities that could lead to cancer.
- Cellular Examination:
-
- Both involve collecting cells or tissues that are then examined under a microscope by a pathologist.
- Early Detection:
-
- Both procedures are crucial for early detection. Early diagnosis can lead to better outcomes and less aggressive treatments.
- Procedure in a Clinical Setting:
-
- Both biopsies and Pap smears are typically performed in a clinical setting, such as a doctor’s office, clinic, or hospital.
- Guidance for Treatment:
-
- The results from both tests can guide further medical decisions, including the need for more detailed investigations, treatment plans, or surgical interventions.
- Potential for Abnormal Findings:
-
- Both tests aim to identify abnormalities. In the case of the Pap smear, it’s specifically about cervical cell abnormalities, while biopsies can detect abnormalities in any tissue they’re taken from.
- Follow-Up Procedures:
-
- Both may require follow-up procedures or tests based on their results. For instance, an abnormal Pap smear might lead to a colposcopy, while certain biopsy results might necessitate further surgical intervention.
- Invasive Nature:
-
- Though the degree varies, both procedures are invasive to some extent. A Pap smear involves scraping cells from the cervix, while a biopsy involves the removal of tissue, whether through a needle or surgical procedure.
Both biopsies and Pap smears are integral tools in the realm of medical diagnostics. They serve as foundational methods for clinicians to understand, diagnose, and subsequently treat potential health concerns.
Limitations and Risks
Biopsy:
- False Negatives: Sometimes, the sample taken might not capture the affected cells, leading to a false-negative result.
- Infection: Any invasive procedure poses a risk of infection. While generally minimal, there’s a chance of introducing infection into the biopsy site.
- Bleeding and Bruising: Particularly in cases where larger samples are taken, bleeding or bruising might occur.
- Scarring: Some biopsy procedures might lead to scarring, especially if a larger incision is required.
Pap Smear:
- False Negatives: Not all abnormal cells are detected in every test, which means cancer or precancerous cells might sometimes be missed.
- False Positives: Conversely, a test might suggest abnormalities when none exist, leading to unnecessary stress and additional procedures.
- Discomfort: While generally painless, some women might experience discomfort during the procedure.
Frequency and Follow-up
Biopsy: Frequency largely depends on the nature and location of the suspected disease, the patient’s medical history, and the results of previous biopsies or tests. For instance:
- Those with certain skin conditions might need regular skin biopsies.
- Patients with chronic liver diseases might require periodic liver biopsies.
Follow-up:
- After a biopsy, the results dictate the next steps. If malignant cells are detected, a treatment plan is developed, which could include surgery, radiation, chemotherapy, or a combination thereof.
- In non-cancerous findings, the patient might need regular monitoring to ensure no malignant changes occur over time.
Pap Smear: Frequency:
- Women aged 30-65 are recommended to have a Pap smear every 3 years or every 5 years if combined with an HPV test.
- Women over 65, or those who’ve had a hysterectomy (with the cervix removed) and have no history of cervical dysplasia or cancer, may no longer need regular Pap smears.
Follow-up:
- If the Pap smear results are abnormal, the patient might need a repeat Pap smear, an HPV test, or a more detailed examination called a colposcopy.
- In more severe cases, a cervical biopsy might be conducted during the colposcopy to ascertain the extent and nature of the abnormality.
Conclusion
Both biopsies and Pap smears are quintessential tools in the medical diagnostic toolkit. While biopsies offer a broader diagnostic spectrum suitable for various body parts and conditions, Pap smears are specialized tests focusing on cervical cancer and its precursors. Understanding their distinctions, limitations, and follow-up procedures is crucial for both medical practitioners and patients.
Early detection remains a cornerstone in the management and treatment of many diseases, particularly cancer. Regular screenings, be it through biopsies or Pap smears, empower patients with knowledge and offer a fighting chance against potential ailments. As medicine continues to evolve, these diagnostic tools serve as foundational pillars, reinforcing the age-old adage – that prevention is better than cure.
