Definition of Hydatidiform Moles and Choriocarcinoma
Definitions of hydatidiform mole and choriocarcinoma:
Hydatidiform Mole:
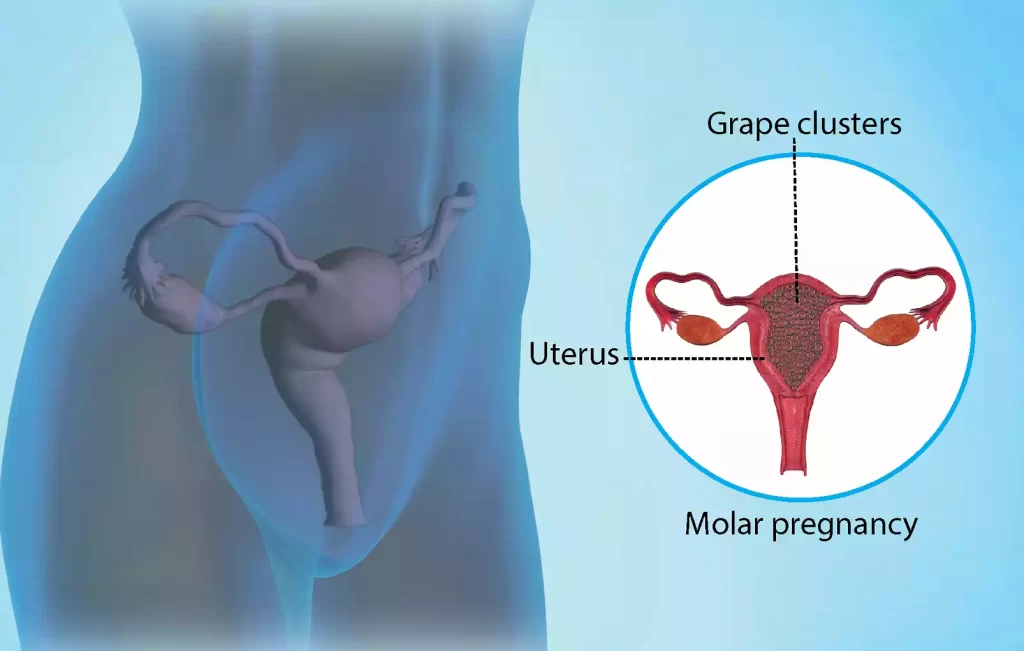
The hydatidiform mole, or molar pregnancy as it is also called, is a rare pregnancy abnormality in which an unfertilized egg implants into the uterus, and grows to become a mass of abnormal tissue, instead of a normal fetus.
There is a difference between two types of hydatidiform moles:
Complete hydatidiform mole: This type involves fertilization by an egg, either by an empty sperm without genetic material or by two sperm. The result is an abnormal mass of cells with no fetal development.
Partial hydatidiform mole: When a regular egg or sperm is fertilized with two sperms, or by a single sperm which duplicates the genetic material of an egg. It is characterized by abnormal tissue in the placenta and some fetal growth.
Untreated hydatidiform lesions can lead to complications during early pregnancy and elevated levels of the hormone human chorionic gonadotropin (hCG), which is produced in pregnancy. Untreated, a mole that is hydatidiform can develop into a choriocarcinoma.
Choriocarcinoma:
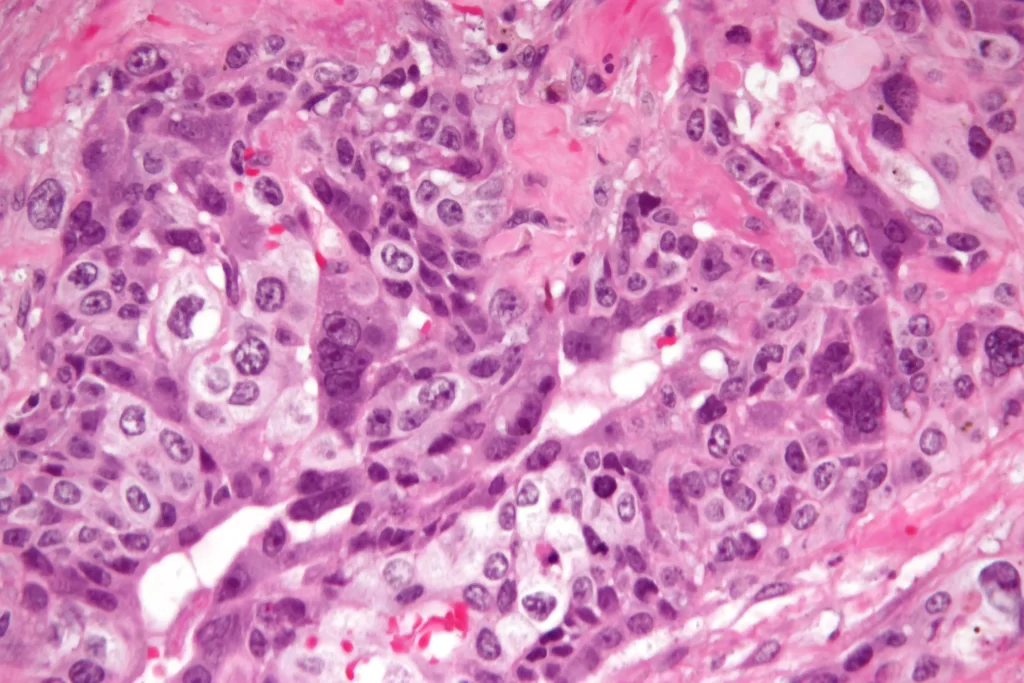
Choriocarcinoma, a form of cancer with a high malignant potential, is caused by trophoblastic (placental) cells. The choriocarcinoma is not a hydatidiform mole. It occurs instead when trophoblastic (tissue-forming) cells turn cancerous and rapidly grow.
The key characteristics of choriocarcinoma are:
Rapid metastasis: Choriocarcinoma is prone to spreading to other organs. This includes the liver, lungs, and brain.
High hCG levels: Choriocarcinoma can cause extremely high hCG levels in the blood. This is a diagnostic indicator.
Aggressive Behavior: Due to its aggressive nature, this cancer responds well to chemotherapy. However, it requires a prompt and aggressive approach.
A choriocarcinoma may develop as a result of a previous hydatidiform lesion or as part of a mixed gestational tumor. A favorable outcome is possible with choriocarcinoma if it’s diagnosed and treated early.
Background Information
Let’s dig deeper into the history of hydatidiform choriocarcinoma and hydatidiform mole:
Hydatidiform Mole (Molar Pregnancy):
- Definition: A hydatidiform mole is a rare abnormal pregnancy in which a mass tissue develops inside the uterus instead of a normal embryo. This condition is also known as a molar pregnancy.
- Types:
-
- Completed Hydatidiform Mole: When an egg (ovum), or two sperms fertilize a normal ovary, this occurs. The genetic material that is produced is all paternal, meaning it comes from the father. There is no fetal growth. This type is commoner and usually associated with more severe symptoms.
- Partial hydatidiform mole: A regular egg is fertilized with two sperms or by a single sperm which duplicates the genetic material of the egg. The sperm contains both maternal and paternal genetic material. There may also be some fetal growth. The fetus, however, is not viable and the placental tissues are abnormal.
- Pathogenesis: The absence of fetal growth and abnormal fertilization can result in complete hydatidiform lesions.The partial hydatidiform melanoma is caused by fertilization errors, which result in both normal and abnormal tissue.Choriocarcinoma:
- Definition: Choriocarcinoma, is a malignant cancerous tumor that develops in trophoblastic (placental) cells during pregnancy. It has no relation to fetal growth and is caused when these trophoblastic (placental-forming) cells turn cancerous.
- Epidemiology: Choriocarcinoma, a rare cancerous tumor, occurs in approximately 1 out of every 40,000 pregnancies. The risk of developing it is greater after a molar pregnancy.
- Pathogenesis: The uncontrolled growth of trophoblastic cells leads to a malignant tumor. Early diagnosis and treatment are crucial because it often spreads to other organs. This includes the liver, lungs, and brain.It is important for patients and clinicians to understand the background of these conditions in order to make an accurate diagnosis and decide on appropriate treatment.
Human chorionic Gonadotropin (hCG) is a hormone that is produced during pregnancy and is used as a diagnostic marker for both conditions. These gestational trophoblastic disorders can only be managed effectively if they are detected early and treated promptly.
Hydatidiform Mole and Choriocarcinoma in the comparison chart
Here’s a concise comparison chart summarizing the key differences between hydatidiform mole and choriocarcinoma:
| Feature | Hydatidiform Mole | Choriocarcinoma |
| Definition | Abnormal pregnancy is where nonviable tissue forms instead of a fetus. | Highly malignant cancer arising from trophoblastic cells. |
| Types | – Complete (no fetal development) – Partial (some fetal development) | N/A |
| Pathogenesis | Abnormal fertilization leads to the proliferation of trophoblastic cells. | Cancerous transformation of trophoblastic cells. |
| Clinical Presentation | – Vaginal bleeding – Pelvic pain – Enlarged uterus – High hCG levels | – Vaginal bleeding – Pelvic pain – Metastases (lungs, liver, brain) – High hCG levels |
| Diagnosis | Histopathology, ultrasound, high hCG levels | Histopathology, imaging, high hCG levels |
| Prognosis | Generally favorable, the risk of malignancy transformation is low. | Favorable with early diagnosis and treatment, metastasis affects prognosis. |
| Treatment | Dilation and curettage (D&C), follow-up care | Chemotherapy (methotrexate, etoposide, cisplatin), radiation (if necessary), monitoring, and follow-up |
| Risk of Recurrence | Lower for complete mole, higher for partial mole | Depends on the response to treatment and the extent of metastasis |
| Typical Patient Profile | Women of childbearing age | Women of childbearing age |
| Metastasis | Rare (unless transformed into choriocarcinoma) | Common, especially in the lungs, liver, and brain |
| Fetal Development | Absent (complete mole) or abnormal (partial mole) | Absent, no fetal development |
| Overall Prognosis | Generally good with proper management | Favorable with prompt treatment and monitoring |
Please note that while this chart provides a concise overview, both conditions can vary in presentation and outcomes based on individual factors and the stage of the disease at diagnosis. Early detection and appropriate medical care are critical for the best possible prognosis in both cases.
Clinical Presentation
This is an overview of the hydatidiform mole and choriocarcinoma clinical presentation:
Hydatidiform Mole (Molar Pregnancy)
Symptoms:
-
- Vaginal Bleeding: This is the most common early sign and can range from mild spots to heavy bleeding.
- Pelvic pain and discomfort: Some women experience pelvic pain or cramping.
Physical Findings:
-
- Uterine Size: The uterus can be larger than expected based on gestational age.
- Theca lutein cysts: These are ovarian cysts that may develop as a result of elevated levels of human gonadotropin. They can be palpable on a physical exam.
- Hyperemesis Gravidarum: Severe vomiting and nausea, more severe than during a normal pregnancy.
Ultrasound Findings:
-
- “Snowstorm’ appearance: An ultrasound can reveal an appearance similar to a mass of grapelike vesicles in the uterus.
- Absence of fetal beat: The absence of the fetal pulse is an important finding in a complete hydatidiform mole.
Choriocarcinoma
Symptoms:
-
- Abnormal vaginal bleeding: This is similar to the hydatidiform mole.
- Pelvic Pain: Women who have choriocarcinoma can experience pelvic pain or discomfort.
- Respiratory symptoms: Symptoms such as cough, chest pain, and shortness of breath may occur if lung metastases exist.
- Neurological symptoms: In cases of brain metastases, neurological symptoms like headaches, seizures or focal deficits can occur.
Physical Findings:
-
- Uterine Enlargement: The uterus can be enlarged, similar to the hydatidiform mole.
- Hepatomegaly: The liver can be palpated to show the extent of metastases.
- Pulmonary Findings: When the lungs are involved, abnormal sounds or findings can be found during a physical exam.
Image Findings:
-
- Metastatic Lesion: Imaging tests, such as chest radiographs or CT scans can reveal metastatic lesions of the liver, brain or other organs.
- Elevated levels of hCG: Blood test results typically show high levels of human gonadotropin, which is a marker for choriocarcinoma.
The clinical presentations of these conditions may overlap, particularly when choriocarcinoma is a result of a hydatidiform mole. Both conditions are characterized by elevated hCG levels, which makes this hormone a vital diagnostic marker. It is important to make an accurate diagnosis, which often involves histopathological evaluation, in order to determine the best treatment for hydatidiform choriocarcinoma.
Prognosis
The prognosis for patients with hydatidiform mole and choriocarcinoma can vary significantly based on several factors, including the type of condition, the stage at diagnosis, the extent of metastasis, and the patient’s overall health. Here’s an overview of the prognosis for each condition:
Hydatidiform Mole (Molar Pregnancy):
- Complete Hydatidiform Mole:
-
- Prognosis is generally good for complete moles, especially when they are diagnosed and treated early.
- Most complete moles do not become malignant, but they do require careful monitoring and follow-up to ensure that no complications, such as gestational trophoblastic neoplasia, develop.
- The risk of developing choriocarcinoma from a complete mole is relatively low but still exists.
- Partial Hydatidiform Mole:
-
- Partial moles have a slightly higher risk of developing into gestational trophoblastic neoplasia or choriocarcinoma compared to complete moles.
- The prognosis depends on factors such as the extent of abnormal tissue and the patient’s response to treatment.
- With appropriate management, most partial moles can be successfully treated.
Choriocarcinoma:
- Metastasis Risk:
-
- Choriocarcinoma is highly aggressive and tends to metastasize to other organs, most commonly the lungs, liver, and brain.
- The prognosis is significantly influenced by the extent and location of metastatic spread.
- Patients with isolated lung metastases generally have a more favorable prognosis than those with widespread or extrapulmonary metastases.
- Survival Rates:
-
- With prompt diagnosis and appropriate treatment, the overall survival rates for choriocarcinoma are relatively high.
- Chemotherapy is the primary treatment, and many patients respond well to chemotherapy regimens that include drugs such as methotrexate, etoposide, and cisplatin.
- The 5-year survival rate for patients with choriocarcinoma is often greater than 90%, especially when the disease is confined to the uterus or has only minimal metastasis.
- Response to Treatment:
-
- Choriocarcinoma is highly responsive to chemotherapy, which can lead to rapid regression of the tumor and resolution of elevated hCG levels.
- Patients typically require close monitoring of hCG levels after treatment to confirm remission.
The prognosis for both hydatidiform mole and choriocarcinoma is generally favorable when these conditions are diagnosed and treated in a timely and appropriate manner. Regular follow-up care and monitoring are essential to ensure that any potential recurrences or complications are detected and managed promptly. Patients with a history of molar pregnancies should be closely monitored in subsequent pregnancies as well to ensure a healthy outcome.
Treatment
The treatment of hydatidiform mole and choriocarcinoma involves different approaches due to the distinct nature of these conditions.
Here’s an overview of the treatment strategies for each:
Hydatidiform Mole (Molar Pregnancy):
- Surgical Management:
-
- The primary treatment for hydatidiform mole is the surgical removal of the abnormal tissue from the uterus. This procedure is called a dilation-curettage (D&C).
- During a D&C, a healthcare provider dilates the cervix and scrapes away the molar tissue from the uterine lining.
- Follow-Up Care:
-
- After the D&C, patients require close monitoring, which includes regular measurement of human chorionic gonadotropin (hCG) levels.
- The hCG levels should decrease over time. Persistent or rising hCG levels may indicate the presence of gestational trophoblastic neoplasia (GTN), which requires further treatment.
- Patients are advised to avoid pregnancy for a specific period to allow for monitoring and to prevent potential complications.
Choriocarcinoma:
- Chemotherapy:
-
- Choriocarcinoma is highly responsive to chemotherapy. Various chemotherapy regimens are used, including single-agent and multi-agent therapies.
- Common chemotherapy drugs used in the treatment of choriocarcinoma include methotrexate, etoposide, and cisplatin.
- Chemotherapy is administered in cycles, and the choice of regimen depends on factors such as the extent of metastasis and the patient’s overall health.
- Radiation Therapy:
-
- Radiation therapy may be considered in cases of choriocarcinoma with localized brain metastases or other specific situations.
- It is generally less commonly used than chemotherapy but may be necessary in certain circumstances.
- Monitoring and Follow-Up:
-
- Patients with choriocarcinoma require close monitoring of human chorionic gonadotropin (hCG) levels and imaging studies (e.g., CT scans) to assess the response to treatment.
- Treatment continues until hCG levels return to normal and imaging studies show the resolution of the tumor.
- Even after apparent remission, long-term follow-up is essential to detect and manage any potential relapses.
- Management of Recurrence or Resistance:
-
- In cases of choriocarcinoma that do not respond to initial chemotherapy or experience recurrence, alternative chemotherapy regimens may be considered.
- In some cases, high-dose chemotherapy with stem cell transplantation may be an option for patients with resistant disease.
It’s important to note that early diagnosis and prompt initiation of treatment are critical for a successful outcome in both hydatidiform mole and choriocarcinoma. Regular follow-up care is necessary to monitor the patient’s condition, ensure that hCG levels return to normal, and detect any potential complications or recurrences. Multidisciplinary care involving gynecologists, oncologists, and other specialists is often necessary for comprehensive management.
Conclusion
Hydatidiform mole and choriocarcinoma are distinct gestational trophoblastic diseases that require different approaches to diagnosis and treatment.
Early detection and appropriate management are essential for favorable outcomes, with surgical removal being the primary treatment for hydatidiform mole and chemotherapy being highly effective for choriocarcinoma.
Regular monitoring and follow-up care are crucial for ensuring patient well-being and detecting potential recurrences or complications.
