Endometrioma and hemorrhagic cysts may sound similar, but the key difference between them is that endometrioma cysts form when tissue similar to the lining of the uterus begins to grow on the ovaries. It is often associated with endometriosis, a condition in which the lining of the uterus grows outside the uterus.
Hemorrhagic cysts, on the other hand, occur when bleeding occurs inside a follicular or corpus luteum cyst. It’s like a cyst that gets a small wound inside.
Both of these cysts are quite common in the female reproductive system. These can vary from simple everyday cysts to more serious cysts, but they are mostly found on the ovaries. Sometimes, you can find cysts outside the ovary as well.
Important of Endometrioma and Hemorrhagic Cyst
Understanding the difference between endometrioma (endometrial cancer) and hemorrhagic syringomyelia for several reasons is vitally important.
- Diagnosis is important: accurate diagnosis requires accurate differentiation between hemorrhagic and endometrioma. These two conditions may have similar symptoms and clinical presentation, so it is important to distinguish them using the right diagnostic method. A correct diagnosis is essential for the right treatment and management.
- 2. Treatment choices: there may be different approaches for managing endometrioma versus hemorrhagic syringomas. Endometriomas associated with endometriosis require treatment options to address both cyst and endometriosis symptoms; on the other hand, hemorrhagic cysts typically do not need active management. They often resolve themselves. Understanding the differences will allow healthcare providers to select the best treatment option for each case.
- Endometriomas: Endometriomas have been linked with infertility, so when trying to conceive it’s crucial that accurately identify an endometrioma. It may require fertility treatment or intervention. Hemorrhagic cysts, on the other hand, do not usually affect fertility. The specific type of cyst helps healthcare providers to provide the appropriate guidance and counseling regarding fertility concerns.
- Long-term impacts: endometriomas or endometriosis can have long-term repercussions for patients’ reproductive and general health, so understanding their relationship and follow-up can provide proper monitoring, treatment, and care. Although hemorrhagic cysts tend to self-resolve with no lasting ill effects on health, they should still be evaluated and monitored regularly.
- Patient support and education: healthcare providers can educate and support patients more effectively if they know the difference between endometrioma, hemorrhagic syringes, and other conditions. Patients can actively participate in their healthcare by learning about the symptoms, complications, and treatment options of each condition.
Understanding the differences between endometrioma, hemorrhagic syringes, and uterine fibroids allows for accurate diagnosis, selection of appropriate treatment, consideration of fertility effects, anticipating long-term consequences, and effective patient support.
What is Endometrioma?
An endometrioma, also known as an endometriotic cyst or chocolate cyst, is a specific type of ovarian cyst that forms when endometrial tissue, which normally lines the inside of the uterus, starts to grow abnormally within the ovaries. This condition is often associated with endometriosis, a chronic medical condition where endometrial tissue grows outside the uterus, leading to inflammation, scarring, and the formation of adhesions in the pelvic area.
Key characteristics of endometriomas include:
- Endometrial Tissue in the Ovaries: Endometriomas contain tissue that resembles the uterine lining, and this tissue starts growing within one or both ovaries.
- Chocolate-Like Fluid: These cysts are filled with a thick, dark, and old blood-like fluid, which gives them the nickname “chocolate cysts.”
- Potential for Pain: Endometriomas can cause pelvic pain, particularly during menstruation, sexual intercourse, or ovulation. The presence of endometriomas is often associated with severe endometriosis-related pain.
- Infertility: In some cases, endometriomas may contribute to infertility, making it challenging for individuals to conceive.
- Diagnosis: They are typically diagnosed through imaging studies, such as ultrasound or magnetic resonance imaging (MRI), which reveal the presence of these cysts in the ovaries.
- Treatment: Treatment options for endometriomas may include surgery to remove the cysts or medical management, depending on the individual’s symptoms, fertility desires, and overall health.
Endometriomas are considered a specific subtype of ovarian cysts and are a common manifestation of endometriosis. They require proper diagnosis and management, often in collaboration with a healthcare provider specializing in reproductive health and gynecological conditions.
What is a Hemorrhagic Cyst?
A hemorrhagic cyst, also known as a hemorrhagic ovarian cyst, is a type of functional ovarian cyst that develops as a result of bleeding within an existing cyst. Functional ovarian cysts are a normal part of the menstrual cycle and typically resolve on their own. However, in some cases, these cysts can bleed, leading to the formation of a hemorrhagic cyst.
Key characteristics of hemorrhagic cysts include:
- Bleeding Within a Cyst: A hemorrhagic cyst is formed when there is bleeding into an existing functional cyst. This bleeding may occur due to the rupture of small blood vessels within the cyst.
- Appearance: Hemorrhagic cysts often contain fresh, red blood, giving them a distinctive appearance. The blood can either be contained within the cyst or may leak into the pelvic cavity, causing pelvic pain.
- Pain: The sudden bleeding and expansion of the cyst can cause acute pelvic pain on the side where the cyst is located.
- Resolution: Most hemorrhagic cysts resolve on their own as the body reabsorbs the blood over time. However, medical monitoring may be necessary to ensure that the cyst is not causing complications.
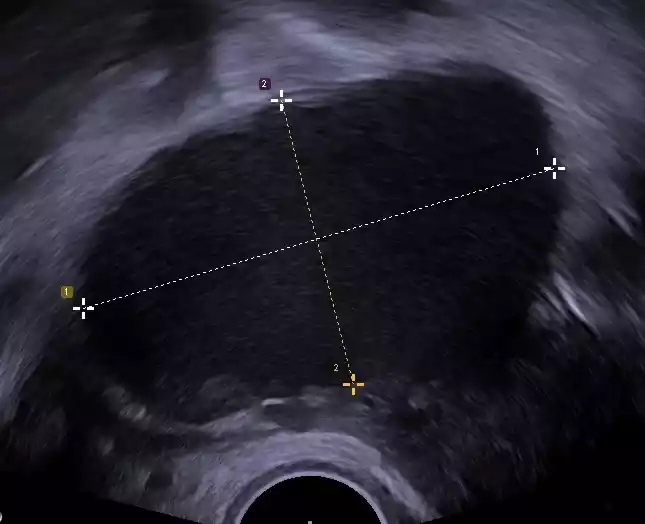
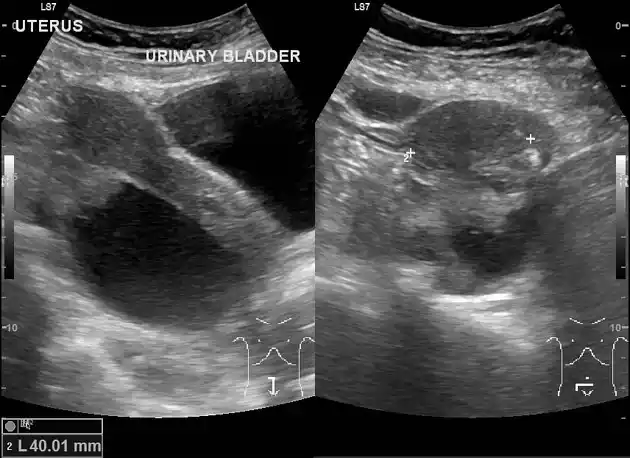
- Diagnostic Methods: Hemorrhagic cysts can be diagnosed through various imaging techniques, such as transvaginal ultrasound, which can reveal the presence of blood and the cyst in the ovaries.
- Treatment: In the majority of cases, treatment for hemorrhagic cysts primarily involves pain management and monitoring. Surgical intervention is rarely required unless complications, such as excessive bleeding or rupture, occur.
Hemorrhagic cysts are considered functional cysts because they originate during the normal menstrual cycle. While they can cause sudden pelvic pain, they are typically benign and tend to resolve without the need for extensive medical intervention. However, it is essential for individuals experiencing severe or persistent symptoms to seek medical evaluation and care.
Key comparison chart
Here’s a key comparison chart summarizing the main differences between endometrioma and hemorrhagic cyst:
| Characteristic | Endometrioma | Hemorrhagic Cyst |
|---|---|---|
| Definition | Cysts formed by abnormal growth of endometrial tissue in the ovaries | Cyst formed due to bleeding within an existing functional cyst |
| Associated Condition | Often associated with endometriosis | Typically a functional cyst within the normal menstrual cycle |
| Fluid Composition | Contains old, dark blood resembling chocolate | Contains fresh, red blood due to recent bleeding |
| Pain Symptoms | May cause pelvic pain during menstruation, sexual intercourse, or ovulation | Can result in acute pelvic pain due to sudden bleeding within the cyst |
| Implications on Fertility | May contribute to infertility in some cases | Generally does not have a significant impact on fertility |
| Diagnostic Methods | Diagnosed through imaging such as ultrasound or MRI | Diagnosed through imaging methods like transvaginal ultrasound |
| Management | Treatment options may include surgery or medication based on symptoms and fertility goals | Typically resolves on its own with pain management and monitoring |
This chart provides a quick overview of the key differences between endometrioma and hemorrhagic cyst, highlighting their definitions, associated conditions, fluid composition, pain symptoms, implications on fertility, diagnostic methods, and management options.
Similarities of Endometrioma and Hemorrhagic Cyst
Endometrioma and hemorrhagic cysts are distinct types of ovarian cysts with different underlying causes and characteristics.
- Ovarian Location: Both endometrioma and hemorrhagic cysts are ovarian cysts, meaning they develop within or on the surface of the ovaries.
- Pain and Discomfort: Both types of cysts can cause pelvic pain and discomfort. Individuals with endometrioma may experience pain during menstruation, sexual intercourse, or ovulation, while those with a hemorrhagic cyst can have acute pelvic pain when the cyst bleeds or expands.
- Diagnostic Methods: Both endometrioma and hemorrhagic cysts can be diagnosed using similar diagnostic methods, including transvaginal ultrasound and other imaging techniques.
- Potential Complications: In some cases, both types of cysts can lead to complications. Endometriomas, if left untreated, can contribute to infertility, while hemorrhagic cysts may lead to significant bleeding and more severe pain.
Despite these similarities, it’s important to remember that the underlying causes, fluid composition, and management strategies for these cysts differ significantly. Understanding these distinctions is crucial for accurate diagnosis and effective management.
Causes and risk factors
Let’s explore the causes and risk factors associated with endometrioma and hemorrhagic cysts:
Causes and Risk Factors of Endometrioma:
- Endometriosis: The primary cause of endometrioma is endometriosis, a chronic condition where the tissue similar to the uterine lining (endometrium) grows outside the uterus. Endometrial tissue may implant and grow within the ovaries, leading to the development of endometriomas.
- Menstrual Flow Backflow (Retrograde Menstruation): Retrograde menstruation, where menstrual blood flows backward into the pelvic cavity instead of out through the cervix, is a common contributing factor to endometriosis and endometriomas.
- Genetic Predisposition: Some individuals may have a genetic predisposition to endometriosis, making them more susceptible to the development of endometriomas.
- Immune System Abnormalities: A compromised immune system or immune dysfunction may contribute to the development of endometrioma, as it may fail to clear abnormal tissue growth effectively.
- Environmental Factors: There is ongoing research into environmental factors, such as exposure to certain chemicals and toxins, that may play a role in the development of endometriosis and endometriomas.
Causes and Risk Factors of Hemorrhagic Cyst:
- Normal Menstrual Cycle: Hemorrhagic cysts are part of the normal menstrual cycle and are considered functional cysts. They develop when a mature follicle or corpus luteum cyst within the ovary experiences bleeding.
- Follicle or Corpus Luteum Rupture: The primary cause of hemorrhagic cysts is the rupture of small blood vessels within a functional cyst. This rupture leads to bleeding within the cyst.
- Hormonal Fluctuations: Hormonal imbalances or fluctuations, such as those related to the menstrual cycle, can increase the likelihood of cyst formation and, in some cases, bleeding within these cysts.
- Age and Reproductive Stage: Hemorrhagic cysts are more common in individuals of reproductive age, particularly those who are still menstruating regularly.
- Medical Conditions: Certain medical conditions, such as polycystic ovary syndrome (PCOS) or irregular menstrual cycles, may slightly elevate the risk of functional cysts, which can potentially become hemorrhagic.
It’s essential to note that while these factors may increase the likelihood of developing endometrioma or hemorrhagic cysts, these cysts can also occur without any identifiable risk factors. Medical evaluation and diagnosis are crucial for understanding the specific causes and risks associated with these conditions in individual cases.
Conclusion
Endometrioma and hemorrhagic cysts are two distinct ovarian cysts with distinct characteristics, causes, and implications. Endometriomas, which contain endometrial tissue, are associated with endometriosis while hemorrhagic cysts result from bleeding within their cyst and are unrelated to endometriosis directly.
Endometriomas are filled with old blood and have a dark chocolate-like appearance; hemorrhagic cysts contain fresh blood that appears reddish or dark in appearance. Recognizing these differences is critical for accurate diagnosis, appropriate management, and effective treatment of any potential underlying conditions.
