A brief overview of Scarlet Fever and Kawasaki Disease
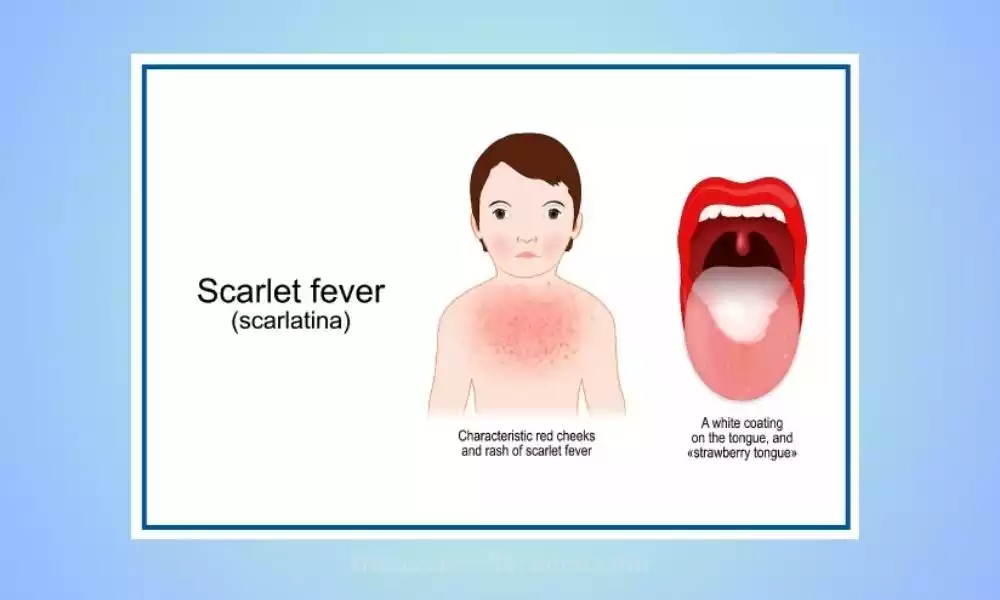
Scarlet Fever: The same bacteria that causes strep is responsible for scarlet fever, Streptococcus. Scarlet fever typically strikes between the ages of 5-15 but can occur at any age; its hallmark symptoms are distinctive rashes, high fevers, sore throats, and swollen tonsils.
Scarlet fever is caused by bacteria producing a toxin that produces the distinctive red, rash seen with scarlet fever, initially starting on the neck and chest areas and spreading throughout other body areas such as the abdomen, back, extremities, etc.
Fine red streaks have a rough surface texture similar to a sandpaper-looking texture; usually lasting 1-3 weeks before additional symptoms such as headache, chills nausea, or vomiting occur.
As well as experiencing a rash, those affected with scarlet fever may also develop strawberry tongue symptoms – an appearance where their tongue turns red and bumpy; their tonsils swollen with a white coating covering, small red spots on the roof of the mouth surface as well as a flushed face with pale areas around mouth region may develop; some individuals even show flushing facial features with pale areas around the mouth region.
Scarlet fever left untreated can result in complications, including rheumatic fever, kidney inflammation (glomerulonephritis), and ear infections. Therefore, early diagnosis and proper antibiotic treatments–typically penicillin or amoxicillin -are crucial to ensure recovery without adverse complications and ensure effective recovery outcomes.
Scarlet fever is an infectious, contagious infection spread via respiratory droplets from infected individuals. Adopting good hygiene practices such as handwashing regularly or covering one’s mouth and nose when coughing or sneezing can help mitigate its spread and slow its occurrence.
Kawasaki Disease:
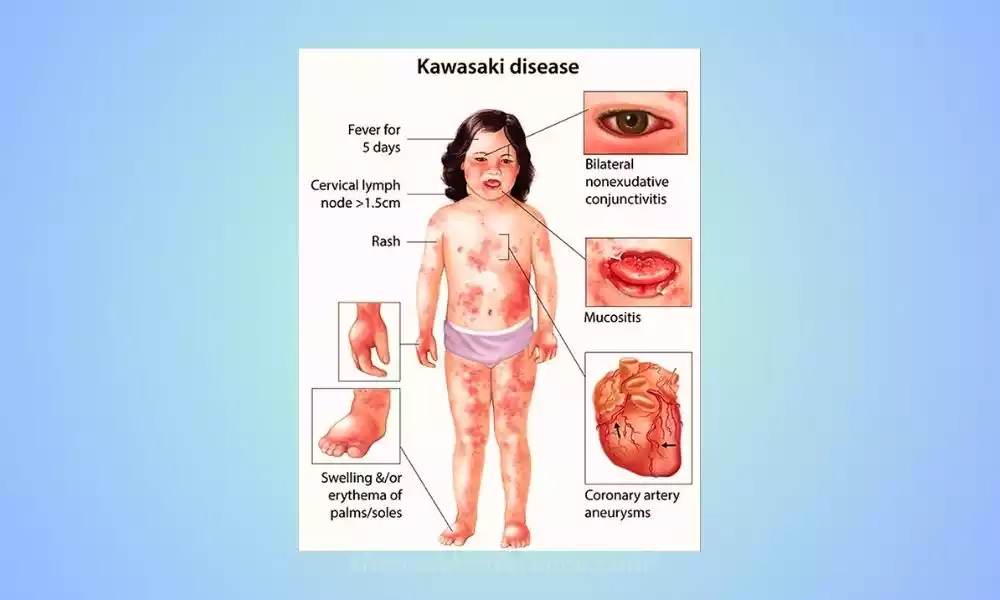
Kawasaki disease is an uncommon but potentially severe disorder primarily affecting young children under five. Aneurysms arise due to inflammation in blood vessels throughout the body, most often coronary arteries which supply oxygen-rich blood to the heart.
The causes of Kawasaki disease remain unclear, although experts believe an abnormal immune response triggered by infection or environmental factors may play a part. This disease does not seem to be contagious and does not appear to have direct inherited links.
The clinical features of Kawasaki disease include a persistent high fever that lasts for at least five days, along with other symptoms. These symptoms may include:
Rash: A non-itchy rash often appears during the acute phase of the illness. It typically involves the trunk, groin, and genital areas, and may have a reddened appearance.
Conjunctivitis: Redness and inflammation of the whites of the eyes (conjunctiva) is common in Kawasaki disease. The eyes may also become bloodshot or swollen.
Changes to Lips and Mouth: Lips may become dry, cracked, and swollen; often appearing reddened or “strawberry”. The tongue may also develop a white coating, with red bumps (known as “strawberry tongue”).
Swollen lymph nodes: Enlarged lymph nodes, particularly in the neck region, are common in Kawasaki disease.
Swollen hands and feet: Hands and feet may become swollen and reddened, with peeling or blistering rash appearing on palms and soles.
If left untreated, Kawasaki disease can lead to complications, particularly affecting the coronary arteries. Coronary Artery Aneurysms, which are weak or bulging sections of blood vessels, pose serious threats to heart health as they increase your risk for serious cardiac problems like heart attacks or rupture of the aneurysm itself.
Prompt diagnosis and treatment of Kawasaki disease are crucial to reduce the risk of complications. Standard treatment entails intravenous immunoglobulin (IVIG) to lower inflammation and shield coronary arteries against damage. Aspirin can also help reduce fever and inflammation; its dosage and duration depend upon the stage of the disease.
Regular follow-up care should be administered for individuals who have experienced coronary artery aneurysms to monitor heart and blood vessel health, especially as part of preventative medicine measures.
Kawasaki disease is typically self-limiting, and most children recover fully without long-term complications if treated promptly and appropriately.
Importance of understanding the differences between the two conditions
Understanding the differences between Scarlet Fever and Kawasaki Disease is of significant importance for several reasons:
Accurate diagnosis: Scarlet Fever and Kawasaki Disease have distinct clinical presentations; being able to distinguish them is integral for proper diagnosis and treatment. Misdiagnosis can lead to delayed or inappropriate management, potentially resulting in complications or worsening of the condition.
Treatment approach: Scarlet Fever can typically be treated using antibiotics like penicillin or amoxicillin to eliminate its bacterial source and restore health. Kawasaki Disease requires specific therapies, including intravenous immunoglobulin (IVIG) therapy and aspirin administration to manage systemic inflammation and avoid further complications. Understanding the differences in treatment approaches is essential to provide the appropriate interventions for each condition.
Prevention of complications: Both Scarlet Fever and Kawasaki Disease can have serious complications if left untreated or mismanaged. Scarlet Fever can lead to conditions like rheumatic fever and glomerulonephritis, while Kawasaki Disease can result in coronary artery abnormalities and potential heart-related complications. Early recognition and appropriate treatment based on the correct diagnosis can help prevent these complications and ensure better patient outcomes.
Public health implications: Scarlet Fever is a contagious disease that can spread easily within communities, especially among children. Understanding its distinct features and promptly identifying cases can aid in implementing appropriate public health measures, such as isolation precautions and antibiotic treatment to prevent further transmission. Kawasaki Disease, although not contagious, requires awareness among healthcare providers to ensure early detection and appropriate management to minimize potential complications.
Research and education: Studying and understanding the differences between Scarlet Fever and Kawasaki Disease contribute to the overall body of medical knowledge. Researchers and healthcare providers alike can leverage it to gain deeper insights into each condition’s pathophysiology, risk factors, and long-term implications. Furthermore, disseminating accurate information through educational initiatives can enhance public awareness, enabling individuals to recognize symptoms and seek timely medical attention.
Distinguishing between Scarlet Fever and Kawasaki Disease is crucial for accurate diagnosis, appropriate treatment, prevention of complications, public health measures, and furthering medical knowledge. By understanding these differences, healthcare professionals can provide optimal care and improve patient outcomes.
Scarlet Fever
Its Scarlet fever, also referred to as group A Streptococcus bacterium infection, primarily affects children but can affect adolescents and adults as well. Scarlet fever symptoms typically include a distinctive rash with fever spike, sore throat symptoms, and enlarged tonsils.
Scarlet fever bacteria produce an erythrogenic toxin which results in its trademark rash: typically seen around the neck and chest before spreading to other parts of the body like the abdomen, back, and extremities.
It appears as fine red dots with a rough texture similar to sandpaper that last for approximately one week before additional symptoms such as headache, chills, nausea, or vomiting occur.
Scarlet fever victims may develop additional symptoms beyond its familiar rash: the strawberry tongue is one such condition; this form is characterized by red and bumpy patches on the tongue that appear red-toned; tonsils swollen to an unsettling degree may become covered with white coating; red spots could form on the roof of the mouth as well. Some individuals also show flushed faces with pale areas around the mouth area.
Scarlet fever is highly contagious and spreads via respiratory droplets from infected individuals or through direct skin lesions or surfaces contaminated by bacteria. Therefore, good hygiene practices like handwashing frequently and covering the mouth and nose when coughing/sneezing may help limit its spread.
Early identification and use of antibiotics such as penicillin or ampicillin are key to avoiding complications and speeding recovery. Antibiotic therapy works to eliminate bacteria that cause symptoms while shortening duration and severity.
For optimal outcomes it’s essential that all prescribed courses of antibiotics be completed as advised by healthcare providers; otherwise, recurrence of bacteria could occur later.
Scarlet fever if left untreated can result in complications including rheumatic fever, kidney inflammation (glomerulonephritis), and ear infections – so seeking medical assistance if you suspect scarlet fever should always be your top priority.
The Scarlet fever infection is a bacterial infection that causes rash, fever, sore tonsils, and a sore throat. It must be treated early to avoid complications. Prompt diagnosis and appropriate therapy are key in managing scarlet fever infections effectively and avoiding complications that arise as a result.
Definition and background information
Scarlet fever is also known as group A Streptococcus. It is an infection caused by Streptococcus Bacteria. Symptoms include red rashes that appear on the back and arms, a high Fever, and a sore throat. The name itself derives from this characteristic scarlet red-hued rash associated with scarlet fever infections.
Scarlet fever was once an extremely dangerous and possibly lethal infection during the 19th and early 20th centuries, yet with antibiotics like penicillin now widely available the mortality rate has significantly diminished and treatment is generally effective against it.
Scarlet fever-inducing bacteria may also spread via coughing or sneezing or through direct contact with the nasal and throat secretions of an individual infected. Such infections result in strep throat symptoms.
Scarlet fever most frequently affects children between five and 15, though anyone of any age is susceptible. Winter and spring seasons tend to see increased cases; typically an incubation period (the timeframe between exposure to bacteria and symptoms manifesting itself) of two to four days will pass before symptoms manifest themselves.
Scarlet fever’s signature symptom is its characteristic rash. This reddening rash typically begins around the neck and chest area before spreading across other parts of the body; its texture resembling that of sandpaper gives skin reddening effects.
Furthermore, other symptoms associated with scarlet fever include high fever (often exceeding 101degF or 38.3degC), sore throat discomfort, difficulty swallowing difficulties and lymph node swellings along with white or yellow-colored tonsils with thick coatings are present alongside this characteristic rash.
Prompt diagnosis of scarlet fever is key to receiving appropriate antibiotic treatment, usually via antibiotics. Diagnosis generally includes clinical symptoms, physical examination findings, and laboratory tests such as throat swabs to test for Streptococcus pyogenes bacteria or perform rapid strep tests.
Scarlet fever treatment typically includes taking antibiotics such as penicillin or amoxicillin to eliminate the bacteria that cause it. For maximum effectiveness and to avoid complications, be sure to complete all prescribed courses of antibiotics prescribed by healthcare providers as instructed.
Scarlet fever usually responds well to appropriate treatment and most individuals recover without long-term complications; therefore it is crucial that anyone suspected of scarlet fever seek medical advice immediately in order to be diagnosed and receive proper diagnosis and care.
Kawasaki Disease
Kawasaki disease is an acute febrile illness that primarily impacts children under 5 years of age. Systemic vasculitis refers to inflammation of all of the blood vessels throughout the body, particularly coronary arteries that provide vitality to your heart. Kawasaki disease is named after the Japanese pediatrician, Dr. Tomisaku Kawasaki, who first described the condition in 1967.
Kawasaki disease remains unexplained; however, experts speculate that its source may lie within an abnormal immune response caused by infection or environmental exposures. This disease does not appear to be contagious and does not seem directly heritable.
Kawasaki disease typically presents with a persistent high fever that lasts for at least five days, along with other characteristic symptoms. These symptoms may include:
Rash: A non-itchy rash often appears during the acute phase of the illness. It typically involves the trunk, groin, and genital areas and may have a reddened appearance.
Conjunctivitis: Redness and inflammation of the whites of the eyes (conjunctiva) is common in Kawasaki disease. The eyes may also become bloodshot or swollen.
Changes in the lips and mouth: The lips may become dry, cracked, and swollen, often with a bright red or “strawberry” appearance. The tongue may also develop a white coating, with red bumps (known as “strawberry tongue”).
Swollen lymph nodes: Enlarged lymph nodes, particularly in the neck region, are common in Kawasaki disease.
Swollen hands and feet: The hands and feet may become swollen and red, with a peeling or blistering rash on the palms and soles.
Other symptoms associated with Kawasaki disease could include irritability, abdominal pain, diarrhea, and joint discomfort.
If left untreated, Kawasaki disease can lead to complications, particularly affecting the coronary arteries. Coronary Artery Aneurysms, weak and bulging areas in blood vessels that increase the risk for heart attack or rupture, should be of great concern and can pose significant threats.
Prompt diagnosis of Kawasaki disease is crucial for time management and prevention of complications. The diagnosis is based on the presence of specific clinical criteria established by the American Heart Association. Laboratory tests such as blood tests and echocardiograms may also help with diagnosing coronary arterial involvement and assessing its extent.
Treatment for Kawasaki disease involves hospitalization and administration of intravenous immunoglobulin (IVIG), which helps reduce inflammation and prevent coronary artery damage. High-dose aspirin may help relieve fever and inflammation; its dosage and duration depend on the stage of the disease.
Individuals diagnosed with coronary artery aneurysms must receive regular follow-ups to ensure optimal heart and vessel health. Most children with Kawasaki disease recover fully without long-term complications if treated promptly and appropriately. However, some individuals may require ongoing cardiac monitoring and follow-up care.
Kawasaki disease is a rare but potentially serious condition characterized by systemic inflammation and involvement of the blood vessels, particularly the coronary arteries. To reduce risk and optimize patient outcomes, early identification, and treatment must take place. To be most effective, early diagnosis must also include early treatment of patients.
Definition and background information
Kawasaki disease is an uncommon but significant childhood illness characterized by inflammation of the blood vessels, primarily affecting children under the age of 5. It was first identified by Dr. Tomisaku Kawasaki in Japan in the 1960s and has since been recognized worldwide.
Kawasaki disease remains unexplained; however, researchers speculate that an abnormal immune response triggered by various infections, genetic predisposition, and environmental influences could play a part. This condition does not spread and does not become contagious.
Kawasaki disease typically manifests as a high fever persisting for at least five days, accompanied by a range of symptoms affecting multiple organ systems.
These include rashes and conjunctivitis (redness and swelling of the eyes), lip and mouth changes such as strawberry-tongue as well as swollen nodes as well as swelling/redness on hands/feet. Other possible symptoms may include irritability, abdominal pain, diarrhea, and joint pain.
One of the most significant complications of Kawasaki disease is its effect on the coronary arteries, which supply blood to the heart muscle. Aneurysms, or bulging and weak areas formed in arterial walls due to inflammation, increase cardiovascular risks such as coronary artery blockages, heart attacks, and other issues in later years.
The diagnosis of Kawasaki disease is primarily based on clinical criteria established by medical experts. Diagnostic methods used for coronary artery disease typically include blood tests and other medical imaging procedures like echocardiography.
Treatment for Kawasaki disease typically involves hospitalization and administration of intravenous immunoglobulin (IVIG), a concentrated mixture of antibodies that helps reduce inflammation and prevent coronary artery damage.
High-dose aspirin may also help relieve fever and inflammation; its dosage and length of usage depend on the stage of illness. Additional therapies and interventions may be recommended based on the individual’s specific condition and symptoms.
With early diagnosis and appropriate treatment, the majority of children with Kawasaki disease recover fully without long-term complications. Long-term monitoring of heart and blood vessel health is necessary, particularly among individuals who develop coronary artery abnormalities.
Research continues to focus on better understanding the causes, risk factors, and optimal treatment approaches for Kawasaki disease. Greater education among healthcare professionals and members of the general public about early recognition and prompt medical intervention of any disease is imperative to improving early recognition and prompt intervention.
Scarlet Fever and Kawasaki Disease in Tabular Form
Here’s a comparison between Scarlet Fever and Kawasaki Disease in a tabular form:
| Aspect | Scarlet Fever | Kawasaki Disease |
|---|---|---|
| Age group affected | Primarily children (5-15 years) | Primarily children under 5 years old |
| Etiology | Caused by Streptococcus pyogenes | Exact cause unknown |
| Rash characteristics | A fine, red rash with a rough texture resembling sandpaper | Non-itchy rash, more diffuse in appearance |
| Mucous membrane involvement | Strawberry tongue, swollen tonsils | Conjunctivitis, red and swollen lips and tongue |
| Additional symptoms | Sore throat, enlarged lymph nodes | Fever, swollen hands, and feet, irritability |
| Complications | Rheumatic fever, glomerulonephritis, ear infections | Coronary artery abnormalities, aneurysms |
| Diagnostic criteria | Clinical symptoms, physical examination findings, laboratory tests | Clinical criteria established by experts, laboratory tests |
| Treatment | Antibiotics (penicillin, amoxicillin) | Intravenous immunoglobulin (IVIG) therapy, aspirin |
| Similarities | Acute febrile illnesses, skin manifestations (rash) | Potential cardiovascular complications |
Please be aware that this table only presents a broad comparison, not covering every possible facet of both conditions. The information should not replace professional medical advice, and it is important to consult healthcare professionals for accurate diagnosis, treatment, and management.
Similarities between Scarlet Fever and Kawasaki Disease
While Scarlet Fever and Kawasaki Disease are distinct conditions with several differences, there are a few similarities between them:
Acute febrile illnesses: Both Scarlet Fever and Kawasaki Disease are characterized by a sudden onset of high fever. Both diseases tend to produce persistent fever that lasts several days or even more.
Rash and skin manifestations: Both diseases can present with skin manifestations. Scarlet fever is characterized by a distinctive sandpaper-style rash that often begins on the chest and neck and spreads throughout the entire body, beginning first as chest and neck symptoms before eventually covering more areas of skin. Kawasaki Disease also manifests with a rash, although the appearance and distribution of the rash are different from Scarlet Fever. The rash in Kawasaki Disease is often more diffuse and may involve the trunk, groin, and genital areas.
Potential complications involving the cardiovascular system: While complications are more common in Kawasaki Disease, both conditions can affect the cardiovascular system. In Scarlet Fever, untreated or inadequately treated cases can lead to complications such as rheumatic fever, which can involve inflammation of the heart valves. Kawasaki Disease involves inflammation that predominantly impacts blood vessels, particularly coronary arteries, leading to aneurysms or other abnormalities forming within these networks.
Note that although these conditions share similarities, proper diagnosis, and treatment require accurate differentiation to achieve success. Healthcare professionals should carefully evaluate the specific clinical features, age groups, and other distinguishing factors to make an accurate diagnosis and provide the most effective management for each condition.
Conclusion
Understanding the differences between Scarlet Fever and Kawasaki Disease is crucial for accurate diagnosis, appropriate treatment, and prevention of complications.
Scarlet Fever is caused by a bacterial infection and commonly affects children, typically manifested with distinctive symptoms including fever, rash, and sore throat. Kawasaki Disease, on the other hand, is an autoimmune condition primarily affecting young children that involves systemic inflammation of both their blood vessels and overall system.
Recognizing the variations in clinical features, age groups affected, etiology, and complications is essential for healthcare professionals to provide optimal care and ensure better patient outcomes.
Prompt diagnosis and appropriate treatment, such as antibiotics for Scarlet Fever and IVIG therapy for Kawasaki Disease, can help prevent complications and promote recovery.
