Both lead to sneezing, congestion, and runny noses, but they originate from distinct sources. Allergic rhinitis is triggered by an immune response to allergens, while vasomotor rhinitis is linked to changes in the autonomic nervous system. Understanding the nuances between these conditions is essential for accurate diagnosis and tailored treatment.
This introduction sets the stage for delving into the intricate differences between allergic rhinitis and vasomotor rhinitis, ensuring that individuals and medical professionals alike can navigate their unique characteristics effectively.
Allergic Rhinitis: Causes, Symptoms, and Characteristics
Allergic Rhinitis: Causes, Symptoms, and Characteristics
Allergic rhinitis, commonly known as hay fever, is a prevalent and bothersome condition that affects the nasal passages and is driven by the immune system’s response to allergens. This section explores the causes, symptoms, and distinguishing characteristics of allergic rhinitis.
Causes: Allergic rhinitis arises from the body’s immune system overreacting to otherwise harmless substances called allergens. When individuals with a predisposition to allergies come into contact with these allergens, their immune system produces antibodies called immunoglobulin E (IgE). These IgE antibodies attach to mast cells and basophils, two types of immune cells. Upon subsequent exposure to the same allergen, these cells release histamine and other chemicals, causing inflammation and the characteristic symptoms of allergic rhinitis.
Symptoms: The symptoms of allergic rhinitis can vary in severity and typically involve the upper respiratory tract.
Common symptoms include:
- Sneezing: Frequent, rapid, and uncontrollable sneezing is a hallmark of allergic rhinitis.
- Runny Nose (Rhinorrhea): Excessive production of thin, clear mucus from the nasal passages.
- Nasal Congestion: Swelling and inflammation of nasal tissues lead to a blocked or stuffy nose.
- Nasal Itching: Persistent itching inside the nose is a distinguishing feature of allergic rhinitis.
- Watery Eyes (Conjunctivitis): Irritation and itching of the eyes with clear, watery discharge.
- Postnasal Drip: Mucus produced in the nasal passages can drip down the back of the throat, causing irritation and coughing.
- Fatigue: Chronic congestion and poor sleep quality can result in fatigue and reduced overall well-being.
- Loss of Smell and Taste: In severe cases, allergic rhinitis may impair the senses of smell and taste.
Characteristics: Several key characteristics differentiate allergic rhinitis from other forms of rhinitis:
- Seasonal and Perennial Patterns: Allergic rhinitis can be classified into seasonal and perennial forms. Seasonal allergic rhinitis, often referred to as “hay fever,” occurs during specific pollen seasons, while perennial allergic rhinitis persists throughout the year due to indoor allergens like dust mites, pet dander, and mold spores.
- Triggers: Allergic rhinitis symptoms are triggered by exposure to specific allergens. Individuals often experience symptoms upon contact with the allergens to which they are sensitized.
- Positive Allergy Tests: Skin prick tests or blood tests can identify the specific allergens to which an individual is allergic. Elevated levels of allergen-specific IgE antibodies indicate sensitization.
- Associations with Other Conditions: Allergic rhinitis is frequently associated with other allergic conditions such as asthma, atopic dermatitis (eczema), and allergic conjunctivitis.
- Response to Allergy Medications: Allergic rhinitis symptoms usually respond well to antihistamines, which block histamine release, and intranasal corticosteroids, which reduce inflammation.
Allergic rhinitis is a common condition characterized by the immune system’s overreaction to allergens. Its symptoms include sneezing, runny nose, nasal congestion, itching, and watery eyes. Recognizing the distinctive seasonal or perennial patterns, identifying triggering allergens, and utilizing appropriate treatments are crucial for effectively managing allergic rhinitis and improving an individual’s overall quality of life.
Treatment options
Effective management of allergic rhinitis involves a range of treatment options to alleviate symptoms and improve quality of life.
Common approaches include:
- Allergen Avoidance: Minimize exposure to known allergens, such as pollen, dust mites, and pet dander.
- Antihistamines: Over-the-counter or prescription medications that block histamine release, reducing itching, sneezing, and runny nose.
- Intranasal Corticosteroids: Prescription nasal sprays that reduce inflammation and relieve congestion and other symptoms.
- Decongestants: Short-term relief from nasal congestion by narrowing blood vessels in the nasal passages; available in oral or nasal spray forms.
- Allergy Immunotherapy (Allergy Shots): Gradual exposure to allergens to desensitize the immune system and reduce allergic reactions.
- Intranasal Anticholinergics: Prescription nasal sprays that help reduce runny nose by blocking certain nerve signals.
- Combination Medications: Some products contain a combination of antihistamines and decongestants for comprehensive symptom relief.
- Saline Nasal Irrigation: Rinsing nasal passages with a saline solution to clear mucus and reduce inflammation.
- Environmental Control Measures: Implementing strategies to reduce indoor allergens, such as using allergen-proof bedding and air purifiers.
Treatment choices depend on the severity of symptoms, triggers, and individual preferences. Consulting a healthcare professional is essential for personalized recommendations and effective management.
Vasomotor Rhinitis: Causes, Symptoms, and Characteristics
Vasomotor rhinitis is a non-allergic condition characterized by nasal symptoms similar to allergic rhinitis but with distinct underlying mechanisms. This section explores the causes, symptoms, and distinguishing characteristics of vasomotor rhinitis.
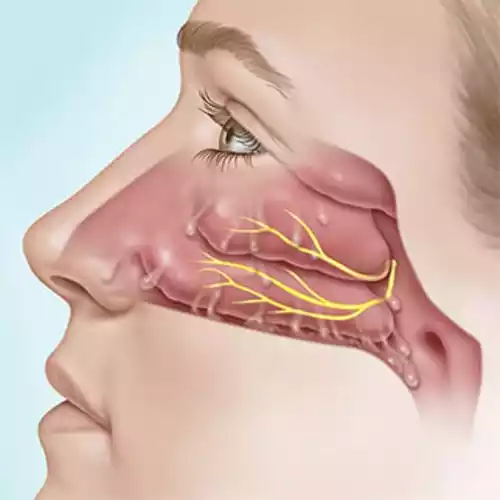
Causes: Unlike allergic rhinitis, vasomotor rhinitis isn’t triggered by allergens. Instead, it’s associated with dysfunction in the autonomic nervous system that controls blood vessel dilation in the nasal passages. This dysfunction can result from factors such as changes in temperature, humidity, air pollutants, strong odors, and hormonal fluctuations.
Symptoms: The symptoms of vasomotor rhinitis mirror those of allergic rhinitis, but there are notable differences:
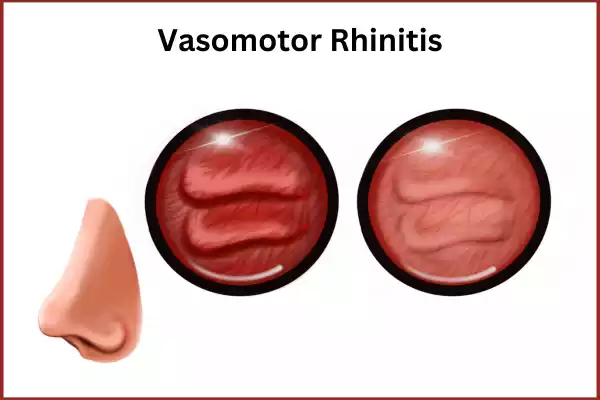
- Nasal Congestion: Persistent nasal congestion is a key symptom due to blood vessel dilation.
- Runny Nose (Rhinorrhea): Clear nasal discharge is common, resembling the watery discharge in allergic rhinitis.
- Sneezing: Occasional sneezing might occur, but it’s less pronounced than in allergic rhinitis.
- Absence of Itching: Unlike allergic rhinitis, itching of the nose, eyes, and throat is typically absent.
- Lack of Allergic Triggers: Vasomotor rhinitis is not triggered by allergens and doesn’t involve an immune response.
Characteristics: Several distinctive characteristics set vasomotor rhinitis apart from other types of rhinitis:
- Non-Allergic Nature: Unlike allergic rhinitis, vasomotor rhinitis lacks a specific immune response to allergens.
- Trigger Factors: Symptoms are often triggered by environmental changes, such as cold air, humidity shifts, smoke, or strong odors.
- Absence of Positive Allergy Tests: Skin prick tests and blood tests for allergens are typically negative in vasomotor rhinitis cases.
- Fluctuating Symptoms: Symptoms can be unpredictable and might vary in intensity and duration.
- Response to Treatments: Vasomotor rhinitis may respond less effectively to typical allergy medications due to its non-allergic nature.
Vasomotor rhinitis is characterized by symptoms similar to allergic rhinitis but lacks an allergic immune response. Nasal congestion, runny nose, and postnasal drip are key symptoms, often triggered by environmental factors rather than allergens. Understanding the non-allergic nature of vasomotor rhinitis and its distinctive characteristics is essential for accurate diagnosis and tailored management strategies to provide relief and enhance the quality of life.
Treatment options
Managing vasomotor rhinitis involves strategies to alleviate symptoms associated with autonomic nervous system dysfunction.
Common treatment approaches include:
- Environmental Modifications: Avoid triggers such as temperature fluctuations, humidity changes, strong odors, and smoke.
- Topical Nasal Sprays: Intranasal corticosteroids or anticholinergic sprays can help reduce nasal congestion and runny nose.
- Ipratropium Bromide Nasal Spray: An anticholinergic nasal spray that can help control excessive nasal secretions.
- Saline Nasal Irrigation: Rinsing nasal passages with a saline solution to relieve symptoms and maintain nasal health.
- Nasal Filters: Specialized filters that fit inside the nostrils to reduce exposure to irritants.
- Oral Antihistamines: Although vasomotor rhinitis isn’t allergic, some individuals might benefit from antihistamines for symptom relief.
Consulting a healthcare professional is crucial for accurate diagnosis and tailored treatment recommendations to effectively manage vasomotor rhinitis symptoms.
Allergic Rhinitis and Vasomotor Rhinitis comparison chart
Here’s a concise comparison chart outlining the key differences between Allergic Rhinitis and Vasomotor Rhinitis:
| Characteristic | Allergic Rhinitis | Vasomotor Rhinitis |
|---|---|---|
| Underlying Cause | Immune response to allergens | Autonomic nervous system dysfunction |
| Triggers | Allergens such as pollen, dust mites, pet dander | Environmental factors like temperature changes, humidity, odors |
| Immune Response | Involves immune system hypersensitivity, IgE antibodies | No allergic immune response |
| Symptoms | Sneezing, runny nose, nasal congestion, itching, watery eyes | Nasal congestion, runny nose, postnasal drip, absence of itching |
| Seasonal/Perennial | Can be seasonal (pollen seasons) or perennial (indoor allergens) | No distinct seasonal pattern |
| Positive Allergy Tests | Positive results in skin prick tests, blood tests | Negative results in allergy tests |
| Response to Allergies | Responds well to antihistamines, intranasal corticosteroids | May respond less effectively to allergy medications |
| Treatment Approach | Allergen avoidance, medication, immunotherapy | Environmental modifications, nasal sprays, saline rinses |
| Associations | Linked to other allergic conditions (asthma, eczema) | No associations with other allergies |
| Common Names | Hay fever, seasonal allergies | Non-allergic rhinitis |
Note that while this chart provides a simplified comparison, each individual’s condition can vary, and a healthcare professional’s evaluation is essential for accurate diagnosis and personalized treatment.
Conclusion
The distinction between allergic rhinitis and vasomotor rhinitis holds immense significance. Despite their shared nasal symptoms, these two conditions stem from entirely different mechanisms, necessitating accurate diagnosis for tailored management.
Allergic rhinitis, driven by immune responses to allergens, manifests with symptoms like sneezing, itching, and watery eyes. It requires measures such as allergen avoidance, antihistamines, and immunotherapy to effectively control symptoms.
Vasomotor rhinitis, on the other hand, arises from autonomic nervous system dysfunction triggered by environmental factors. This condition results in persistent nasal congestion, runny nose, and postnasal drip, often lacking itching and allergic triggers. Its management involves strategies like environmental modifications and specific nasal sprays.
