Diabetes Mellitus is a chronic metabolic disease characterized by elevated levels of blood sugar. There are two primary types of diabetes: Insulin-Dependent Diabetes Mellitus (IDDM) and Non-Insulin-Dependent Diabetes Mellitus (NIDDM), also known as Type 1 and Type 2 diabetes, respectively.
The two types of diabetes differ in terms of their causes, the age at which they begin, and the treatment methods. Understanding these differences is essential for managing and caring for patients. This brief introduction will examine the differences between IDDM and NIDDM.
A brief overview of IDDM
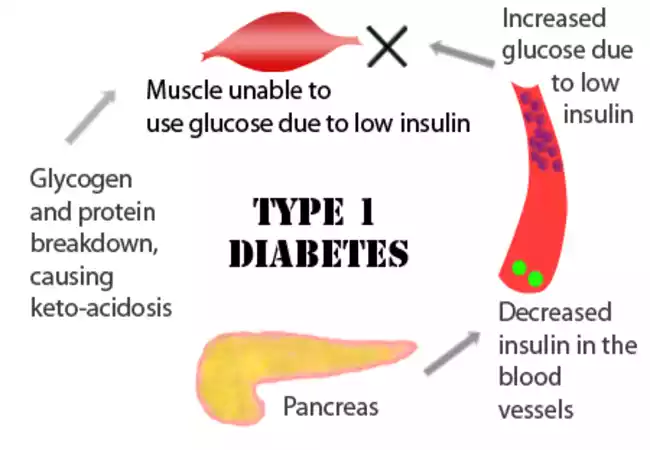
Insulin-Dependent Diabetic Mellitus, also known as Type 1 Diabetes, is an autoimmune disease that occurs when the immune system attacks and destroys the beta cells of the pancreas. This autoimmune reaction leads to a complete lack of insulin, which is a crucial hormone for controlling blood sugar levels. Type 1 diabetics must take insulin for the rest of their lives.
The IDDM has the following features:
- Onset: Type 1 diabetes is most common in childhood and adolescence.
- Autoimmune origin: Although the exact cause of Type 1 Diabetes is not known, it involves a combination of genetic susceptibility, environmental triggers, and possibly viral infections.
- Insulin Dependence: Due to the lack of insulin production in Type 1 diabetics, they must use exogenous insulin (external insulin) via insulin pumps or injections to regulate their blood sugar levels.
- Symptoms: include weight loss, fatigue, and blurred vision. These symptoms can appear suddenly.
- Blood Sugar Monitor: Frequent monitoring is necessary to adjust insulin doses, and maintain target levels.
- Complications: Type 1 diabetes, if not managed properly, can cause a variety of complications including diabetic ketoacidosis, cardiovascular disease, kidney damage, nerve damage, and vision problems.
- Treatment: Type 1 diabetes treatment focuses on tight control of blood sugar, which is often achieved through multiple daily insulin injections and insulin pump therapy. In addition to meal planning and carbohydrate counting as well as regular physical activity, these are also important in managing the disease.
- Research Advancements: Ongoing research aims to better understand the autoimmune processes that are involved in Type 1 Diabetes and develop potential cures and preventive strategies such as islet-cell transplantation or immunotherapy.
Type 1 diabetes can be a difficult condition to manage, but it is one that can be managed with constant monitoring and insulin therapy throughout life. The quality of life of people with Type 1 Diabetes continues to improve as advances in diabetes research and care continue.
A brief overview of NIDDM
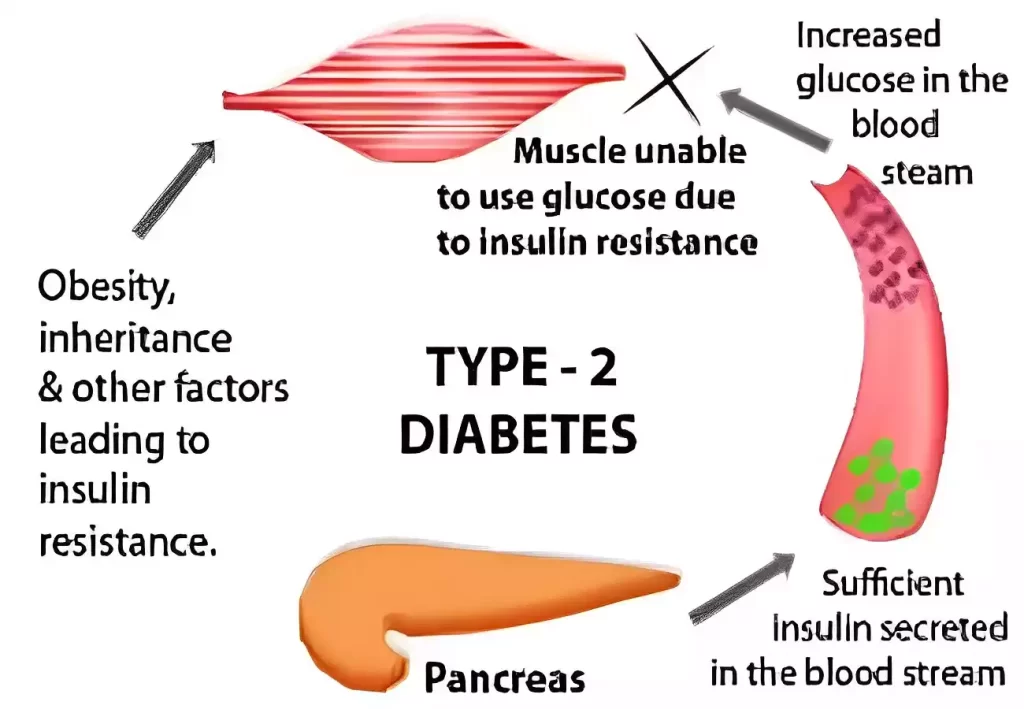
Non-Insulin-Dependent Diabetes Mellitus (NIDDM), also known as Type 2 diabetes, is a chronic metabolic disorder characterized by insulin resistance and relative insulin deficiency. Type 2 diabetes is different from Type 1 diabetes, where the immune system destroys beta cells that produce insulin. Type 2 diabetes occurs when the cells of the body become less responsive to insulin.
The NIDDM has the following features:
- Onset: Type 2 diabetes often begins in adulthood but is more common in children and adolescents due to obesity.
- Insulin Resistant: Insulin resistance means that cells in the body, such as muscles, fats, and liver cells do not respond to insulin effectively. This leads to elevated blood sugar levels.
- Risk Factors: Risk factors for type 2 diabetes include obesity and sedentary living, family history of diabetes, and ethnicity. Certain racial or ethnic groups tend to be more susceptible.
- Gradual Onset: Symptoms of type 2 diabetes usually develop slowly, and some people may be asymptomatic for years.
- Symptoms include excessive thirst (polydipsia), frequent urine (polyuria), and increased hunger (polyphagia). Other symptoms are fatigue, unexplained loss of weight, and slow healing.
- Blood Sugar Monitor: Regular blood sugar monitoring helps people with Type 2 Diabetes and their healthcare providers to make treatment adjustments.
- Treatment: Type 2 diabetes is treated by reducing blood sugar levels through lifestyle changes (diet, exercise), oral medications to improve insulin sensitivity (or stimulate insulin production), or insulin therapy.
- Complications: Type 2 diabetes, if not managed properly, can cause complications such as cardiovascular disease, kidney diseases, neuropathy, retinopathy, and peripheral arterial disease (PAD).
- Prevention: Weight loss, healthy eating habits, regular physical exercise, and quitting smoking can reduce the risk of developing Type 2 Diabetes, particularly in individuals with pre-diabetes.
- Individualized Treatment: Type 2 diabetes treatment plans are highly individualized and take into account factors such as age, health, and other medical conditions.
Type 2 diabetes can be effectively managed with lifestyle changes, medications, and early diagnosis. Regular health checkups, monitoring of blood sugar, and adherence to treatment plans are essential to long-term wellness and to reduce complications.
IDDM and NIDDM in the comparison chart
Here’s a comparison chart highlighting the key differences between Insulin-Dependent Diabetes Mellitus (IDDM), also known as Type 1 diabetes, and Non-Insulin-Dependent Diabetes Mellitus (NIDDM), also known as Type 2 diabetes:
| Characteristic | Insulin-Dependent Diabetes Mellitus (IDDM) | Non-Insulin-Dependent Diabetes Mellitus (NIDDM) |
|---|---|---|
| Onset Age | Typically occurs in childhood or adolescence | Usually diagnosed in adulthood, but also seen in children and adolescents, especially due to rising obesity rates |
| Autoimmune Origin | The immune system attacks and destroys insulin-producing beta cells in the pancreas | Insulin resistance and relative insulin deficiency; The pancreas may produce some insulin |
| Insulin Dependence | Requires lifelong insulin therapy | May not initially require insulin and may be managed with lifestyle changes and oral medications |
| Symptoms Onset | Abrupt and symptoms often develop rapidly | Gradual onset and some individuals may remain asymptomatic for an extended period |
| Body Weight | Normal or underweight at diagnosis (though can vary) | Often associated with overweight or obesity, but weight can vary |
| Blood Sugar Levels | Extremely high due to insulin deficiency | Elevated due to insulin resistance and inadequate insulin production |
| Ketosis Risk | At risk for diabetic ketoacidosis (DKA) | Less likely to develop DKA unless under severe stress or illness |
| Risk Factors | Genetics, autoimmune factors | Obesity, sedentary lifestyle, genetics, family history, age, and ethnicity are common risk factors |
| Treatment Approach | Requires insulin therapy from diagnosis | Initially managed with lifestyle modifications (diet, exercise) and may progress to oral medications or insulin |
| Blood Sugar Monitoring | Frequent monitoring, including multiple daily blood glucose checks | Monitoring is recommended but frequency may vary |
| Complications | Can develop both microvascular and macrovascular complications | Complications include cardiovascular disease, neuropathy, nephropathy, and retinopathy |
| Prevention | Not preventable due to autoimmune origin | Potentially preventable or delayed through lifestyle changes and early intervention in high-risk individuals |
Importance of distinguishing between IDDM and NIDDM
Distinguishing between IDDM (Insulin-Dependent Diabetes Mellitus) and NIDDM (Non-Insulin-Dependent Diabetes Mellitus), also known as Type 1 and Type 2 diabetes respectively, is crucial for several reasons:
- Treatment Selection: The treatment approaches for IDDM and NIDDM differ significantly. Type 1 diabetes always requires insulin therapy because it results from an absolute deficiency of insulin production. In contrast, Type 2 diabetes may initially be managed with lifestyle modifications and oral medications. Misdiagnosis or confusion between these types can lead to inappropriate treatment, potentially causing health complications.
- Disease Management: Effective management of diabetes hinges on understanding the underlying cause and physiology. People with Type 1 diabetes must carefully balance their insulin doses to maintain blood sugar within a healthy range. In Type 2 diabetes, lifestyle changes such as diet and exercise are often central to managing the condition. Confusing these two types can lead to suboptimal management.
- Risk Factors and Prevention: Recognizing the type of diabetes is essential for identifying risk factors and prevention strategies. Type 2 diabetes is strongly associated with obesity, sedentary lifestyles, and genetics. Understanding this connection can motivate individuals to make lifestyle changes to reduce their risk. In contrast, Type 1 diabetes is primarily influenced by autoimmune factors, making it less preventable but potentially manageable through early intervention.
- Education and Support: Patients with diabetes require education and support tailored to their specific type. Providing accurate information and resources can empower individuals to take control of their health. Mislabeling or misunderstanding the type of diabetes can lead to confusion and ineffective support.
- Research and Advancements: The distinction between IDDM and NIDDM is critical in research efforts to understand the causes, risk factors, and treatments for each type. Advances in diabetes care, including medications and technologies like insulin pumps or continuous glucose monitors, are driven by research specific to each type.
- Public Health Planning: Accurate classification of diabetes types is vital for public health planning and policy development. It helps in estimating the prevalence of each type, assessing healthcare resource needs, and designing targeted prevention and management programs.
- Psychological Impact: The psychological impact of living with diabetes can vary between Type 1 and Type 2 diabetes. Misclassification may lead to misunderstandings about the emotional and social aspects of the condition, affecting individuals’ well-being and mental health.
Distinguishing between IDDM and NIDDM is essential for tailoring effective treatment and management strategies, promoting prevention and education, advancing research, and providing appropriate support to individuals with diabetes.
It ensures that people receive the most appropriate care and resources for their specific condition, ultimately improving their quality of life and reducing the risk of complications.
Background Information
Diabetes mellitus is a chronic and complex metabolic disorder characterized primarily by high levels of glucose in the bloodstream. This condition is caused by a disruption of the body’s ability to regulate blood sugar, either because there is insufficient insulin produced or because insulin is not used properly.
Background information on diabetes mellitus includes:
- Insulin: Insulin is produced by the gland behind the stomach, the pancreas. Insulin’s main role is to regulate the blood sugar level by facilitating glucose uptake from the bloodstream. The cells can then use the glucose as energy or store it to be used later.
- Glucose: is the main source of energy in the cells. After eating, the digestive tract breaks down carbohydrates to glucose. This is released into the bloodstream and causes blood sugar levels to rise.
- Pancreatic function: The pancreas is a key player in diabetes. In the pancreas clusters of cells known as islets of Langerhans are responsible for producing beta cells. In Type 1 Diabetes (IDDM), the autoimmune process leads to the destruction and loss of beta cells. Type 2 diabetes (NIDDM) is characterized by normal or elevated insulin production, but cells that are resistant to it.
- Types of Diabetes Mellitus:
- Type I Diabetes (IDDM): This form is marked by an autoimmune reaction where the immune system attacks and destroys insulin-producing beta cell in the pancreas. Type 1 diabetics require insulin therapy for the rest of their lives.
- Type II Diabetes (NIDDM): Type 2 diabetes is primarily insulin resistance. Cells don’t respond effectively to insulin. The pancreas produces more insulin initially to compensate for the increased demand, but eventually, it may not be able to meet that demand. Type 2 diabetes can be caused by obesity, sedentary living, or genetic factors. Usually diagnosed in adults, but increasingly in children and teens due to the rising obesity rate.
- Diabetes Mellitus: Prevalence and Impact: Diabetes is a major global health issue. The prevalence of diabetes has steadily increased due to factors like changing diets and sedentary habits, as well as an aging population. Unmanaged diabetes can cause serious complications such as cardiovascular disease, kidney damage, nerve damage, and vision problems.
- Diabetes Management: To manage diabetes, you must keep your blood sugar within a certain range. The treatment options vary according to the type of diabetes. Treatment options may include lifestyle changes (diet, exercise), insulin therapy, blood sugar monitoring, oral medications, and in some cases, adjunct therapies such as continuous glucose monitoring devices (CGMs) and insulin pumps.
- Complications: Uncontrolled diabetes over a long period of time can cause a variety of complications including cardiovascular disease (heart attacks, strokes), kidney failure, diabetic neuropathy, diabetic retinopathy, and other problems.
It is important for healthcare professionals, patients, and the public to understand the background information about diabetes mellitus in order to prevent and manage this chronic condition. This will also help reduce the complications that are associated with it and improve health overall.
Etiology and Risk Factors
Diabetes Mellitus: Etiology and Risk factors:
Diabetes mellitus is influenced in different ways by genetics, lifestyle, and environmental factors. Understanding the etiological and risk factors of diabetes is essential for prevention and management.
This is an overview of some of the main contributors to diabetes mellitus:
Etiology:
- Genetic predisposition: Genetics play a major role in diabetes development. Individuals who have a family history are at higher risk of developing diabetes, especially Type 2. Specific genetic variations may increase diabetes susceptibility by affecting insulin action or production.
- Autoimmune factors: Type 1 diabetes is an autoimmune disorder. The body’s immune systems mistakenly target and destroy the insulin-producing pancreatic beta cells. Genetic susceptibility, as well as environmental factors, are believed to trigger autoimmunity factors.
- Triggers of Diabetes: Environmental factors can trigger diabetes, particularly Type 1 diabetes. These triggers include viral infections (particularly enteroviruses) and exposure to certain chemicals or toxins.
Risk Factors:
- Age: Type 2 diabetes (NIDDM), especially after 45 years of age, is more common. Type 2 diabetes, however, is being diagnosed at younger ages due to the rising rate of childhood obesity.
- Obesity: Obesity is an important risk factor for type 2 diabetes. Insulin resistance is caused by excess body fat. This includes abdominal fat or visceral body fat.
- Physical inactivity: A sedentary lifestyle and lack of regular exercise are linked to a higher type 2 diabetes risk. Exercise improves insulin sensitivity, which helps control blood sugar levels.
- Unhealthy diet: A diet high in processed food, sugary drinks, and saturated fats may contribute to Type 2 diabetes. A balanced diet that is rich in vegetables, fruits, and whole grains can reduce the risk.
- Gestational Diabetes: Women with gestational diabetic symptoms are at a higher risk of Type 2 diabetes in the future.
- Polycystic ovary syndrome (PCOS): Women who have PCOS, a hormonal disorder, are at a higher risk for insulin resistance and type 2 diabetes.
- Hypertension: High blood pressure is frequently associated with diabetes. Both conditions are often co-existing and have similar risk factors.
- Race & Ethnicity: Some ethnic and racial groups, including African Americans, Hispanic Americans, and Native Americans as well as Asian Americans have a greater risk of diabetes.
- Smoking: Smoking can be a risk factor for Type 2 diabetes. Smoking can cause inflammation and insulin resistance.
- Stress: Chronic stress can increase blood sugar levels, and lead to Type 2 diabetes.
Understanding the etiology of diabetes and its risk factors is important for healthcare providers, those at risk, and public health initiatives. Early intervention and prevention strategies focus on lifestyle changes and regular screenings. Genetic counseling is also offered to those with a history of diabetes.
Diagnosis and Diagnostic Criteria
The diagnosis of diabetes mellitus includes a blood sugar test and, in certain cases, additional tests that confirm the type. The diagnostic criteria vary slightly for Type 1 (Insulin-Dependent Diabetes Mellitus, IDDM) and Type 2 (Non-Insulin-Dependent Diabetes Mellitus, NIDDM) diabetes.
Diagnosis Type 1 Diabetes:
- Symptoms: The presence of classical symptoms of diabetes such as excessive urination, polydipsia, unexplained loss of weight, and fatigue.
- Random Blood Sugar Test: A random blood sugar test regardless of time, indicating a level greater than 200 milligrams/deciliter (mg/dL), along with symptoms.
- Fasting Blood Glucose Test: A blood glucose test performed after a fast of at least eight hours. Two separate results of 126mg/dL confirm diabetes.
- Oral Glucose tolerance test (OGTT): Blood glucose levels are measured in an OGTT after fasting, and again after two hours of consuming a standardized sugar solution. Diabetes is confirmed by a blood glucose level greater than 200 mg/dL at the 2-hour mark.
- Test: For Glycated Hemoglobin HbA1c: A level of 6.5% and higher indicates diabetes. HbA1c is a measure of average blood sugar over the last two to three month.
In the case of severe symptoms and hyperglycemia, a random blood glucose test can be used to diagnose the condition.
Diagnosis Type 2 Diabetes:
- Fasting Blood Glucose Test: A blood glucose test performed after a fast of at least eight hours. Two separate results of 126mg/dL confirm diabetes.
- Oral Glucose tolerance test (OGTT): An OGTT may be used if the diagnosis of Type 2 diabetes is unclear. A blood glucose reading of 200 mg/dL at the 2-hour mark confirms diabetes.
- Test: for Glycated Hemoglobin HbA1c: A level of 6.5% or more confirms diabetes. As with Type 1 Diabetes, HbA1c is a measure of average blood sugar over the last two to three months.
- Random Blood Glucose test: A random blood glucose level of 200mg/dL and higher, along with the presence of classic diabetes symptoms confirms a diagnosis of Type 1 diabetes.
- Risk factors: Healthcare providers may conduct blood sugar tests for individuals who have risk factors for Type 2, such as obesity, a family history of diabetes, or a sedentary lifestyle, even if they do not experience symptoms.
To minimize the possibility of false positives, it’s important that you make a diagnosis based on results from two different tests. In cases of uncertainty, healthcare providers can also use other tests to differentiate between Type 1 diabetes and Type 2 Diabetes, including the measurement of autoantibodies, such as GAD antibodies.
Diabetes is a serious condition that can have severe consequences. It’s important to diagnose and manage diabetes early in order to prevent complications and improve health outcomes. Individuals with diabetes risk, and especially those who have risk factors, need to undergo regular screenings, as prescribed by their healthcare provider.
Treatment Approaches
Treatment Options for Diabetes Mellitus:
Management of diabetes mellitus aims to improve overall health, control blood sugar, and prevent complications. Treatment depends on factors such as the type and severity of diabetes.
Here are the key treatment approaches for both Type 1 (Insulin-Dependent Diabetes Mellitus, IDDM) and Type 2 (Non-Insulin-Dependent Diabetes Mellitus, NIDDM) diabetes:
Type I Diabetes (IDDM):
- Insulin Therapy: Insulin therapy is required for life by people with Type 1 Diabetes, as their bodies don’t produce insulin. Insulin can be administered by insulin pumps or injections. Treatment plans can include:
- Insulin basal: Long-acting, to maintain a constant level of insulin in the blood.
- Bolus insulin is a rapid-acting insulin that can be taken before meals to help control the blood sugar spikes after meals.
- Correction doses: Additional Insulin to correct high blood glucose levels.
- Blood Sugar Monitoring: Frequent monitoring of blood glucose is necessary to adjust insulin dosages and maintain target blood sugar levels. This can be achieved using glucose meters or continuous monitoring devices (CGM).
- Carbohydrate Calculation: Type 1 diabetics often count carbohydrates to determine the insulin dosage and match it with the carbohydrate intake in their meals and snacks.
- Meal planning: A balanced meal plan, with an emphasis on carbohydrate control, is essential to managing blood sugar. A registered dietitian will help you create a meal plan that is right for you.
Type 2 diabetes (NIDDM):
- Lifestyle Modifications:
- Diet: Adopting an eating plan that emphasizes whole grains, vegetables, and fruits, as well as lean protein, while limiting processed foods and sugars.
- Exercise: Regular physical activity such as walking, cycling, swimming, or swimming to improve insulin sensitivity. At least 150 minutes of moderate-intensity exercise should be done per week.
- Weight Control: Maintaining a healthy body weight and achieving it through diet and physical activity can improve blood sugar levels.
- Oral Antidiabetic Medicines: Many people with Type 2 Diabetes may need oral medications to reduce blood sugar levels. They may increase insulin sensitivity, stimulate insulin production, or reduce glucose production by your liver.
- Injectable Medicines: Some individuals with Type 2 Diabetes may require injectable medications such as insulin or glucagon-like peptide-1 receptor agonists (GLP-1R).
- Blood glucose Monitoring: Regular monitoring of blood sugar levels is recommended, particularly for those who take medications that may cause hypoglycemia.
- Monitoring Glycated hemoglobin (HbA1c): Monitoring levels of HbA1c helps to assess long-term control of blood sugar and guide treatment adjustments.
- Support and Education: Diabetes Self-Management Education (DSME) can empower individuals to make educated choices about their health and manage it effectively.
- Routine Healthcare Checkups: Routine healthcare checkups are important for managing diabetes. They monitor your overall health and address any complications.
- Cardiovascular Risk Management: Managing cardiovascular risks like high blood pressure or cholesterol is important since diabetics are at a higher risk for heart disease.
Healthcare providers should review and adjust treatment plans for both types. The goal of diabetes management is to keep blood sugar within a certain range, avoid complications, and improve overall quality. Healthy eating and regular exercise are essential components of diabetes management. Medication and insulin are tailored to the type of disease and its progression.
Long-term Complications
When blood sugar levels are elevated for a prolonged period of time and poorly controlled, long-term complications can occur. These complications can cause serious health problems and affect different organ systems.
To reduce the risk of complications, it’s important that people with diabetes manage their condition well. Here are some of the long-term complications associated with both Type 1 (Insulin-Dependent Diabetes Mellitus, IDDM) and Type 2 (Non-Insulin-Dependent Diabetes Mellitus, NIDDM) diabetes:
Microvascular Complications:
- Diabetic Retinopathy: Damage to blood vessels within the retina may lead to vision issues, including blindness if untreated. Early detection and treatment of diabetic retinal disease requires regular eye examinations.
- Diabetic Nephropathy: Over time, high blood sugar levels damage the kidney’s filtration system. This can lead to kidney disease or even kidney failure. Early intervention requires regular monitoring of kidney functions.
- Diabetic Neuropathy: Nerve damage can cause tingling and numbness in the extremities. In severe cases, foot ulcers can develop and there is a risk of amputation.
Macrovascular complications:
- Cardiovascular Disease: People with diabetes are at an increased risk for heart disease. This includes coronary artery diseases, heart attacks, and strokes. To reduce this risk, it is important to manage blood pressure, cholesterol, and blood sugar.
- Peripheral Artery Disease: PAD is a condition where there is reduced blood flow in the extremities. This can cause leg pain, slow wound healing, and, in severe cases, even amputation.
- Cerebrovascular Disease: Diabetes can increase the risk of strokes. Strokes can be fatal or cause severe neurological impairments.
Other Complications:
- Hyperglycemia: Episodes of low sugar (hypoglycemia), can cause confusion, dizziness, and fainting. In severe cases, seizures may occur or the person will lose consciousness. Maintaining blood sugar levels can prevent hypoglycemic episodes.
- Hyperglycemic hyperosmolar state (HHS): This condition is primarily associated with Type 2 Diabetes when blood sugar levels are extremely high. It can lead to confusion, dehydration, and even coma.
- Infections & Wound Healing: High blood sugar levels can affect the immune system, causing frequent infections and delayed healing.
- Dental Problems: Diabetes increases the risk of gum disease, tooth loss, and other dental issues.
- Sexual Dysfunction: Both men and women with diabetes can experience sexual dysfunction. This includes erectile dysfunction in men and reduced libido in women.
- Mental health issues: Diabetes can be emotionally difficult and can contribute to mental illnesses such as depression or anxiety.
While diabetes can increase the risk of complications, proper management including blood sugar control and lifestyle changes, medication adherence, and regular medical checks, can prevent or delay their development. When complications do occur, early detection and intervention are crucial.
Diabetes patients should develop a comprehensive plan of care with their healthcare provider that addresses risk factors and prevents or mitigates long-term complications.
Prognosis
There are several factors that can affect the prognosis of a person with diabetes mellitus. These include the type of diabetes and its severity, as well as the overall health of the individual, and any complications.
Here’s an overview of the prognosis for both Type 1 (Insulin-Dependent Diabetes Mellitus, IDDM) and Type 2 (Non-Insulin-Dependent Diabetes Mellitus, NIDDM) diabetes:
Type I Diabetes (IDDM):
- A Lifelong Condition: Type 1 diabetes requires lifelong insulin therapy. Although there is no cure for type 1 diabetes, the right management can help individuals lead healthy lives.
- Life expectancy: Type 1 diabetics can live a life that is similar to the average population if they are well-managed and avoid complications.
- Complications: Diabetes-related complications can have a significant impact on the prognosis. Early intervention, regular monitoring, and proper blood sugar control can help reduce complications and improve long-term outlook.
- Risk of Hypoglycemia: A severe episode of hypoglycemia can be fatal. It is important to have a careful management plan and educate yourself on how to recognize and treat low blood sugar.
Type 2 diabetes (NIDDM):
- Chronic condition: Type 2 diabetes, like Type 1, is a chronic disease that can be managed with lifestyle changes, oral medication, and in some cases insulin therapy.
- Life expectancy: Type 2 diabetics who are well-managed can live a life similar to that of those without diabetes. Poor management and complications can decrease life expectancy.
- Complications: The presence of complications has a strong influence on the prognosis. Heart disease, renal disease, and peripheral arterial disease are all common complications that can have a negative impact on long-term health.
- Lifestyle changes: A healthy diet, regular exercise, weight control, and quitting smoking can improve the prognosis of individuals with type 2 diabetes.
- Insulin and Medication: Some people with type 2 diabetes will eventually need insulin therapy, particularly if other treatments fail to control their blood sugar. It is important to adhere to insulin and prescribed medication regimens for a long-term healthy life.
- Prevention & Early Intervention: Early detection, prevention strategies, and prompt intervention are important for improving the outlook of Type 2 diabetes.
Diabetes management is highly individual. Prognosis can differ widely between people depending on factors such as genetics, lifestyle, healthcare access, and adherence.
Regular monitoring, diabetes self-management training, and a partnership with healthcare providers are all ways to help people with diabetes minimize complications and achieve better outcomes. Diabetes is manageable and many people with diabetes live healthy and full lives with the right care.
Conclusion
Diabetes mellitus can be a complex, but manageable, condition. It requires regular medical attention, careful blood sugar management, and lifestyle changes. Early diagnosis and management can improve the outlook for diabetics, helping them lead healthy and fulfilling lives.
To achieve the best outcomes for diabetes management, it’s important to work closely with your healthcare provider, follow treatment plans, and make positive life changes.
