Osteoporosis, a common skeletal condition, is characterized by the thinning of bones. This leads to an increased fracture susceptibility and fragility. It is broadly divided into two types: primary and secondary osteoporosis.
Understanding the differences between the two types of osteoporosis is essential for accurate diagnosis, treatment, and prevention. This overview will examine the causes, definitions, and differences between primary and secondary Osteoporosis.
Definition of Osteoporosis
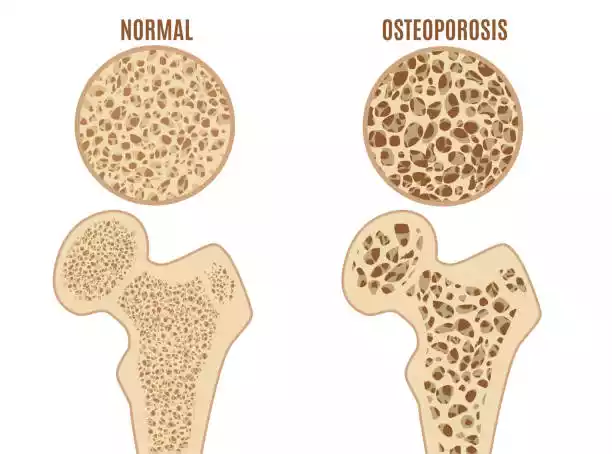
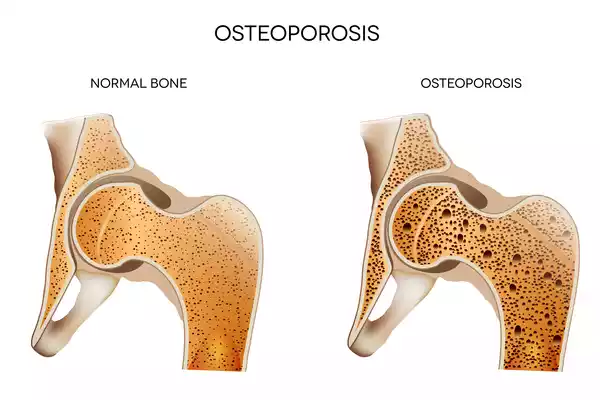
Osteoporosis, also known as osteoporosis, is a condition that causes the bones to gradually weaken and thin. This results in a reduced bone density. It can also increase fracture susceptibility. Osteoporosis causes the bones to become porous and fragile, which makes them more susceptible to breaking even under minimal stress or trauma.
The condition can progress silently, without any obvious symptoms, until it leads to a fracture, usually in the hip, spine, or wrist. Osteoporosis can be a serious health issue, especially for the elderly. Fractures can cause serious complications, and reduce quality of life.
Primary Osteoporosis
The term primary osteoporosis is used to describe a form of osteoporosis that occurs without any other medical conditions or factors. Age, hormonal changes, and genetics are the main factors. Postmenopausal and older women are more likely to develop primary osteoporosis. There are two subtypes of osteoporosis.
- Osteoporosis Type 1 (Postmenopausal Osteoporosis):
- This condition is most common in women who have experienced menopause.
- Estrogen is essential for maintaining bone density. Its decrease during menopause can lead to an accelerated loss of bone.
- Common outcomes include increased bone fragility and increased susceptibility to fractures.
- Osteoporosis Type 2 (Senile Osteoporosis):
- It affects both men and women. However, it is more common in individuals over 70 years old.
- The age-related loss of bone is due to a decrease in bone formation, and changes in the remodeling process.
- As we age, our bone density decreases, and the risk of fracture increases.
Smoking, diet, and physical activity can have a significant impact on bone health in both primary osteoporosis types. Correct diagnosis, regular monitoring, and lifestyle changes can reduce the risk of fractures and manage primary osteoporosis. In high-risk patients, treatment may include medication to prevent bone loss and strengthen the bones.
Risk Factors
The risk factors for osteoporosis are varied, including age, gender, and genetics.
Here are some risk factors that you may encounter:
- Age: The risk for primary osteoporosis rises with age, especially in senile osteoporosis. Bone density decreases as people age.
- Gender: Women have a greater risk of osteoporosis than men. This is primarily because estrogen levels drop during and after the menopause. Men can also get osteoporosis but usually later in life.
- Family history: An increased risk of fractures or osteoporosis can be attributed to a genetic predisposition.
- Hormonal Changes :
- Menopause: The hormonal change associated with menopause and the reduction in estrogen accelerates bone loss among women.
- Low testosterone: A low level of testosterone in men can cause bone loss, and increase the risk of osteoporosis.
- Nutrition and Diet:
- Low calcium intake: Diets lacking in calcium will weaken the bones over time.
- Vitamin D Deficiency: Vitamin D deficiency can cause calcium absorption to be hindered and bone loss.
- Physical activity: Sedentary lifestyles or a lack of weight-bearing exercises can increase osteoporosis risk. Weight-bearing exercises help maintain bone density.
- Smoking: Smoking can lead to lower bone density, slower healing, and fractures.
- Alcohol consumption: An excessive amount of alcohol can reduce bone density and interfere with calcium absorption.
- Use of Corticosteroids: The long-term use of corticosteroid medication can cause bone loss, and increase the risk of osteoporosis.
- Some Medical Conditions: Certain medical conditions, such as rheumatoid, celiac, Crohn’s, and hyperthyroidism, can cause bone loss.
- Low body weight: A small frame or being underweight can increase your risk of osteoporosis because there is less bone density to begin with.
- Race/Ethnicity: Certain ethnic groups such as Caucasians or Asians have a greater risk of osteoporosis.
- Fractures Prior: Previous fragility fractures increase the risk of future fractures.
These risk factors may increase your chances of developing osteoporosis but they don’t guarantee it. Most cases of osteoporosis can be prevented or managed through lifestyle changes, nutrition, and, if necessary, medical intervention. Consult a healthcare professional if you have multiple risk factors, or if you are concerned about your bone health.
Secondary Osteoporosis
It is not a condition that is caused by hormonal fluctuations or age alone. This condition is usually associated with specific risk factors and causes that lead to bone loss.
Here are some key aspects of secondary osteoporosis:
- Underlying medical conditions: Secondary osteoporosis can be caused by a variety of medical conditions:
- Hormonal Disorders: Conditions such as hyperthyroidism and hyperparathyroidism can affect the hormonal balance required to maintain bone density.
- Gastrointestinal Diseases: Malabsorption disorders, such as celiac, can cause bone loss by preventing calcium and vitamin D absorption.
- Chronic kidney disease: Impaired renal function can affect bone health by affecting the ability of the body to regulate calcium and phosphorus levels.
- Rheumatic Diseases: Rheumatic diseases such as systemic lupus and rheumatoid arthritis can cause chronic inflammation of the bones and joints.
- Medications: Some medications have been known to cause secondary osteoporosis. Long-term use includes:
- Corticosteroids: These medications, which are commonly prescribed to treat conditions such as asthma, rheumatoid arthritis, and autoimmune disease, can cause bone weakness over time.
- Anticonvulsants: Certain medications used to treat seizures and epilepsy may interfere with calcium absorption.
- Proton pump inhibitors (PPIs): The long-term use of PPIs for acid reflux, stomach ulcers, and other conditions can increase the risk of fractures.
- Lifestyle Factors: Lifestyle choices can influence secondary osteoporosis.
- Alcohol and Bone Health: Heavy drinking for a long time can be harmful.
- Smoking and Bone Density: Smoking has been associated with lower bone density.
- Poor nutrition: An inadequate intake of calcium and Vitamin D can lead to bone loss.
- Immobility: Prolonged inactivity due to paralysis or sedentary living can cause muscle and bone weakness.
- Age and Gender: Although primary osteoporosis affects more women after menopause, secondary osteoporosis may affect anyone, regardless of age or gender.
- Fractures: People who have suffered from fragility fractures in the past may be more susceptible to secondary osteoporosis.
In order to diagnose and manage secondary osteoporosis, it is important to address the underlying medical conditions, modify medications, and implement lifestyle changes as well as medications that improve bone density. Individuals with secondary osteoporosis must work closely with healthcare providers to identify and effectively manage the root cause.
Causes and Risk Factors
Secondary osteoporosis is caused by a variety of factors, including underlying medical conditions and medications. Lifestyle choices and other lifestyle choices can also contribute to bone loss. Understanding these risk factors is essential for identifying those at high risk and treating the condition effectively.
These are the most common causes and risk factors for secondary osteoporosis:
- The underlying medical conditions: a. Hormonal Dysfunction:
- Hyperthyroidism: An overactive gland of the thyroid can cause excessive bone resorption, resulting in weakened bones.
- Hyperparathyroidism: An overproduction of parathyroid hormonal can cause calcium loss in the bones.
- Cushing’s Syndrome: Elevated cortisol levels, usually due to a tumor, can cause bones to weaken.
b. Gastrointestinal Disorders:
- Inflammatory Bowel Disease: Conditions such as Crohn’s Disease and Ulcerative Colitis can reduce the absorption of nutrients, including calcium and Vitamin D.
- Celiac Disease: Gluten intolerance may lead to malnutrition.
Chronic kidney disease: A dysfunctional kidney can affect the balance of calcium and phosphorus, which in turn will affect bone health.
Autoimmune and Rheumatic Conditions
- Rheumatoid Arthritis: This autoimmune disease causes chronic inflammation that can affect the bones and joints.
- Systemic Lupus Erythematosus: SLE may cause bone loss as a result of inflammation and medication side effects.
- Medicines Corticosteroids: Long-term corticosteroid use, such as the medication prednisone can lead to bone loss and an increased risk of fractures.b. Anticonvulsants: Some drugs that treat epilepsy or seizures can interfere with calcium metabolism.Proton pump inhibitors (PPIs): The long-term use of PPIs for acid reflux and stomach ulcers may reduce calcium absorption.
- Lifestyle Factors Alcoholism: Heavy drinking for a long time can have a negative impact on bone health.b. Smoking: Smoking has been associated with a lower bone density, and a reduced ability to heal bones.Low body weight: Underweight or a small frame can increase the risk for secondary osteoporosis.Inactivity: Lack of weight-bearing exercise and prolonged inactivity can lead to loss of bone.
- Age and Gender: Secondary Osteoporosis may affect people of any gender or age, depending on its underlying cause. Some conditions are more common in certain populations.
- Fractures: People who have suffered from fragility fractures may be more susceptible to secondary osteoporosis as they can indicate compromised bone health.
- Family history: If you have a family history of fragility fractures or osteoporosis it may increase your risk of secondary osteoporosis. This is especially true if genetic factors play a role.
- Dietary factors: An inadequate intake of calcium and Vitamin D in the diet may contribute to secondary osteoporosis.
- Menstrual irregularities: Hormonal imbalances can affect bone health in females with irregular or absent cycles.
- Side effects of medications: Certain medications used to treat medical conditions can have side effects that damage bones.
It is important to identify the cause of secondary osteoporosis or the combination of causes that contribute to it. This will allow for effective treatment and management. Diagnostic tests, medical histories, and evaluations are used by healthcare providers to identify the underlying causes of secondary osteoporosis and to develop a customized plan to optimize bone health.
Diagnosis
The diagnosis of osteoporosis is based on a combination of clinical evaluations, imaging studies, and testing for bone density. The diagnostic process is used to assess bone health and the risk of fracture.

These are the main steps and methods for diagnosing osteoporosis:
- Medical History and Physical Examen:
- The healthcare provider will begin by taking a medical history. This includes any risk factors and family history of osteoporosis. They will also review current medications.
- You may need to perform a physical exam to check your posture and height and for signs of vertebral injuries.
- Fracture Assessment:
- Identify any fragility fractures in the spine or hips.
- Bone Density Test:
- Dual-Energy-X-Ray Absorptiometry, or DEXA: This is the method most commonly used to measure bone density. The test measures bone mineral density at the hips and spines, generating a T-score that compares a person’s BMD with that of an average young adult. The T-score is used to classify bone density into normal, osteopenia, or osteoporosis.
- DXA can be used to measure bone density in peripheral bones such as the heel, wrist, or finger.
- Lab Tests:
- Tests of calcium, phosphate, and vitamin D levels, as well as markers of bone turnover, can be performed.
- Tests for thyroid, parathyroid, and sex hormonal levels may be performed, particularly in cases where secondary osteoporosis is suspected.
- Vertebral Imaging:
- X-rays, CT scans, or MRIs can be used to detect deformities or fractures in the vertebrae that may result from osteoporosis.
- FRAX Tool:
- The FRAX is a fracture risk assessment tool that calculates an individual’s risk over a 10-year period of suffering a major fracture (e.g. hip, spine, or wrist). The calculator takes into account multiple factors such as age, gender, BMD, and prior fractures.
- Secondary Osteoporosis Assessment:
- Additional investigations may be required to determine the medical condition underlying the bone loss if secondary osteoporosis has been suspected on the basis of the clinical evaluation or test results.
- Assessing Lifestyle Factors:
- Assessing lifestyle factors such as physical activity, diet, alcohol, and smoking can help identify modifiable risks.
- Patient history and risk factor assessment:
- A history of falls may be asked of patients, since a history can increase the risk of fractures, particularly in older adults.
- DXA Monitoring:
- If osteoporosis is diagnosed, regular DXA scans can be recommended to assess the treatment effectiveness and monitor any changes in bone density.
A comprehensive evaluation that includes bone density tests and an assessment of possible underlying causes allows healthcare providers to make an accurate diagnosis and determine the best treatment and prevention measures. Early diagnosis is crucial for fracture prevention and effective management.
Primary and Secondary Osteoporosis in the comparison chart
Here’s a comparison chart outlining the key differences between primary and secondary osteoporosis:
| Characteristic | Primary Osteoporosis | Secondary Osteoporosis |
|---|---|---|
| Definition | Age-related or hormonal bone loss is not associated with underlying medical conditions or medications. | Result of underlying medical conditions, medications, or other factors that contribute to bone loss. |
| Age of Onset | Typically occurs in postmenopausal women and older adults. | Can occur at any age, depending on the underlying cause or condition. |
| Etiology | Mainly influenced by age, genetics, gender, and hormonal changes (e.g., menopause). | Caused by specific medical conditions, medications, or lifestyle factors. |
| Risk Factors | – Aging – Gender (more common in women) – Family history – Hormonal changes – Genetics – Lifestyle factors (e.g., diet, physical activity) | – Underlying medical conditions – Medications (e.g., corticosteroids, anticonvulsants) – Hormonal disorders – Gastrointestinal disorders – Lifestyle factors (e.g., alcohol, smoking) |
| Pathophysiology | – Hormonal changes (e.g., estrogen decline in postmenopausal women) – Altered bone remodeling process – Reduced bone density | – Underlying medical conditions disrupt bone health – Medications may interfere with bone metabolism – Inflammation and other factors contribute to bone loss |
| Clinical Presentation | – Increased fracture risk, particularly in hip, spine, and wrist – Often asymptomatic until fractures occur | – Increased fracture risk associated with underlying condition – Symptoms of the underlying condition may be present |
| Diagnosis | – Bone density testing (DXA) – Fracture risk assessment – Clinical evaluation – Medical history | – Bone density testing (DXA) – Identification of underlying condition – Medication history – Clinical evaluation |
| Treatment and Management | – Lifestyle modifications (e.g., diet, exercise) – Medications to strengthen bones (e.g., bisphosphonates) – Fall prevention strategies | – Address underlying medical condition – Medication adjustment, if possible – Lifestyle modifications – Medications to improve bone density – Fall prevention strategies |
| Prevention | – Lifestyle changes (e.g., calcium, vitamin D, exercise) – Early detection and management | – Managing underlying medical conditions – Medication management – Lifestyle changes to support bone health |
| Prognosis | – Good prognosis with early intervention and management – Fracture risk reduction with treatment | – Prognosis depends on the underlying condition – Management may involve ongoing treatment and monitoring |
This chart highlights the fundamental distinctions between primary and secondary osteoporosis, emphasizing their causes, risk factors, clinical presentation, and management strategies. Understanding these differences is essential for healthcare providers to make accurate diagnoses and provide appropriate care to patients.
Importance of Understanding Primary and Secondary Osteoporosis
There are several important reasons why it is important to understand primary and secondary osteoporosis:
- Accurate Treatment and Diagnosis: It is important for healthcare providers that they make an accurate diagnosis. This helps to determine the best treatment strategy. Secondary osteoporosis is often treated differently than primary osteoporosis.
- Effective Preventive: By understanding the causes and risk factors of primary and secondary osteoporosis, individuals can take preventive action. Early intervention, lifestyle modifications, and dietary changes can help reduce the risk of osteoporosis.
- Customized care: Understanding the underlying cause of secondary osteoporosis allows healthcare providers to tailor their treatment. It is important to address the specific medical condition, or side effects of medication that are contributing to bone loss. This will ensure that patients receive effective treatment.
- Fracture prevention: Osteoporosis can lead to serious fractures and have serious consequences for the elderly. Understanding osteoporosis and its associated risk factors will help healthcare providers implement fracture prevention strategies. This will reduce the burden fractures place on patients and healthcare systems.
- Improved Outcomes: Early diagnosis and proper management of osteoporosis may lead to better patient outcomes. Early treatment can improve the quality of life and maintain bone density for those with osteoporosis.
- Cost reduction: By identifying and treating osteoporosis, both primary and secondary, effectively, healthcare systems may be able to reduce the financial burden of osteoporosis-related fractures, hospitalizations, and long-term care.
- Research and Development: A clear understanding of primary and secondary osteoporosis helps to direct research efforts. Researchers can concentrate on developing specific treatments for osteoporosis types and better strategies to prevent bone loss.
- Empowering Patients: Patients who understand their condition, and the underlying causes of it, are more likely to be involved in their own healthcare. Knowing about osteoporosis helps individuals make informed decisions regarding their lifestyles, medications, and treatment options.
- Public Health Initiatives: Public health initiatives that aim to prevent and manage osteoporosis will benefit from an understanding of the primary and secondary forms. This knowledge can be used to develop educational programs and policies that promote bone health.
It is important to distinguish between primary and secondary Osteoporosis for accurate diagnosis, tailored treatment, and effective prevention. This leads to improved patient outcomes, cost-savings, and advances in research and public health to combat this common bone disease.
Treatment and Management
Treatment and management of osteoporosis are focused on improving bone health, strengthening bones, and reducing fracture risks. Treatment options can vary depending on osteoporosis type, underlying causes, and patient characteristics.

The following are the key elements in osteoporosis treatment and management:
1. Lifestyle Modifications:
- Dietary changes: Make sure you are getting enough calcium and vitamin D in your diet or through supplements. Dairy products, leafy vegetables, and fortified food are all calcium-rich foods. Vitamin D is obtained through sunlight, supplements, or certain foods.
- Weight Bearing Exercise: Do regular weight-bearing exercises such as walking or jogging. You can also do resistance training and dance. These activities stimulate bone formation and help maintain bone density.
- Fall prevention: Implement strategies for fall prevention to reduce fracture risk. Remove tripping hazards from your home.
- Quit Smoking and Limit Alcohol Consumption: Alcohol and smoking can have a negative impact on bone health.
2. Medications:
- Bisphosphonates: These drugs such as alendronate or risedronate are commonly prescribed for reducing bone resorption and increasing bone density. These drugs are commonly prescribed for primary and secondary osteoporosis.
- Hormone Replacement (HRT): Estrogen, or a combination of estrogen and progestin, may be prescribed for postmenopausal women to prevent bone loss. HRT is rarely used to treat secondary osteoporosis.
- Selective estrogen receptor modulators (SERMs): Medication like raloxifene mimics estrogen’s effects on bone protection in postmenopausal women without the risk associated with HRT.
- Teriparatide and Abaloparatide are drugs that stimulate bone formation: They are only prescribed for severe osteoporosis cases or when other treatment options are not effective.
- Denosumab: A monoclonal antibody that can be used to treat bone resorption when other treatments do not work.
- Calcitonin: is an alternative medication that can reduce the pain of vertebral fractures, and also inhibit bone resorption.
- Medication Modification: In cases of secondary osteoporosis it may be necessary to adjust or discontinue medications that contribute to bone loss.
3. Monitoring:
- It is important to schedule regular follow-up appointments in order to monitor the treatment’s effectiveness and make any necessary adjustments. To assess any changes in bone density, repeat the DXA test.
4. Nutrition and Supplements:
- Maintaining bone health requires adequate nutrition, which includes calcium and vitamin D. If dietary intakes are insufficient, supplements may be prescribed.
5. Preventing Falls:
- Use strategies to avoid falls, particularly in older adults. Included in this are home safety modifications and vision tests, as well as balance exercises.
6. Management of Underlying Conditions:
- In secondary osteoporosis cases, the primary focus is on managing the medical condition that contributes to bone loss. It may be necessary to work with specialists in order to treat the condition.
7. Patient Education:
- Information about osteoporosis and its management strategies will empower patients to take an active role in their own care and adopt lifestyle changes that promote bone health.
The treatment and management plan should be tailored to the specific needs of each patient, their risk factors, and the underlying causes of osteoporosis. The healthcare providers are crucial in diagnosing osteoporosis, developing treatment plans, and optimizing bone health to reduce fracture risk.
Prevention Strategies
It is important to prevent osteoporosis in order to maintain strong, healthy bones for the rest of your life.
The following strategies will help you reduce your risk of developing osteoporosis:
1. Calcium intake:
- Foods rich in calcium include dairy products, leafy vegetables, fortified food (e.g. fortified orange juice, cereals), and fish that have edible bones.
- If your calcium intake is not sufficient, you may want to consider taking supplements. To determine the correct dosage, consult your healthcare provider.
2. Take Vitamin D to the Recommended Level:
- Vitamin D is essential for calcium absorption. Sunlight exposure, dietary sources such as fatty fish and fortified milk products, or supplements, if needed, are all ways to ensure you get enough vitamin D. For vitamin D recommendations, consult your healthcare provider.
3. Weight-bearing exercises:
- Weight-bearing exercises, such as walking or jogging, and dancing, along with strength training and weight-bearing exercises can help maintain bone strength and density. At least 150 minutes per week of moderate-intensity aerobic exercise, including weight-bearing activities, is recommended.
4. Quit Smoking:
- Smoking can lead to a decrease in bone density and an increased risk of fractures. Smoking is not only harmful to your bones, but it also affects your overall health.
5. Limit Alcohol Consumption:
- Excessive alcohol intake can weaken bones. Moderation is key if you plan to consume alcohol. The recommended limit is different in each country, but it’s generally one drink for women per day and two for men.
6. Maintain a Healthy Weight:
- Underweighting increases your risk of osteoporosis. To achieve a healthy weight, eat a balanced diet and exercise regularly.
7. Avoid Falls:
- Falls are one of the leading causes of fractures among older adults. Reduce the risk of falling:
- Keep your home lit and clear of tripping hazards.
- Handrails are essential on stairs and in bathrooms.
- Strengthening and balance exercises can help you improve your stability.
- Regularly check your eyesight
8. Medication Management:
- Discuss with your doctor alternative options or prevention measures if you take medications that can cause bone loss, such as corticosteroids.
9. Bone Health Assessment:
- Consider bone density testing to determine your bone health if you are at risk for osteoporosis. This can be used to identify early signs and preventive measures of bone loss.
10. Work with your healthcare provider to treat and manage underlying medical conditions:
11. Medication for High-Risk Individuals: In certain cases, healthcare professionals may recommend osteoporosis medication for individuals who are at high risk. This includes postmenopausal women with multiple risk factors or women who have experienced fragility fractures.
12. Consult your healthcare provider: Consult with your healthcare provider for personalized advice on osteoporosis. This is especially important if you are at risk or have a medical condition.
Osteoporosis is preventable by maintaining good bone health throughout your life. These strategies can reduce your risk of developing osteoporosis, and the associated fractures.
Complications and Prognosis
Osteoporosis may lead to a variety of complications, especially if left untreated or when fractures are present. The prognosis and complications of osteoporosis are dependent on factors like the severity of the bone loss, fractures present, the effectiveness of the treatment, and the individual’s health status.
Below are some of the potential complications associated with osteoporosis and their prognosis:
1. Osteoporosis increases the risk for fractures.
- Disability and Pain: A hip fracture can lead to severe pain and disability.
- Loss Of Independence: Hip injuries, in particular, can lead to a loss of independence as the individual may need assistance in daily activities.
- Reduced Life Quality: Chronic pain and limited mobility can have a negative impact on a person’s life quality.
- Mortality: Hip fractures are associated with a higher risk of death due to complications, such as blood clots and pneumonia.
2. Vertebral fractures: These can cause complications, such as:
- Kyphosis Multiple vertebral breaks can cause the spine’s curve to forward, resulting in a stooped position known as kyphosis.
- Reduced lung capacity: A severe kyphosis may reduce lung capacity, increasing the risk of respiratory issues.
3. Limited Mobility: Fractures and pain can cause limited mobility. This can lead to muscle weakness and loss of balance. Falls are also more likely.
4. Psychological Impact: Physical limitations and pain caused by osteoporosis or fractures may have psychological effects, such as depression and anxiety.
5. Complications of Treatment: Some medications for osteoporosis may cause side effects or complications. With a healthcare provider, it is important to discuss the risks and benefits of treatment.
6. Prognosis:
- The prognosis of osteoporosis depends on many factors, including age, health, and the effectiveness of prevention and treatment strategies.
- A timely diagnosis and the appropriate treatment can improve prognosis. Treatment can improve the quality of life, decrease fracture risk, and maintain or increase bone mass.
- Exercise, calcium-rich foods, and fall prevention can all improve your prognosis.
- It is important to monitor and follow up with your healthcare provider regularly in order to determine the effectiveness of treatment and make any necessary adjustments.
- Addressing the underlying medical conditions can improve bone health and prognosis in cases of secondary osteoporosis.
Osteoporosis can be managed and people with the condition can live active, fulfilling lives if they receive proper treatment and diagnosis. Early intervention and lifestyle changes are key to reducing complications and improving prognosis in individuals with osteoporosis.
Conclusion
Osteoporosis, a condition that can be debilitating and is often common, is characterized by weak bones. This increases the risk of fractures. Understanding the causes, risks, prevention strategies, and treatments available is crucial for maintaining bone health, whether it’s primary or secondary.
Early diagnosis and proactive treatment are essential to reduce complications and improve the quality of life of individuals living with or at risk of osteoporosis.
