The foremost noteworthy differentiator of A1c from a glucose test is the truth that A1c speaks to the sum of glycosylated hemoglobin (hemoglobin which is bound by glucose) in blood. Glucose is a blood sugar test that is fasting that is performed using the glucose glucometer.
In the presence of glucose urine is a sign that you have the presence of diabetes. Checking your blood sugar can uncover whether you have got prediabetes or the sort 2 frame of diabetes. Prediabetes is the beginning step within the advancement of Sort 2 Diabetes. Prediabetes as well as type 2 diabetes can be dangerous and could cause cardiovascular disease as well. Your blood sugar level is greater than the average blood sugar level. There are different tests that we will go through to decide the nearness of high blood sugar levels. Blood glucose and A1c tests are two of them.
Definition of A1C and Glucose
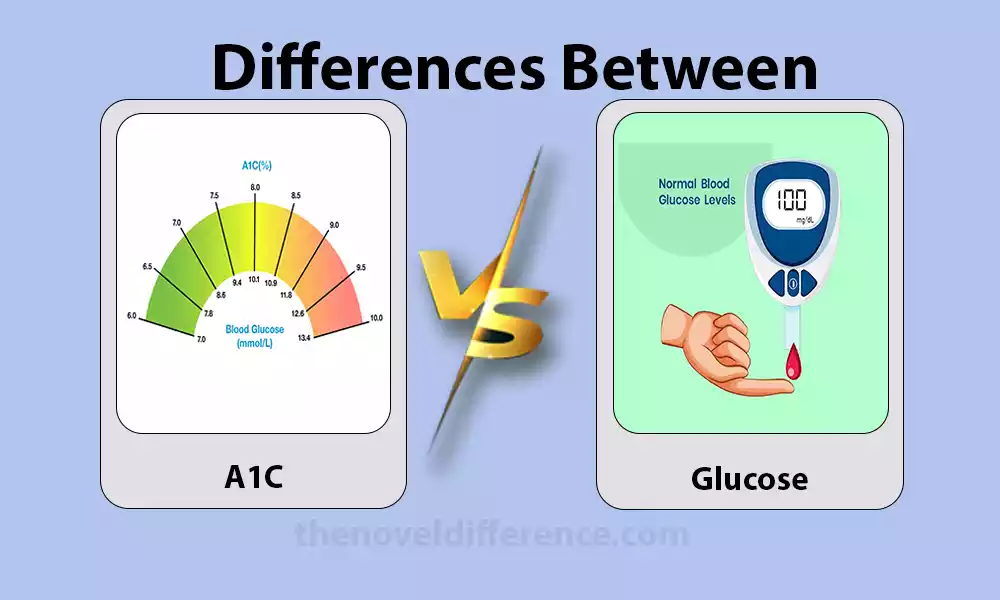
A1C: A1C, also known as glycated hemoglobin, may be a blood test that measures typical blood sugar levels over A1C and Glucose to three months. It indicates long-term blood sugar control. The A1C test measures the rate of hemoglobin (a protein in ruddy blood cells) that’s glycated, or bound to glucose. Since red blood cells have a lifespan of approximately three months, the A1C test reflects the average blood sugar levels during that time. The results are reported as a percentage, with higher values indicating poorer blood sugar control.
Glucose: Glucose, also alluded to as blood sugar, is the essential source of vitality for the body’s cells. It could be a straightforward sugar that circulates within the circulation system and is obtained from the breakdown of carbohydrates within the eat less. Glucose levels within the blood can vary all through the day in reaction to different variables, such as nourishment admissions, physical movement, and hormone levels.
Observing blood glucose levels is critical for people with diabetes to guarantee the appropriate administration of their condition. Glucose levels are commonly measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L), and the timing of the estimation (fasting, postprandial, subjective) may impact the explanation of the around.
Importance of monitoring blood sugar levels
Monitoring blood sugar levels is crucial for several reasons:
1. Diabetes management: For individuals with diabetes, monitoring blood sugar levels helps in managing the condition effectively. It permits them to get how their body reacts to nourishment, physical movement, pharmaceuticals, and other components. By observing blood sugar levels, people can make educated choices almost their eat less, working out, and medicine to keep their blood sugar inside the target extent.
2. Treatment adjustments: Regular monitoring of blood sugar levels provides valuable information to healthcare professionals for making necessary adjustments to diabetes treatment plans. It helps them assess the effectiveness of medications, insulin dosages, and lifestyle interventions. By analyzing blood sugar trends, healthcare providers can tailor treatment plans to meet the specific needs of individuals with diabetes.
3. Hypoglycemia and hyperglycemia prevention: Checking blood sugar levels permits people to distinguish and avoid scenes of hypoglycemia (moo blood sugar) and hyperglycemia (tall blood sugar). By distinguishing blood sugar variances early on, people can take provoked activity to anticipate complications related to extraordinary blood sugar levels, such as seizures, misfortune of awareness, diabetic ketoacidosis, or long-term harm to organs.
4. Long-term complications prevention: Monitoring blood sugar levels is integral in protecting against long-term effects associated with diabetes. Tall blood sugar levels over a drawn-out period can lead to complications influencing the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), nerves (diabetic neuropathy), and cardiovascular framework (heart illness, stroke). By maintaining optimal blood sugar control, individuals can reduce the risk of these complications and maintain better overall health.
5. Lifestyle evaluation: Observing blood sugar levels gives experiences into the impacts of counting calories, physical action, stretch, and other way-of-life variables on blood sugar direction. It helps individuals identify patterns or triggers that may contribute to blood sugar fluctuations, empowering them to make informed choices about their lifestyle habits and make adjustments as necessary.
Observing blood sugar levels enables people with diabetes to require control of their condition, anticipate complications, and make educated choices concerning their treatment and way of life choices. It is a fundamental component of successful diabetes administration and advances in general well-being.
What is A1C?
A1C, moreover known as glycated hemoglobin, could be a blood test that gives a normal degree of blood sugar levels over the past A1C and Glucose to three months. It specifically reflects the amount of glucose that has become attached to hemoglobin, the protein within red blood cells. A1C is expressed as a percentage and is commonly used to diagnose and monitor diabetes.
What is an A1c Test?
Hemoglobin A1c tests provide insight into your average level of blood sugar over the past 2 or 3 months. It’s moreover called HbA1c, glycated hemoglobin test, and glycohemoglobin. It’s a parcel like a baseball player’s season batting normally. A single diversion doesn’t tell you how a player is performing in their career. And 1 day’s test comes about do not grant you the total picture of how your treatment is working.
Individuals who have diabetes require this test routinely to see if their levels are remaining inside the extent. It can tell in case you would like to alter your diabetes drugs. The A1c test is additionally utilized to analyze diabetes.
How is A1C measured?
The A1C test measures the rate of glycated hemoglobin (HbA1c) inside the blood, reflecting the ordinary blood sugar levels over A1C and Glucose to three months.
Here’s how the A1C is measured:
1. Blood sample collection: The A1C test requires a blood sample, which is typically obtained through a simple blood draw from a vein in the arm. An effective blood sample collection system should include A1C and Glucose needle and syringe or vacuum tube methods of taking samples.
2. Laboratory analysis: Once the blood sample is collected, it is sent to a laboratory for analysis. Samples undergo various chemical procedures to ascertain how much hemoglobin has become glycosylated.
3. Hemoglobin separation: The primary step within the research facility examination is to isolate the hemoglobin from other components of the blood test. Hemoglobin is the protein in ruddy blood cells that carries oxygen all through the body.
4. Glycation detection: After separating the hemoglobin, the laboratory technicians use various methods to detect and quantify the glycated portion of the hemoglobin. One common strategy is ion-exchange high-performance fluid chromatography (HPLC), which isolates distinctive shapes of hemoglobin based on their electrical charge. Another method is immunoassay, which utilizes antibodies to specifically detect glycated hemoglobin.
5. Calculation of A1C percentage: Once the sum of glycated hemoglobin is measured, it is communicated as a rate of the whole hemoglobin within the blood test. This percentage represents the A1C level.
6. Reporting the results: The laboratory provides the A1C results to the healthcare provider or individual undergoing the test. The results are reported as a percentage, indicating the average blood sugar levels over the preceding A1C and Glucose to three months. The higher the rate, the higher the normal blood sugar levels.
It’s imperative to note that the A1C test ought to be performed in a certified research facility utilizing standardized strategies to guarantee exact and ddependable rollults. Also, certain variables such as certain restorative conditions (e.g., iron deficiency, hemoglobinopathies) and pregnancy can influence the precision of A1C estimations, so it’s basic to examine any important components with a healthcare proficiency.
Interpreting A1C results
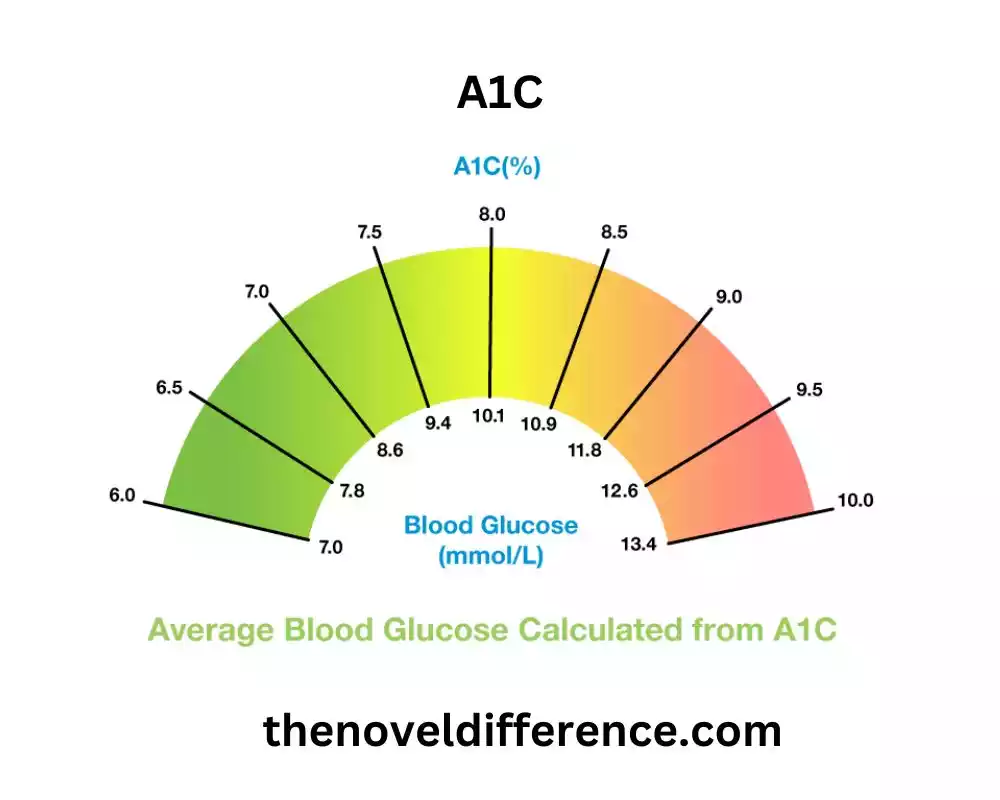
Interpreting A1C results involves understanding the percentage value obtained from the test and its relationship to average blood sugar levels over A1C and Glucose to three months.
Here’s how to interpret A1C results:
1. A1C levels and corresponding blood sugar averages: The A1C result is reported as a percentage. This percentage represents the average blood sugar levels over the preceding A1C and Glucose to three months. The following are general guidelines for interpreting A1C results:
• Normal range: A1C levels below 5.7% are typically considered within the normal range, indicating good blood sugar control.
• Prediabetes range: A1C levels between 5.7% and 6.4% demonstrate prediabetes, which suggests the person has higher-than-normal blood sugar levels but isn’t tall sufficient to be classified as diabetes.
• Diabetes range: A1C levels of 6.5% or higher are often indicative of diabetes. A conclusion of diabetes is more often than not affirmed with extra tests, such as fasting blood glucose or verbal glucose resistance tests.
2. Target A1C levels for different individuals: The target A1C levels may shift depending on components such as age, general well-being, and the nearness of other therapeutic conditions.
The American Diabetes Association (ADA) recommends the following target ranges:
• For most non-pregnant adults with diabetes: A1C below 7% is often the target, indicating good blood sugar control. Individualized targets should take into account factors like the duration of diabetes, age, and potential complications.
• For certain individuals: such as older adults or those with a history of severe hypoglycemia or limited life expectancy, more relaxed targets (e.g., A1C below 8%) may be appropriate.
• For pregnant individuals with diabetes: A1C levels below 6% are generally recommended to reduce the risk of pregnancy complications.
3. A1C as an indicator of diabetes management: Regular A1C testing is an essential tool in assessing the effectiveness of diabetes management. Monitoring A1C levels over time helps evaluate the impact of treatment plans, lifestyle changes, and medication adjustments on blood sugar control. By aiming for target A1C levels, individuals can reduce the risk of diabetes-related complications and maintain overall better health.
It’s imperative to note that A1C comes about and ought to be translated in conjunction with other blood sugar estimations, such as fasting blood glucose and self-monitoring of blood glucose. A healthcare professional can provide personalized guidance and help interpret A1C results in the context of an individual’s overall health and diabetes management plan.
Why is A1C important?
A1C is an essential tool for assessing overall diabetes management. By reflecting average blood sugar levels over a prolonged period, it offers insights into how well an individual’s treatment plan is working. A1C results guide healthcare providers in determining treatment adjustments, evaluating the risk of complications, and setting personalized targets for diabetes control.
What is glucose?
Glucose could be a straightforward sugar and an essential source of vitality for the body’s cells. It is determined from the nourishments we expend and is transported through the circulatory system to different organs and tissues. Keeping up ideal glucose levels is significant for generwellbeingng and well-being.

Energy and Storage
Your body is outlined to keep the level of glucose in your blood consistent. Beta cells in your pancreas screen your blood sugar level every few seconds. When your blood glucose rises after you eat, the beta cells discharge affront into your circulation system. Affront acts like a key, opening muscle, fat, and liver cells so glucose can get interior them.
Most of the cells in your body utilize glucose besides amino acids (the building blocks of protein) and fats for vitality. But it’s the most source of fuel for your brain. Nerve cells and chemical delivery people there require it to assist theprepardatata. If it wasn’t for this, the brain would not be functioning properly.
Once your body has utilized the energy it requires to function, any excess glucose is stored in tiny bundles of glycogen in the liver and muscles. Your body can store sufficient to fuel you for almost a day.
After you haven’t eaten for several hours, your blood glucose level drops. Your pancreas stops churning out affront. Alpha cells within the pancreas start to deliver a distinctive hormone called glucagon. It signalizes the liver to break down stored glycogen and transform it into glucose.
That voyages to your circulatory system to renew your supply until you’re able to eat once more. Your liver can moreover make its claim glucose employing a combination of squander items, amino acids, and fats.
How is glucose measured?
Glucose levels can be measured using various methods.
The most common methods of measuring glucose include:
1. Self-Monitoring of Blood Glucose (SMBG): This method involves using a glucose meter to measure glucose levels in a drop of blood obtained through a fingerstick. The process typically involves the following steps: a. Clean the fingertip with an alcohol swab. b. Use a lancet device to prick the fingertip and obtain a small drop of blood. c. Place the blood sample on a test strip that is inserted into the glucose meter. d. The glucose meter analyzes the blood sample and displays the glucose concentration on its screen.
2. Continuous Glucose Monitoring (CGM): CGM systems provide real-time glucose monitoring throughout the day and night. CGM systems use a small sensor inserted under the skin, usually on the abdomen or arm, to measure glucose levels in the interstitial fluid. The sensor sends the glucose readings wirelessly to a receiver or smartphone app, allowing users to monitor glucose levels continuously. Some CGM systems also provide alerts for high or low glucose levels.
3. Laboratory-Based Blood Glucose Tests: Blood glucose levels can be measured through venous blood samples collected by healthcare professionals. The blood samples are sent to a laboratory for analysis. Laboratory-based tests may include a. Fasting Blood Glucose Test: This test measures glucose levels after an overnight quick (as a rule 8 to 12 hours) to survey fasting blood sugar levels. b.
4. Oral Glucose Tolerance Test (OGTT): This test includes expending a particular sum of glucose arrangement, and blood tests are taken at interims (such as 1 hour, 2 hours) a short time later to the degree how the body forms glucose over time. OGTT is commonly used to diagnose gestational diabetes and impaired glucose tolerance. c. Random Blood Glucose Test: This test measures glucose levels at any time, regardless of when the person last ate. It is often used in emergency or clinical situations when immediate glucose assessment is required.
It’s important to follow the instructions provided with the glucose monitoring device or consult with a healthcare professional for accurate and proper usage of glucose monitoring methods. Standard observing of glucose levels is basic for people with diabetes to evaluate their blood sugar control, make fitting alterations to their treatment plans, and keep up ideal well-being.
Why is glucose important?
Glucose levels specifically impact a person’s prompt well-being and can have a noteworthy effect on long-term well-being. Tall blood sugar (hyperglycemia) can lead to indications like expanded thirst, visit urination, weakness, and obscured vision. Moo blood sugar (hypoglycemia) can cause tiptipinessisarray, shakiness, and indeed misfortune of awareness. Maintaining stable glucose levels is crucial for managing diabetes effectively.
Comparison Chart
Certainly! Here’s a comparison chart highlighting the key differences between A1C and glucose measurements:
| A1C | Glucose |
|---|---|
| Reflects 2-3 months average | Snapshot or short-term |
| Blood test | Self-monitoring, CGM, or lab test |
| Percentage (%) | mg/dL or mmol/L |
| Assess long-term blood sugar control, evaluate diabetes management | Real-time monitoring, immediate treatment decisions |
| Diagnose diabetes, assess treatment effectiveness, evaluate the risk of complications | Immediate treatment adjustments, managing blood sugar fluctuations |
It’s important to note that while A1C is a valuable tool for assessing long-term blood sugar control, glucose measurements play a crucial role in day-to-day diabetes management and treatment decisions. A1C and Glucose measurements provide valuable information in managing diabetes effectively.
Similarities Between A1C and Glucose
While A1C and glucose measurements differ in several aspects, there are also some similarities between A1C and Glucose.
Here are some commonalities:
1. Blood sugar indicators: Both A1C and glucose measurements provide information about blood sugar levels in the body.
2. Diabetes management: Both A1C and glucose measurements are used in the management of diabetes. They help healthcare providers and individuals with diabetes monitor blood sugar control, make treatment decisions, and assess the effectiveness of diabetes management strategies.
3. Relationship to diabetes complications: Both A1C and glucose levels are associated with the risk of developing diabetes-related complications, such as cardiovascular disease, kidney disease, nerve damage, and eye problems. Higher A1C levels and elevated glucose levels can increase the risk of complications in individuals with diabetes.
4. Targets for control: Both A1C and glucose measurements have target ranges that guide diabetes management. These targets are set based on rules built up by organizations such as the American Diabetes Affiliation (ADA). The objective is to preserve blood sugar levels inside a particular run to decrease the chance of complications and advance general well-being.
5. Monitoring tools: Both A1C and glucose measurements can be tracked over time to monitor changes in blood sugar control. Regular monitoring allows individuals and healthcare providers to assess trends, evaluate treatment effectiveness, and make adjustments to the management plan as needed.
While A1C provides a broader picture of long-term blood sugar control, glucose measurements offer more immediate information about blood sugar levels. A1C and Glucose measurements are valuable in understanding and managing diabetes, complementing each other to provide a comprehensive assessment of blood sugar control and guide treatment decisions.
Conclusion
Understanding the differences between A1C and glucose is crucial for effectively managing diabetes. A1C provides an average measure of blood sugar control over several months, while glucose measurements offer real-time feedback.
A1C and Glucose measurements have unique roles in assessing diabetes management and guiding treatment decisions. By working closely with healthcare providers, individuals with diabetes can strive for optimal A1C and glucose levels, promoting better long-term health outcomes.