When it comes to understanding the complex forms that happen within the human body, the renal framework plays a crucial part. The kidneys are capable of keeping up the body’s liquid adjust, sifting squander items, and controlling different electrolyte levels. Two critical processes that take put within the renal tubules are tubular reabsorption and tubular emission. We will delve into the difference between tubular reabsorption and tubular secretion, exploring their mechanisms and functions in detail.
Definition of Tubular Reabsorption and Tubular Secretion
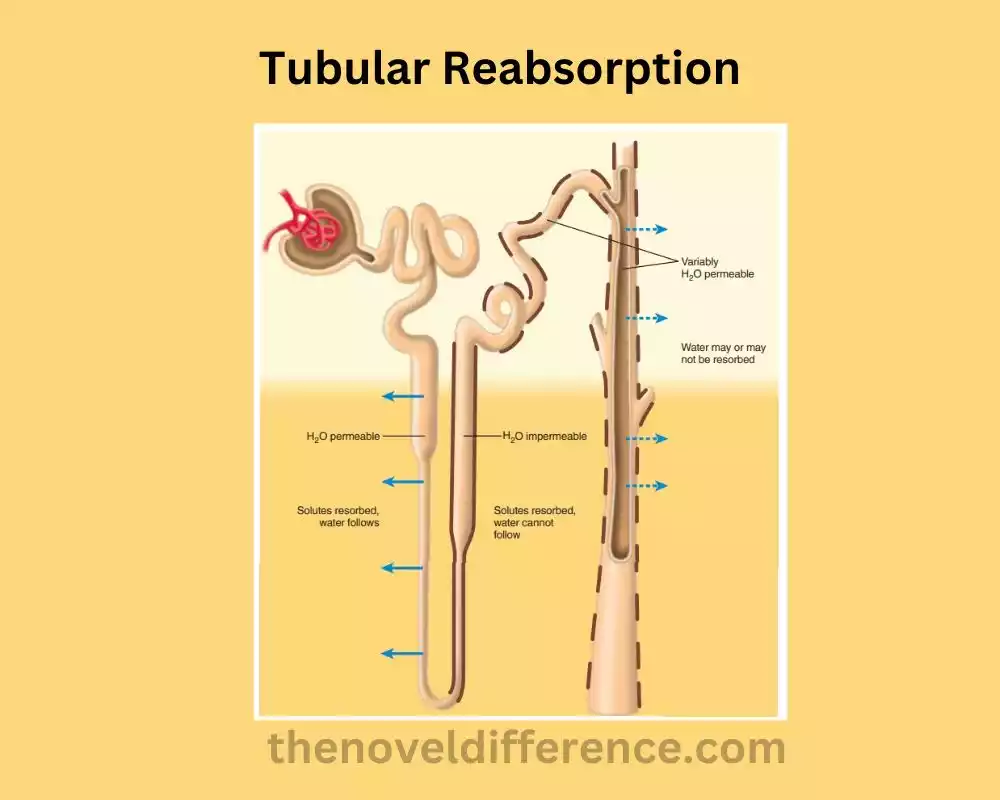
Tubular Reabsorption: Tubular reabsorption may be a preparation in renal physiology where substances that were initially sifted out of the blood within the glomerulus are transported back into the circulatory system through the renal tubules. It occurs primarily in the proximal convoluted tubule, but also in other segments of the nephron. Amid tubular reabsorption, fundamental substances such as water, electrolytes, glucose, and amino acids are reabsorbed to preserve the body’s liquid adjust and protect profitable supplements. The process involves both active and passive transport mechanisms, regulated by hormones and autoregulation.
Tubular Secretion: Tubular secretion is a process in renal physiology where substances are actively transported from the peritubular capillaries into the renal tubules for excretion into the urine. It happens transcendently within the proximal convoluted tubule and distal convoluted tubule, as well as within the collecting channels. Tubular secretion plays a vital role in eliminating waste products, regulating acid-base balance, and controlling the concentration of certain ions in the body. Hydrogen ions, potassium particles, creatinine, urea, and different drugs and poisons are illustrations of substances that are effectively emitted from the blood into the renal tubules. Hormonal control, autoregulation, and neural control contribute to the regulation of tubular secretion.
Importance of these processes in renal physiology
Tubular reabsorption and tubular secretion are essential processes in renal physiology that play crucial roles in maintaining overall bodily homeostasis.
Here are the key significance of these forms:
1. Maintenance of fluid and electrolyte balance: Tubular reabsorption guarantees that the correct sum of water and electrolytes, such as sodium, potassium, and chloride, are reabsorbed back into the circulation system. This makes a difference control the volume and composition of body liquids, keeping up appropriate hydration and electrolyte adjustments.
2. Acid-base balance regulation: Tubular secretion of hydrogen ions and reabsorption of bicarbonate ions play a vital role in maintaining the body’s acid-base balance. By regulating the pH of the urine, the kidneys help maintain the overall acid-base equilibrium in the body.
3. Control of blood pressure: Tubular reabsorption of sodium ions, coupled with water reabsorption, affects blood volume and subsequently blood pressure. By adjusting the reabsorption of sodium, the kidneys can influence blood pressure regulation.
4. Nutrient reabsorption: Tubular reabsorption ensures the reabsorption of essential nutrients, such as glucose and amino acids, which are selectively transported back into the bloodstream. This process prevents their loss in the urine and helps maintain proper nutrient levels in the body.
5. Waste product elimination: Tubular secretion facilitates the excretion of waste products, such as creatinine and urea, from the bloodstream into the urine. By actively secreting these substances, the kidneys aid in the elimination of metabolic waste and maintain overall physiological balance.
6. Drug and toxin elimination: Tubular secretion also plays a critical role in eliminating drugs, toxins, and foreign substances from the body. By actively secreting these substances into the tubules, the kidneys contribute to the detoxification and removal of potentially harmful compounds.
Tubular reabsorption and tubular discharge are basic forms that permit the kidneys to direct liquid and electrolyte adjustments, keep up acid-base harmony, dispense with squandered items, and control blood weight. These forms are crucial for keeping up by and large renal work and supporting the right working of the body as an entirety.
What is Tubular Reabsorption?
Tubular reabsorption could be a physiological handle that happens within the renal tubules of the kidneys. It involves the selective transport of substances from the tubular fluid back into the bloodstream, effectively reabsorbing them and preventing their loss in the urine.
Tubular reabsorption primarily takes place in the proximal convoluted tubule, but it also occurs in other segments of the nephron, including the loop of Henle, the distal convoluted tubule, and collecting ducts. This handle plays a significant part in keeping up the body’s liquid adjust, and electrolyte levels, and supplementing homeostasis.
Amid tubular reabsorption, different substances are transported over the tubular epithelium and into the peritubular capillaries. The reabsorption can happen through both dynamic and inactive transport instruments, depending on the characteristics of the substances being reabsorbed.
Some of the key substances that undergo tubular reabsorption include:
1. Water: The majority of water reabsorption occurs passively via osmosis. As solutes, such as sodium and glucose, are reabsorbed, water follows them through water channels called aquaporins.
2. Sodium ions: Sodium reabsorption is crucial for maintaining fluid balance and blood pressure regulation. It happens through dynamic transport forms, fundamentally within the proximal convoluted tubule, where sodium particles are transported out of the tubular lumen and into the peritubular capillaries.
3. Glucose: Glucose reabsorption occurs through active transport processes facilitated by glucose transporters. Under normal circumstances, all filtered glucose is reabsorbed in the proximal convoluted tubule, preventing its loss in the urine.
4. Amino acids: Like glucose, amino acids are actively reabsorbed in the proximal convoluted tubule to prevent their excretion.
5. Other electrolytes and nutrients: Various ions, such as potassium, calcium, phosphate, and bicarbonate, are also reabsorbed in specific segments of the renal tubules to maintain appropriate levels in the body.
The method of tubular reabsorption is firmly directed by different variables, counting hormones such as antidiuretic hormone (ADH) and aldosterone, as well as autoregulation and neural control. These mechanisms ensure that the reabsorption of substances occurs optimally, maintaining the body’s internal balance and preventing excessive loss of essential solutes.
Active transport
Active transport could be a handle in which atoms or particles are transported over a cell layer against their concentration angle, from a range of lower concentration to a region of higher concentration. This process requires the use of vitality within the frame of adenosine triphosphate (ATP) or an electrochemical slope.
Specific transport proteins called carrier proteins or pumps are involved. These proteins span the cell membrane and undergo conformational changes to facilitate the movement of molecules or ions across the membrane. The conformational changes occur in response to the binding of the transported substance and the energy provided by ATP hydrolysis or an electrochemical gradient.
Active transport is essential for various physiological processes in the body, including:
1. Nutrient uptake: Active transport is involved in the absorption of nutrients in the gastrointestinal tract. For example, the absorption of glucose in the intestines relies on active transport proteins.
2. Ion homeostasis: Active transport plays a vital part in keeping up the adjustment of particles, such as sodium, potassium, calcium, and hydrogen particles, over cell layers. This is often vital for nerve conduction, muscle compression, and the general work of cells and tissues.
3. Kidney function: Active transport within the renal tubules permits for the reabsorption of basic substances, such as glucose, amino acids, and particles, from the filtrate back into the circulatory system, as well as the emission of squandered items into the pee.
4. Cellular signaling: Active transport is involved in the uptake and release of signaling molecules and neurotransmitters, allowing for proper communication between cells.
5. Drug absorption and excretion: Active transport processes in various tissues, including the intestines, kidneys, and liver, are responsible for the absorption and excretion of drugs and other xenobiotics.
Active transport is a vital mechanism for the transport of molecules and ions across cell membranes, against their concentration gradients. It permits cells and organs to preserve fitting levels of substances, direct cellular forms, and carry out specialized functions essential for the correct working of the body.
Passive transport
Passive transport is a biological process by which molecules or ions move across a cell membrane without the need for energy expenditure. Unlike active transport, passive transport relies on the inherent physical properties of molecules and the concentration gradients across the membrane.
There are three main types of passive transport:
1. Diffusion: Diffusion is the spontaneous movement of molecules or ions from an area of higher concentration to an area of lower concentration. This movement occurs down the concentration gradient until equilibrium is reached. Straightforward dissemination includes the coordinated development of little, nonpolar particles (e.g., oxygen and carbon dioxide) over the lipid bilayer of the cell film. Facilitated diffusion, on the other hand, involves the movement of larger or charged molecules through specific transport proteins, such as channel proteins or carrier proteins.
2. Osmosis: Osmosis is a specific type of diffusion that refers to the movement of water across a selectively permeable membrane. Water particles move from a region of lower solute concentration (hypotonic) to a region of higher solute concentration (hypertonic) until harmony is built up. Osmosis is significant for keeping up legitimate hydration and osmotic adjustments in cells and tissues.
3. Filtration: Filtration is the movement of solutes through a selectively permeable membrane under the influence of hydrostatic pressure. This process occurs in specialized structures such as the glomerulus in the kidneys, where blood pressure forces water and small solutes to pass through the filtration barrier and form the initial filtrate.
Passive transport is an important mechanism for various biological processes, including:
• Nutrient uptake: Small molecules, such as glucose and amino acids, can enter cells through facilitated diffusion or simple diffusion.
• Gas exchange: Oxygen and carbon dioxide diffuse across cell membranes to facilitate gas exchange in tissues and lungs.
• Maintenance of ion balance: Some ions, such as potassium and chloride, can passively diffuse across membranes to maintain proper ion concentrations.
• Cell signaling: Small molecules and ions involved in cellular signaling can move across membranes passively, allowing for communication between cells.
Passive transport is a fundamental process that allows for the movement of molecules and ions across cell membranes, driven by the concentration gradients. It plays a pivotal part in keeping up cellular homeostasis and encouraging basic physiological capacities.
What is Tubular Secretion?
Tubular secretion is a process in renal physiology where substances are actively transported from the peritubular capillaries into the renal tubules for excretion into the urine. It happens essentially within the proximal convoluted tubule and distal convoluted tubule, as well as within the collecting channels of the nephron.
Tubular emission plays an imperative part in a few physiological capacities, including:
1. Elimination of waste products: Tubular discharge encourages the evacuation of certain squandered items from the circulation system into the tubular liquid, which is able in the long run be excreted within the pee. Examples of waste products that undergo tubular secretion include creatinine, a metabolic waste product from muscle breakdown, and urea, a byproduct of protein metabolism.
2. Acid-base balance regulation: The secretion of hydrogen ions (H+) into the renal tubules helps regulate the pH balance of the body. By actively secreting hydrogen ions, the kidneys contribute to the elimination of excess acid and the maintenance of proper acid-base equilibrium.
3. Ion homeostasis: Tubular secretion also allows for the regulation of the concentration of certain ions in the body. The distal convoluted tubule secretes hydrogen particles (H+) and potassium particles (K+) into the tubular liquid while reabsorbing sodium particles (Na+). This process helps maintain proper electrolyte balance.
4. Drug and toxin elimination: Tubular secretion is involved in the excretion of various drugs, toxins, and foreign substances from the body. It serves as a critical component for expelling these substances from the circulation system and anticipating their aggregation within the body.
The process of tubular secretion is mediated by specific transport proteins located on the apical (luminal) membrane of the renal tubular cells. These transporters actively move substances from the peritubular capillaries into the tubular fluid, against their concentration gradients. Examples of substances that undergo tubular secretion include hydrogen ions, potassium ions, organic acids, organic bases, and certain drugs.
The regulation of tubular secretion is influenced by various factors, including hormonal control, autoregulation, and neural control. Hormones such as aldosterone and antidiuretic hormone (ADH) can balance the discharge of particular substances in reaction to the body’s needs and keep up homeostasis.
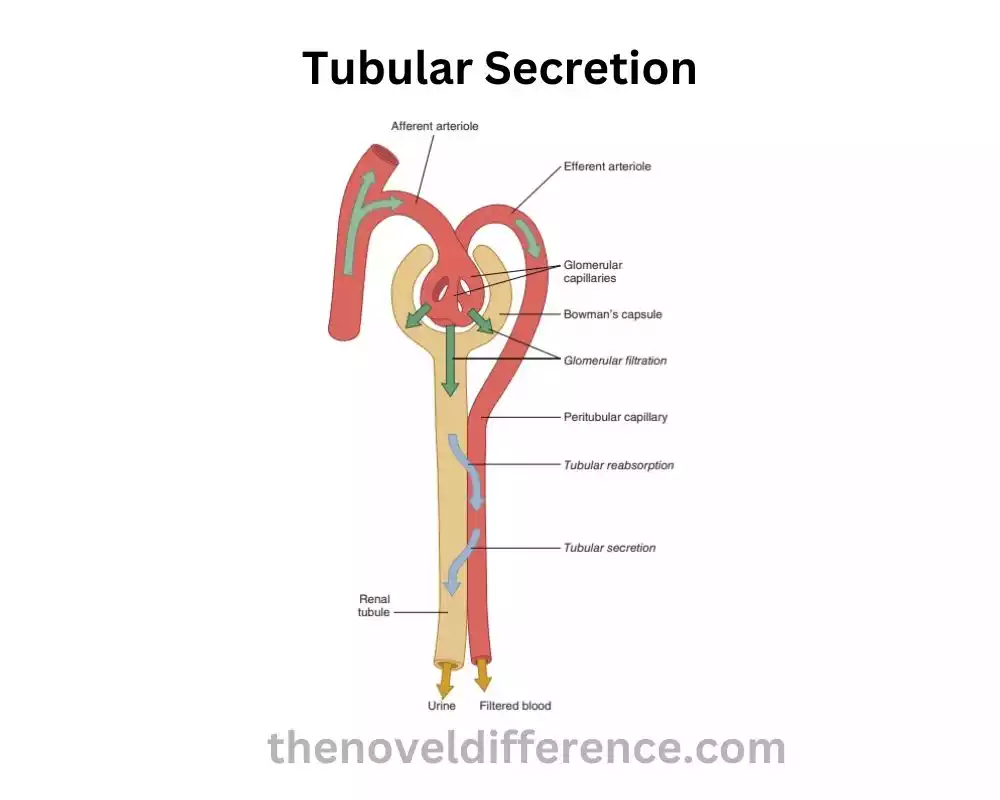
Tubular emission is a dynamic preparation within the kidneys that includes the specific transport of substances from the peritubular capillaries into the renal tubules. It plays a crucial role in waste product elimination, acid-base balance regulation, ion homeostasis, and the elimination of drugs and toxins from the body.
Hydrogen ions
Hydrogen ions (H+) are positively charged ions consisting of a single proton and no electrons. Hydrogen particles play a critical part in a few physiological forms and are especially vital in directing the pH adjustment of different body liquids.
Here are some key aspects related to hydrogen ions:
1. Acidic properties: Hydrogen ions are often associated with acidity. Hydrogen ions can separate from water atoms, coming about in an increment within the concentration of H+ particles and a diminish in pH. Substances that release hydrogen ions are called acids.
2. pH balance: pH is a measure of the acidity or alkalinity (basicity) of a solution. The pH scale ranges from 14, with 7 being considered unbiased, values below 7 demonstrating corrosiveness, and values over 7 showing alkalinity. The concentration of hydrogen ions in a solution determines its pH. The higher the concentration of H+ particles, the lower the pH and the more acidic the arrangement.
3. Acid-base regulation: Hydrogen ions play a crucial role in maintaining proper acid-base balance in the body. This balance, known as acid-base homeostasis, is essential for normal physiological functions. The kidneys, along with the respiratory system and various buffer systems, help regulate the concentration of hydrogen ions in the body to maintain pH within a narrow range. The secretion of hydrogen ions into the renal tubules during tubular secretion is one mechanism by which the kidneys contribute to acid-base regulation.
4. pH of body fluids: Different body fluids have different pH levels. Blood vessel blood pH is regularly around 7.4, which is marginally soluble. Venous blood and interstitial fluid have slightly lower pH values. The pH of gastric corrosive within the stomach is exceedingly acidic (around 1-3), whereas the pH of pee can shift depending on components such as hydration status and slimming down.
5. Electrolyte balance: Hydrogen ions are included within the control of electrolyte adjustment, especially the adjustment of sodium (Na+) and potassium (K+) particles. The kidney’s capacity to emit hydrogen particles into the renal tubules is coupled with the reabsorption of sodium particles, making a difference to preserve appropriate sodium-potassium adjustment.
6. Cellular function: Hydrogen ions play a part in cellular forms such as chemical action and the era of adenosine triphosphate (ATP) in mitochondria. Changes in hydrogen ion concentration can affect enzyme function and alter cellular metabolism.
Hydrogen ions are vital in keeping up the pH adjustment of body liquids, directing acid-base homeostasis, and impacting different physiological forms. Their concentration is tightly regulated by the kidneys, respiratory system, and buffer systems to ensure the proper functioning of the body.
Potassium ions
Potassium ions (K+) are emphatically charged particles that play a pivotal part in various physiological forms inside the human body. They are one of the foremost inexhaustible intracellular cations and are fundamental for legitimate cellular work.
Here are some key aspects related to potassium ions:
1. Electrolyte balance: Potassium may be a major intracellular electrolyte, and its concentration in interior cells is much higher than in extracellular liquids. Keeping up the adjustment of potassium particles between the intracellular and extracellular compartments is basic for typical cell work, counting nerve transmission, muscle compression, and the upkeep of appropriate liquid adjust.
2. Nerve and muscle function: Potassium ions are involved in the generation and propagation of nerve impulses (action potentials). They play a vital role in maintaining the resting membrane potential of neurons and muscle cells. Changes within the extracellular potassium concentration can influence the volatility of nerves and muscles, possibly driving anomalies such as muscle shortcomings, cardiac arrhythmias, and neurological unsettling influences.
3. Acid-base balance: Potassium ions are involved in acid-base regulation, particularly in the exchange with hydrogen ions (H+) in the kidneys. Hydrogen particles can be traded for potassium particles within the distal renal tubules, making a difference to control the pH adjustment of the blood and keeping up appropriate acid-base homeostasis.
4. Fluid and electrolyte balance: Potassium ions, along with sodium ions (Na+), help regulate fluid balance and osmotic pressure across cell membranes. The concentration of potassium particles within the extracellular liquid is directed by different instruments, counting renal excretion, reabsorption, and the action of potassium channels in cell films.
5. Heart function: Potassium ions are crucial for the normal functioning of the heart. They play a basic part in keeping up the electrical steadiness of cardiac cells and the consistency of cardiac muscle withdrawals. Imbalances in potassium levels can lead to arrhythmias and cardiac dysfunction.
6. Kidney function: The kidneys play a significant role in maintaining potassium balance in the body. They regulate potassium excretion through processes such as filtration, reabsorption, and secretion in the renal tubules. Hormones such as aldosterone and insulin also influence potassium handling in the kidneys.
It is critical to note that both moo potassium levels (hypokalemia) and tall potassium levels (hyperkalemia) can have unfavorable impacts on different physiological forms. Hypokalemia can lead to muscle shortcomings, cardiac arrhythmias, and metabolic unsettling influences, whereas hyperkalemia can result in serious cardiac arrhythmias and unsettling influences in nerve and muscle work.
Potassium ions are vital for maintaining proper cellular function, nerve transmission, muscle contraction, and fluid balance. Their levels are tightly regulated to ensure the normal functioning of the body.
Comparison Chart
Certainly! Here’s a comparison chart highlighting the key differences between tubular reabsorption and tubular secretion:
| Tubular Reabsorption | Tubular Secretion |
|---|---|
| Process of selectively transporting substances from renal tubules back into the bloodstream | Process of actively transporting substances from the peritubular capillaries into the renal tubules for excretion |
| Primarily occurs in the proximal convoluted tubule, but also in other segments of the nephron | Primarily occurs in the proximal convoluted tubule and distal convoluted tubule, as well as in the collecting ducts |
| Involves both active and passive transport mechanisms | Involves active transport of substances across the tubular epithelium |
| Reclaims important substances from the tubular fluid to prevent their loss in the urine | Eliminates substances from the blood and selectively removes them from the body |
| Moves substances from the tubular lumen into the peritubular capillaries (bloodstream) | Moves substances from the peritubular capillaries into the tubular lumen |
| Water, glucose, amino acids, electrolytes | Hydrogen ions, potassium ions, drugs, toxins, waste products |
| Maintains fluid balance, electrolyte homeostasis, and nutrient retention | Contributes to waste product elimination, acid-base balance regulation, drug and toxin elimination |
| Assessing renal function, managing electrolyte and acid-base disorders, understanding drug interactions | Assessing renal function, understanding drug interactions, managing kidney diseases and dysfunction |
Clinical Significance
The clinical significance of tubular reabsorption and tubular secretion lies in their role in renal physiology and their impact on various medical conditions and therapeutic interventions.
Here are some clinical implications of these processes:
1. Renal function assessment: Tubular reabsorption and secretion play a crucial role in the overall functioning of the kidneys. Evaluating the efficiency of these processes can help assess renal function and diagnose renal disorders. Tests such as renal clearance ponders, which degree of the rate at which certain substances are cleared from the blood by the kidneys, give important data approximately tubular reabsorption and emission.
2. Electrolyte and acid-base disorders: Disorders of tubular reabsorption and secretion can lead to imbalances in electrolytes and disruptions in acid-base balance. Abandons in tubular reabsorption of sodium or potassium can cause electrolyte unsettling influences such as hyperkalemia or hyponatremia. Similarly, impaired tubular secretion of hydrogen ions can result in metabolic acidosis.
3. Diuretics: Diuretic medications are commonly used to increase urine output and treat conditions such as hypertension and edema. They work by altering the processes of tubular reabsorption and secretion. For instance, loop diuretics inhibit sodium and chloride reabsorption in the loop of Henle, while thiazide diuretics inhibit sodium reabsorption in the distal convoluted tubule. Understanding these mechanisms is important for the appropriate use of diuretics and managing fluid and electrolyte balance.
4. Drug interactions and toxicity: Tubular secretion is involved in the excretion of drugs and toxins from the body. Alterations in tubular secretion can impact drug levels, efficacy, and toxicity. Certain drugs can inhibit or compete for transporters involved in tubular secretion, leading to drug interactions or increased risk of drug accumulation and toxicity. Knowledge of these processes helps in understanding drug pharmacokinetics and optimizing drug therapy.
5. Kidney diseases and dysfunction: Various kidney diseases can affect tubular reabsorption and secretion, leading to impaired renal function and associated clinical manifestations. For example, in renal tubular acidosis, there is a defect in hydrogen ion secretion, resulting in metabolic acidosis. Tubular brokenness may contribute to the advancement of proteinuria and electrolyte awkward nature.
6. Renal drug handling: Tubular reabsorption and secretion influence the renal clearance of drugs, which is an important consideration in drug dosing and therapeutic monitoring. Drugs that undergo extensive tubular reabsorption may require higher doses, while drugs that are actively secreted may be affected by drug-drug interactions or renal impairment.
Understanding the role of tubular reabsorption and secretion in renal physiology and their clinical implications helps healthcare professionals in diagnosing and managing renal disorders, optimizing drug therapy, and maintaining electrolyte and acid-base balance.
Conclusion
Tubular reabsorption and tubular secretion are essential processes in renal physiology that occur in the nephrons of the kidneys. Tubular reabsorption includes the specific transport of substances from the renal tubules back into the circulation system, basically within the proximal convoluted tubule, to recover vital substances such as water, glucose, amino acids, and electrolytes.
Tubular emission is the dynamic transport of substances from the peritubular capillaries into the renal tubules, especially within the proximal and distal convoluted tubules, for disposal from the body. Tubular secretion helps in the excretion of waste products, regulation of acid-base balance, and elimination of drugs, toxins, and excess ions.
