Axonal and demyelinating neuropathy are distinct forms of peripheral neuropathy, each with unique characteristics and implications. In axonal neuropathy, nerve damage primarily affects the nerve fibers (axons), while in demyelinating neuropathy, it involves the protective myelin sheath around the nerves. This brief overview will highlight the key disparities between these neuropathic conditions.
What is Axonal Neuropathy?
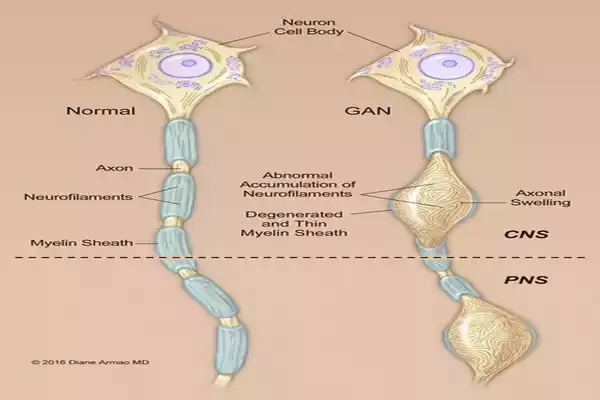
Axonal neuropathy, also known as axonopathy, is a type of peripheral neuropathy characterized by damage to the nerve fibers themselves, specifically the axons. Axons are the long, slender projections of nerve cells (neurons) that transmit electrical impulses, allowing for the communication of sensory information and motor signals between the body and the brain.
In axonal neuropathy:
- Nerve Fiber Damage: The primary feature is damage or degeneration of the axons, which disrupts the transmission of nerve signals.
- Mechanisms: Axonal neuropathy can result from various causes, including metabolic disorders, toxins, physical trauma, hereditary factors, or systemic diseases. These factors can directly damage the axons or disrupt the transport of essential nutrients and molecules along them.
- Clinical Presentation: Symptoms typically include muscle weakness, loss of sensation, tingling, and pain in the affected areas. The severity and specific symptoms can vary depending on the nerves involved.
- Diagnosis: Diagnosis often involves clinical evaluation, nerve conduction studies, electromyography (EMG), and sometimes nerve biopsies to assess the extent of axonal damage.
- Treatment: The management of axonal neuropathy aims to address underlying causes when possible and alleviate symptoms. This may involve medications for pain management, physical therapy, lifestyle modifications, and treatment of any underlying conditions contributing to the neuropathy.
Axonal neuropathy can be further categorized into acquired (resulting from external factors) and inherited (due to genetic mutations) forms, each with its own set of causes and treatment considerations. Accurate diagnosis and timely intervention are essential in managing axonal neuropathy and improving the quality of life for affected individuals.
What is Demyelinating Neuropathy?
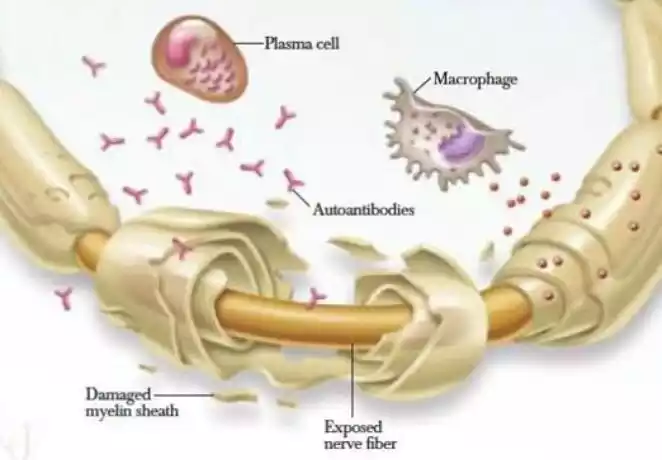
Demyelinating neuropathy, also known as demyelinating polyneuropathy, is a type of peripheral neuropathy characterized by damage to the protective myelin sheath that covers nerve fibers. The myelin sheath acts like insulation on an electrical wire, facilitating the rapid and efficient transmission of nerve signals.
Here are the key features of demyelinating neuropathy:
- Myelin Damage: In demyelinating neuropathy, the myelin sheath is damaged or destroyed, leading to impaired nerve signal conduction. This can cause various neurological symptoms.
- Mechanisms: Demyelinating neuropathies can occur due to various factors, including autoimmune disorders (like Guillain-Barré syndrome), hereditary conditions (such as Charcot-Marie-Tooth disease), infections (like certain viral or bacterial infections), and sometimes as a side effect of certain medications or as a result of exposure to toxins.
- Clinical Presentation: Symptoms of demyelinating neuropathy can include muscle weakness, loss of coordination, tingling, numbness, and difficulty with fine motor skills. The specific symptoms and their severity can vary based on the location and extent of myelin damage.
- Diagnosis: Diagnosis typically involves a combination of clinical evaluation, nerve conduction studies, electromyography (EMG), and sometimes cerebrospinal fluid analysis or nerve biopsies to determine the extent of myelin damage and rule out underlying causes.
- Treatment: Management of demyelinating neuropathy often focuses on addressing the underlying cause if known. In autoimmune demyelinating neuropathies like Guillain-Barré syndrome, immune-modulating therapies may be employed. Supportive care, physical rehabilitation, and medications for pain management can also be part of the treatment plan.
It’s important to note that demyelinating neuropathies can vary in their course and severity. Some may be acute and rapidly progressive, while others may have a more chronic and slowly progressing nature. Early diagnosis and appropriate treatment are vital for minimizing disability and improving outcomes for individuals with demyelinating neuropathy.
Axonal and Demyelinating Neuropathy in the comparison chart
Here’s a comparison chart highlighting the key differences between axonal and demyelinating neuropathy:
| Feature | Axonal Neuropathy | Demyelinating Neuropathy |
|---|---|---|
| Primary Damage | Axons are damaged | The Myelin sheath is damaged |
| Underlying Mechanisms | Toxins, trauma, diseases | Autoimmune, hereditary, infections |
| Symptoms | Muscle weakness, tingling, pain | Coordination issues, numbness, tingling |
| Clinical Presentation | Gradual, progressive loss of function | Fluctuating symptoms, relapsing-remitting pattern |
| Causes | Varied, including toxins, diseases, genetics | Often associated with autoimmune disorders, hereditary conditions |
| Diagnosis | Nerve conduction studies, electromyography | Cerebrospinal fluid analysis, nerve biopsies, nerve conduction studies |
| Treatment | Address underlying causes, pain management, physical therapy | Address underlying causes, immune modulation, supportive care |
| Prognosis | Varies depending on the cause, may be irreversible | Can fluctuate with periods of improvement and relapse |
Understanding these differences is crucial for healthcare professionals to make accurate diagnoses and implement appropriate treatment strategies for individuals with neuropathy.
Importance of distinguishing between axonal and demyelinating neuropathy
Distinguishing between axonal and demyelinating neuropathy is of paramount importance in clinical medicine for several reasons:
- Accurate Diagnosis: Determining the specific type of neuropathy allows for a precise diagnosis. This accuracy is crucial because the underlying causes, clinical courses, and treatment approaches often differ significantly between axonal and demyelinating neuropathies.
- Treatment Selection: The choice of treatment can be vastly different for axonal and demyelinating neuropathies. For example, immunomodulatory therapies that target the immune system might be effective in demyelinating neuropathies but ineffective or even harmful in axonal neuropathies.
- Prognostic Information: Knowing whether a neuropathy is axonal or demyelinating can provide valuable prognostic information. Demyelinating neuropathies often have a more favorable prognosis, with potential for recovery, especially when identified and treated early.
- Prevention of Complications: Understanding the specific type of neuropathy can help anticipate and address potential complications. For instance, if muscle weakness is due to axonal damage, strategies for managing muscle atrophy and preventing falls might be emphasized.
- Targeted Management: Rehabilitation and physical therapy plans can be tailored to address the unique deficits associated with each type of neuropathy. Demyelinating neuropathy patients may benefit from gait training, while axonal neuropathy patients may require strength-building exercises.
- Research and Drug Development: Accurate classification is vital in clinical trials and research. It ensures that study populations are appropriately defined, which is crucial for evaluating the effectiveness of new treatments.
- Cost-Efficiency: Appropriate differentiation between axonal and demyelinating neuropathies can reduce healthcare costs. Unnecessary and potentially harmful treatments can be avoided when the diagnosis is accurate.
- Patient Counseling: Patients and their families benefit from knowing the type of neuropathy. Understanding the nature of the condition, its potential progression, and treatment options can empower individuals to make informed decisions about their care and lifestyle.
Distinguishing between axonal and demyelinating neuropathy is not only diagnostically crucial but also has significant implications for treatment, prognosis, patient management, and the development of targeted therapies. This differentiation allows healthcare providers to provide the most effective and personalized care to individuals living with neuropathic conditions.
Diagnosing Axonal vs. Demyelinating Neuropathy
Diagnosing Axonal Neuropathy:
- Clinical Evaluation: Begins with a detailed medical history and physical examination, focusing on symptom presentation and progression.
- Nerve Conduction Studies (NCS): Measures nerve signal conduction speed and amplitude, revealing reduced signal strength or slower conduction.
- Electromyography (EMG): Evaluates muscle electrical activity, identifying denervation in affected muscles.
- Blood Tests: Used to detect underlying conditions like diabetes or vitamin deficiencies contributing to axonal neuropathy.
- Nerve Biopsy: Occasionally performed to assess the extent of nerve damage when the cause is unclear.
Diagnosing Demyelinating Neuropathy:
- Clinical Evaluation: Begins with a thorough history and physical examination, emphasizing symptom progression.
- Nerve Conduction Studies (NCS): Used to assess demyelinating neuropathy, showing slowed nerve conduction velocities and abnormal nerve signal shapes.
- Electromyography (EMG): Detects muscle activity abnormalities due to demyelination.
- Cerebrospinal Fluid Analysis: May reveal elevated protein levels in conditions like Guillain-Barré syndrome.
- Nerve Biopsy: Reserved for rare cases to confirm demyelinating neuropathy and distinguish it from other nerve disorders.
Future Directions in Neuropathy Research
Future directions in neuropathy research are promising, as ongoing studies and innovations aim to advance our understanding of these complex nerve disorders and improve treatment options.
Here are some key areas of focus:
- Genomic Research: Continued exploration of genetic factors contributing to neuropathies can lead to improved diagnostics and personalized treatment approaches. Identifying specific gene mutations associated with different neuropathies is crucial.
- Advanced Imaging Techniques: Advancements in imaging technologies, such as magnetic resonance neurography and high-resolution ultrasound, allow for better visualization of nerve structures, aiding in early diagnosis and monitoring disease progression.
- Nerve Regeneration: Research into regenerative therapies, including stem cell-based approaches and nerve grafting, holds promise for repairing damaged nerves and restoring function in neuropathy patients.
- Neuroinflammation: Understanding the role of neuroinflammation in neuropathies, especially autoimmune forms, can lead to the development of targeted immunomodulatory treatments with fewer side effects.
- Biomarkers: The discovery of reliable biomarkers can enable early diagnosis and tracking of disease progression, potentially improving treatment outcomes and therapeutic monitoring.
- Peripheral Nerve Interfaces: Innovations in neural interfaces and prosthetics can enhance the quality of life for individuals with neuropathy by restoring sensory and motor functions.
- Patient-Centered Research: More emphasis on patient-reported outcomes and patient engagement in research can lead to treatments that better address the unique needs and experiences of neuropathy patients.
- Big Data and AI: The analysis of large datasets using artificial intelligence can provide insights into neuropathy patterns, risk factors, and treatment responses, enabling more precise healthcare delivery.
- Drug Development: Ongoing efforts to identify and test novel drugs and therapies, including neuroprotective agents and gene therapies, offer hope for more effective treatments.
- Prevention Strategies: Research into lifestyle factors and environmental exposures that contribute to neuropathies, such as diet, exercise, and toxin exposure, can lead to preventative measures.
- Global Collaboration: International collaboration among researchers and healthcare providers can accelerate progress in neuropathy research by sharing knowledge and resources.
These future directions in neuropathy research aim to advance our understanding of the underlying mechanisms, improve diagnostic accuracy, enhance treatment options, and ultimately provide better outcomes and quality of life for individuals affected by neuropathic conditions.
Conclusion
Neuropathy encompasses a wide range of conditions affecting the peripheral nervous system. Understanding the distinctions between axonal and demyelinating neuropathy is crucial for accurate diagnosis and tailored treatment.
Both types present unique challenges, but ongoing research offers hope for improved diagnostics and therapies. As we delve deeper into the complexities of neuropathy, we move closer to providing better care and quality of life for those affected by these conditions.
