Definition of blood transfusion
The term “blood transfusion” refers to the process of receiving blood transfusion is a medical procedure where patients receive blood or other transfusions of blood intravenously. This could be the whole blood, or specific components of it, like platelets, red blood cells plasma, blood, or factors that clot.
Blood transfusions are often used to replace blood loss due to injury or surgery as well as to treat anemia if the body isn’t producing sufficient red blood cells or to treat illnesses that alter the blood’s functions or components. The proper matching and screening of blood donated for infectious agents is essential to guarantee the safety of the procedure.
Definition of dialysis
Dialysis is a medical procedure that mimics the functions of natural kidneys through the removal of excessive fluids, waste products, and electrolytes from the bloodstream.
This procedure becomes necessary when kidneys have been damaged or are unable to properly filter blood, which is seen in chronic kidney illness or acute kidney injury.
There are two primary dialysis types hemodialysis, which involves the removal of blood from the body, cleaned using an external device, and afterward back into the body, and dialysis peritoneal in which the cleanser enters the abdominal cavity.
The waste products are removed through the peritoneum, which is a membrane that lines an abdominal cavity. The choice of which method to use is determined by the patient’s medical conditions, lifestyle, and personal preference.

Blood Transfusion and Dialysis in the comparison chart
Here’s a comparison chart for Blood Transfusion and Dialysis:
| Feature | Blood Transfusion | Dialysis |
| Primary Purpose | Replace lost or deficient blood components | Replace kidney function to filter and clean blood |
| Indications | Blood loss, anemia, clotting disorders, certain cancers | Chronic kidney disease, acute kidney injury, fluid overload, certain poisonings |
| Procedure Duration | 1.5 to 4 hours (per unit) | Hemodialysis: 3-5 hours/session; Peritoneal Dialysis: Varies |
| Frequency | As needed based on the condition | Hemodialysis: Typically 3 times/week; Peritoneal Dialysis: Daily |
| Benefits | Restores blood volume, enhances oxygenation, supports clotting | Removes toxins, manages fluid, maintains electrolyte balance |
| Risks | Transfusion reactions, infections, iron overload | Infections, low blood pressure, muscle cramps, peritonitis |
| Associated Costs | Blood products, testing, hospitalization, administration | Treatment sessions, access maintenance, equipment, medications, monitoring |
| Equipment/Supplies | Blood bags, IV lines, transfusion sets | Dialysis machines, dialyzers, solutions, catheters, needles |
| Duration of Dependency | Typically short-term; some conditions require regular transfusions | Chronic, unless the patient undergoes a kidney transplant |
This chart offers a concise comparison of the two procedures. However, it’s essential to remember that the specifics for each patient might vary based on their medical conditions and circumstances.
Purpose and Indications of Blood Transfusion and Dialysis
Blood Transfusion
Purpose:
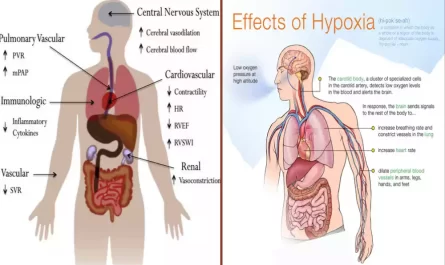
- To replace deficient or lost blood components for those who need them thus improving the ability of blood to provide oxygen to tissues of the body, to maintain hemostasis, and aid in other biological processes.
Indications:
- Blood loss: Due to surgeries traumas, or injuries that cause significant bleeding.
- Anemia: Anemia occurs when the body does not produce sufficient red blood cells. It could be caused by conditions such as iron deficiency anemia sickle cell anemia Thalassemia, and many more.
- Treatments for Cancer: Chemotherapy can affect the bone marrow, decreasing its capacity to make red blood cells.
- Bone Marrow Failure: Conditions like aplastic anemia, where the bone marrow is unable to make enough blood cells.
- coagulation disorders: When there’s a deficit in the clotting factors such as in hemophilia and von Willebrand’s.
- Thrombocytopenia: The low number of platelets can cause excessive bleeding.
- Organ Transplants: For the support of patients who undergo transplants, particularly if there is a possibility of blood loss, as well as if the person suffers from an existing illness that makes transplantation likely.
Dialysis
Purpose:
- To artificially fulfill the function of filtering the kidneys, they remove waste, salt, and fluids from our bodies. keep a steady concentration of certain chemical substances in the blood, and help in controlling blood pressure.
Indications:
- Chronic Kidney Disease (CKD) (also known as End-Stage Retinal Disease (ESRD): In cases where the kidneys have lost most of their filtering capabilities dialysis becomes a necessity to maintain life.
- Acute Kidney Injuries (AKI): Sudden and unexpected kidney failure, which can be reversed. Dialysis is a lifeline for the body during this time.
- Toxic Overload: In the case of poisonings or overdoses of drugs dialysis is a method to swiftly eliminate the causing agents.
- Electrolyte Imbalance: Conditions causing severe electrolyte imbalances, such as hyperkalemia (high potassium levels) which could be life-threatening.
- fluid overload: If diuretic treatment isn’t working or feasible dialysis may be able to remove excess fluid, aiding those suffering from heart failure.
It’s important to note that although dialysis and blood transfusions are vital treatments, they’re utilized for different scenarios in the clinical world. The necessity for either is determined by specific medical conditions and the judgment of medical experts.
Procedures of Blood Transfusion and Dialysis
Blood Transfusion
- Preparation:
- Crossmatching and Blood Typing: Before transfusion, both the donor’s and recipient’s blood is tested and cross-matched to guarantee compatibility, and lower the risk of having a transfusion reaction.
- screening: Donated blood is tested for infectious agents such as HIV Hepatitis B and C Syphilis, HIV, and a variety of other illnesses.
- Administration:
- Intravenous Access: An IV line is connected by a needle. an IV line (IV line) is placed into one of the veins of the patient.
- The Slower Introduction: The blood or its product is slowly introduced into the bloodstream of a patient.
- Monitoring: All through the blood transfusion the patient’s vital indicators (heart rate and temperature, blood pressure, etc.).) are continuously monitored to identify any negative reactions.
- Completion and Post-Transfusion:
- After the transfusion has been completed the IV line is taken out.
- The patient may be monitored for a brief time to check for any delayed reaction.
Dialysis
There are two major kinds of dialysis available: Hemodialysis as well as Peritoneal dialysis. Here’s a short overview of their methods:
- Hemodialysis:
- Vascular Access creation: Before the first session the surgical procedure is carried out to make a vascular access, the arteriovenous (AV) fistula, graft, or venous catheter.
- Connectivity to Dialysis Machine: During every session, two needles are inserted into the vascular access, and are linked to tubes that connect directly to dialysis machines.
- Cleansing the blood: The blood is expelled, and then passed through a dialyzer (or artificial kidney) inside the machine. There, the waste products, salt, and fluids are eliminated and transferred back to your body.
- Time of session: The typical session runs for 3-5 hours, and is typically required at least three times per week.
- Peritoneal Dialysis:
- Catheter placement: A soft tube (catheter) is surgically placed inside the abdomen, a few weeks before the first procedure.
- Fluid Description: Dialysis solution is introduced into the abdomen via the catheter. The peritoneal membrane in the body functions as a filter that allows waste products and excess fluid to move through the bloodstream into the solution.
- The process of draining: After several hours the solution that contains the body’s wastes is removed.
- Exchange: The dialysis fluid is then added to the system to begin over again. This process (fill in, dwell in, and drain) may be repeated multiple times per day, based upon the method used for dialysis selected.
Both dialysis and blood transfusion are complicated procedures that require meticulous attention as well as sterile methods and constant monitoring to ensure the safety of patients and the best results.
Benefits and Risks of Blood Transfusion and Dialysis
Blood Transfusion
Benefits:
- Live-saving: Restores blood flow after traumas, surgeries, or serious injuries.
- Oxygen Supply: Increases the capacity of oxygen transport of blood, which is particularly beneficial for those suffering from anemia.
- Allows blood Clotting: Provides platelets or clotting factors to patients suffering from bleeding disorders.
- Therapeutic Application: Helps manage and treat illnesses such as sickle cell disorder, thalassemia, and certain types of cancer.
Risks:
- The Transfusion Reactions: Allergies, febrile or more serious issues such as transfusion-related acute damage to the lung (TRALI).
- Diseases: While rare, due to a rigorous test, there is a chance of transmission of infections like HIV, hepatitis B, or C.
- Iron Overload: Multiple transfusions over time could result in an excessive amount of iron within the body.
- Mismatch Reactions: Hemolytic reactions can happen when the blood transfused doesn’t match perfectly.
- Graft Vs. Host Disease is a rare ailment that occurs when immune cells from transfused host cells attack the host’s body cells.
Dialysis
Benefits:
- life-saving: Helps people suffering from renal disease the opportunity to enjoy longer more productive lives.
- Cleansing the body of waste: Removes toxins and waste products that are accumulating in the bloodstream.
- Fluid Balance: Aids in regulating fluid buildup in the body.
- Electrolyte Regulation: Maintains a healthy balance of electrolytes and minerals in the blood.
- Blood Pressure Control: Aids with regulating blood pressure.
Risks:
- Infections: In particular, at the location of vascular access during hemodialysis, or on the catheter that is used in the peritoneal dialysis.
- low blood pressure: It could be a side result of the fluid removal process in dialysis.
- Muscle Cramps: Often caused due to the rapid loss of fluids in the course of treatment.
- Peritonitis: inflammation of the belly’s lining which is a possible result of dialysis of the peritoneal area.
- Hemodialysis-Associated Amyloidosis: Chronic inflammation can lead to deposits of abnormal proteins in joints and tendons, causing pain.
- Weakness and fatigue: Common side effects following treatment, in the body’s adjustment to the changes in electrolytes and fluids.
- Long-term dependence: Without a kidney transplant, patients suffering from end-stage renal diseases remain in need of dialysis.
It’s important to know that, while there are risks involved with both blood transfusions as well as dialysis, both procedures are usually necessary and life-saving. Medical professionals are trained to reduce risks and handle any issues that might occur.
Duration and Frequency of Blood Transfusion and Dialysis
Blood Transfusion
Duration:
- The length of a blood transfusion can differ based on a variety of factors, including the amount of blood transfused, its specific component (whole blood red blood cells, plasma, platelets) as well as the patient’s medical condition.
- A typical unit consisting of red blood cells could be transfused in 1.5 up to four hours. Plasma and platelets could be transfused faster usually in 30 minutes to two hours per unit.
Frequency:
- The frequency of blood transfusions is contingent on the reason behind the transfusion.
- For instance:
- Patients suffering from chronic anemia could receive regular transfusions every couple of weeks or even months.
- People who are undergoing chemotherapy could require transfusions at the end of each cycle.
- Patients suffering from acute bleeding due to surgery or trauma could receive several units in rapid succession or in a short time.
Dialysis
- Hemodialysis:
Duration:
- A typical hemodialysis session takes approximately 3 to 5 hours.
Frequency:
- The majority of patients undergo hemodialysis 3 times per week. some may require more frequent visits.
- Peritoneal Dialysis:
Duration:
- The duration of each exchange (fill or dwell) as well as drain) will vary, but it is usually approximately 30 minutes to an hour.
- “Dwell Time” or “dwell time,” when the dialysis solution is kept in the abdomen, may be anywhere from 4 to six hours throughout the day. It could be longer at night.
Frequency:
- The number of exchanges that are required will depend on the type of dialysis peritoneal:
- Continuous Ambulatory Peripheral Dialysis (CAPD): Usually 3 to 5 exchanges throughout the day. There is also an extended stay overnight.
- Automated Peritoneal Dialysis (APD) (also known as Continuous Cycling Peritoneal Dialysis (CCPD): Conducted throughout the night using a machine generally lasting 8 to 10 hours during which the patient rests and can be supplemented by one exchange during the daytime.
It’s crucial to know that the time and frequency of dialysis as well as blood transfusion will be adapted to each patient’s requirements, based on medical evaluations and recommendations of health professionals.
Associated Costs of Blood Transfusion and Dialysis
Associated Costs of Blood Transfusion and Dialysis
The cost of both dialysis and blood transfusions will vary depending on many variables, such as the location or country of origin as well as the system of healthcare (private and public. public) as well as the needs that the person is undergoing, as well as other costs associated with ancillary services. This is a brief overview of the subject:
Blood Transfusion
- Blood as well as Blood Prices for the product: Depending on the blood component needed (whole blood red blood cells plasma, platelets, and other factors that cause clotting, etc. ) prices may vary. Particular blood types, or processed blood (like washed or irradiated red cells) may be more expensive.
- Tests and Screening: Costs for making sure that the blood is free of infectious agents and appropriate to be used by the person.
- Hospitalization and administration: The costs for hospital rooms or transfusion center, the healthcare personnel responsible for administering the transfusion, and other supplies.
- Monitor and post-transfusion care: Costs for post-transfusion care and monitoring that include tests to detect possible reactions or problems.
- Extra Treatment: When complications occur like transfusion reactions, further expenses for treatment, medication, or prolonged hospital stays might be required.
Dialysis
- Treatment Costs: Costs per dialysis treatment, which could include the cost of using the dialysis machine as well as dialyzers, solutions, and other equipment.
- Access Management: For hemodialysis, there are expenses associated with making and maintaining access to vascular blood vessels (like fistulas and grafts) that may require surgery, examinations, or possible revisions.
- home dialysis equipment: If you are in dialysis at home or peritoneal the cost is medical equipment and supplies and dialysis treatments.
- Hospital and Dialysis Center Fees: Included are facility fees as well as medical professionals’ fees.
- Monitoring and Medications: Regular blood tests to monitor the efficiency of dialysis, medication costs (like phosphate binders, erythropoiesis-stimulating agents, or vitamin D analogs), and other related treatments.
- Education: For patients opting for dialysis at home (like CAPD or home hemodialysis) There are expenses related to the required training.
- Transportation: Patients may be charged for transportation on regular visits to dialysis centers.
It is important to remember it is important to note that the coverage of insurance (public as well as private) as well as government subsidies or other charitable programs may dramatically impact the out-of-pocket costs of patients. Patients should consult with their doctor as well as their insurance company for more specific information about the charges they may be responsible for.
Conclusion
Dialysis and blood transfusions are crucial medical procedures that serve distinct functions: the first replenishes blood components while the latter is a substitute for kidney function. While both are life-saving procedures they differ in terms of duration, indications, risks, and cost.
Each procedure is individualized to the specific needs of each patient and ensures the best health outcomes. As technology advances the efficiency and safety of these procedures will increase their value in the current world of health care.