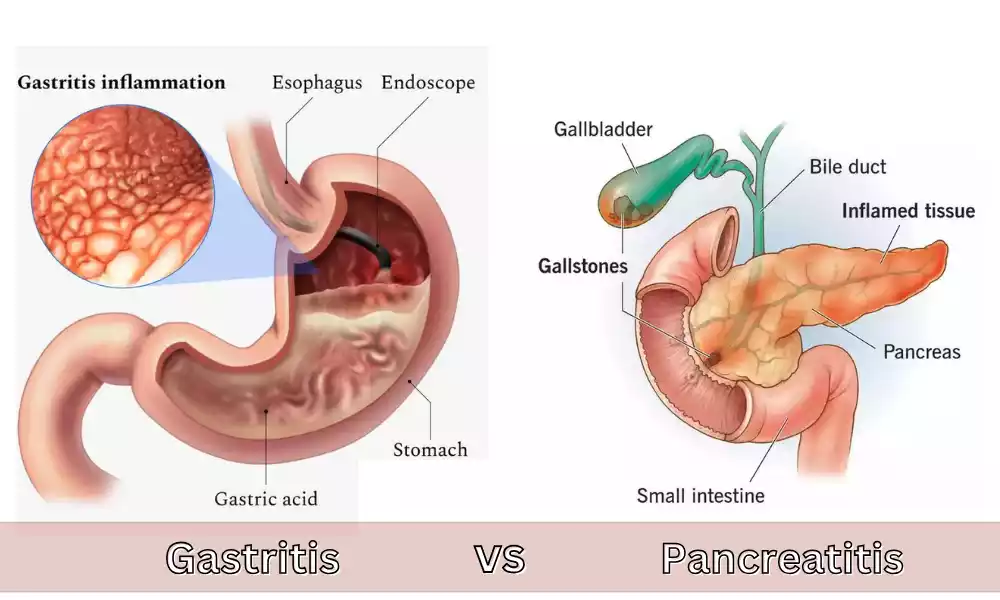
Gastritis and Pancreatitis are both inflammation-related conditions that affect the digestive system, however, they are ascribed to various organs and have distinct sources. Gastritis is the term used to describe inflammation of the stomach’s lining usually caused by infection prolonged use of certain medications or an excessive intake of alcohol.
pancreatitis is a condition that causes inflammation in the pancreas typically due to causes like gallstones, alcohol use, or other medications. Although both can be accompanied by abdominal discomfort and discomfort It’s crucial to know the difference between them to ensure a proper diagnosis and a successful treatment.
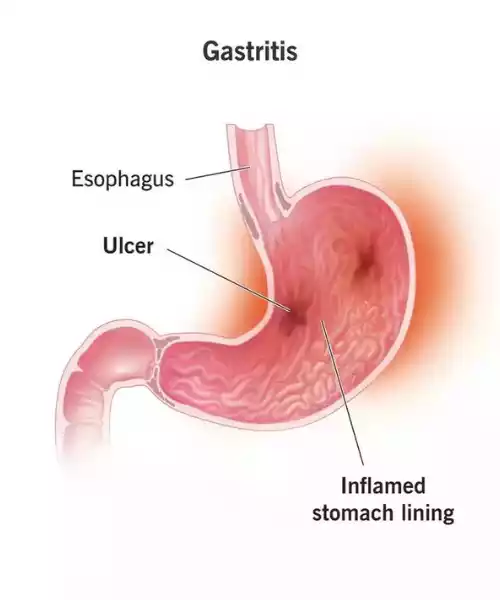
Definition of Gastritis
Gastritis is the term used to describe the irritation, inflammation, or eroding of the stomach’s lining. It can happen suddenly (acute gastritis) or progress gradually over time (chronic gastritis). The condition can cause various symptoms, which range from heartburn and indigestion to more serious complications if it is not treated.
Causes of Gastritis
-
- Helicobacter Pylori (H. Pylori) illness: One of the most prevalent causes across the globe. H. Pylori is a type of bacterium which can infect stomachs. If not treated, the infection may cause ulcers and in some instances can increase the chance of developing stomach cancer.
- Long-term usage of NSAIDs: Nonsteroidal anti-inflammatory drugs such as Ibuprofen aspirin, aspirin, and naproxen may decrease the amount of a substance that exists in the stomach. It can assist in shielding the stomach lining from acid in your stomach.
- Excessive alcohol consumption: Alcohol can irritate and damage the mucous lining of your stomach, causing acute gastritis.
- Autoimmune gastritis: The immune system of the body attacks stomach lining cells. This kind of gastritis is more frequent in those who suffer from other autoimmune conditions like Hashimoto’s Disease or type 1 diabetes.
- Bile Reflux: The backflow of bile into the stomach through the bile tract may result in gastritis.
- The causes of infections are viruses and bacteria: Besides H. Pylori, other infections caused by viruses and bacteria can cause gastritis, particularly in those who have weak immune systems.
- Stress: Extreme strain from major surgical procedures, injuries burns, or serious infections can lead to acute stress gastritis.
- Other medications: Besides NSAIDs, other drugs like corticosteroids potassium supplements, chemotherapy, and iron can irritate the stomach liner.
- Crohn’s Disease: It is an inflammatory digestive disease that may also affect the stomach, resulting in gastritis.
- Radiotherapy: Exposure to radiation caused by radiotherapy can cause gastritis.
- Another cause: Ingestion of toxic substances or foreign objects swallowed or even chronic vomiting may cause gastritis in certain instances.
It’s important to remember that often gastritis could occur without any clear root. It is essential to speak with medical professionals if anyone suspects they might have gastritis for a correct diagnosis and the appropriate treatment.
Symptoms of Gastritis
Upper abdominal discomfort or pain: It can be manifested as an aching, burning, or gnawing feeling.
- Nausea or frequent stomach upset:
- Abdominal Bloating: Swollen or full around the abdomen.
- Belching: Burping that is frequent or irregular, which can lead to the release of undigested liquid or food items.
- Vomiting: Sometimes the vomit could be bloody or display the appearance of coffee grounds, which could indicate stomach bleeding.
- Afraid loss: Feeling less hungry or not feeling the urge to eat normally.
- Feeling fuller quickly after eating:
- Loss of weight: Intentionally lost weight could be due to gastritis that affects the absorption of nutrients or decreases appetite.
- The tarry, black stool: Indicative of bleeding in the stomach that can be caused by digestive enzymes, may darken the stool.
- Indigestion or heartburn: A burning sensation in the throat or chest.
Diagnosis and Treatment of Gastritis
Diagnosis of Gastritis:
- Physical Exam: The doctor may look for tenderness in your abdomen.
- Upper endoscopy (EGD): A thin tube with cameras is inserted down the throat and into the stomach. The doctor can observe the stomach lining in real-time and, if needed collect small samples of tissue (biopsy) to be tested in a laboratory.
- Blood tests: To check for anemia (which may be caused by stomach bleeding) or to determine evidence of H. Pylori bacteria.
- Stool Test: Check for blood or H. Pylori infection.
- Breath test: When you’ve eaten a tiny portion of food that contains a radioactive element You’ll be asked to blow into a bag that will be sealed. If H. pylori is present the breath sample will be contaminated with carbon dioxide radioactive.
Treatment of Gastritis:
- Treatments to inhibit acidity production: Proton Pump Inhibitors (PPIs) such as omeprazole (Prilosec) and Lansoprazole (Prevacid) as well as Rabeprazole (Aciphex) along with esomeprazole (Nexium) can decrease your acid production. that your stomach produces.
- Treatments to lower the production of acid: Acid blockers or H2 blockers such as ranitidine (Zantac) as well as famotidine (Pepcid) and Cimetidine (Tagamet) may provide short-term relief.
- Antacids: Antacids available on the market such as Maalox, Mylanta, Rolaids, and Tums can neutralize stomach acid and offer quick relief.
- Antibiotics: When H. Pylori bacteria are identified a combination of antibiotics is prescribed to kill the bacteria.
- Stomach protection: Medications like sucralfate (Carafate) or misoprostol (Cytotec) may help protect the stomach liner.
- Avoiding irritating substances: Cutting down on the consumption of alcohol and avoiding NSAIDs instead of medication for pain can lessen the irritation.
- Dietary Changes: Smaller and more frequent meals and decreasing or removing spicy foods such as acidic foods, sour food, and caffeine can aid.
- Stopping smoking cigarettes: Smoking cigarettes can raise stomach acid, causing symptoms to worsen.
The exact treatment strategy will be based on the underlying cause that is causing the gastritis. If, for instance, gastritis is the result of prolonged NSAID usage, stopping these medications (with the guidance of a physician) might assist. If H. pylori is the source, a program of antibiotics as well as acid-suppressing medicines are typically prescribed. Always consult a healthcare professional to determine the best method of treatment for your particular situation.
Definition of Pancreatitis
Pancreatitis: Pancreatitis is an inflammation of the pancreas which is an organ behind the stomach, which produces enzymes to aid digestion as well as hormones like insulin. Pancreatitis is either acute (sudden beginning and short-lived) as well as chronic (persisting for a prolonged period).
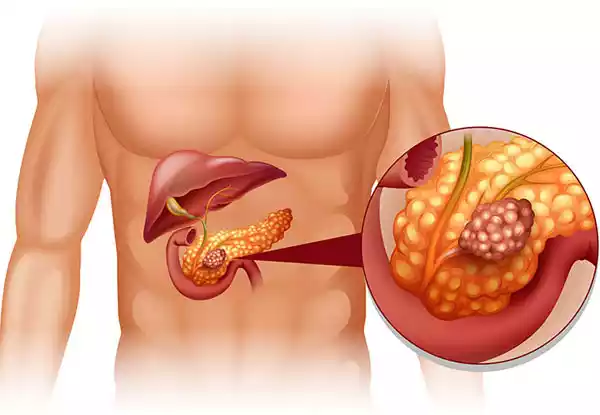
Causes of Pancreatitis
- Gallstones: Small stones-like structures that develop within the gallbladder which may stop the pancreatic duct from functioning, and cause acute pancreatitis.
- Chronic Alcohol Consumption: Long-term excessive alcohol consumption is among the main causes of chronic pancreatitis.
- Hypertriglyceridemia: Extremely high levels of triglycerides (a type of fat) in the blood can cause acute pancreatitis.
- Hypercalcemia: Increased levels of calcium present in blood. This may be caused by various diseases, such as hyperparathyroidism.
- Medicines: Some medications, for example, certain antiviral medicines diuretics, estrogens, diuretics corticosteroids, and many others, can trigger pancreatitis.
- Autoimmune diseases: Conditions where the immune system is attacking the body, like Sjogren’s or Lupus may cause pancreatitis.
- abdominal surgery or Injury: Trauma or surgery to the abdomen may cause pancreatitis.
- Diseases: A few viral illnesses such as hepatitis B or cytomegalovirus may cause pancreatitis.
- Cystic Fibrosis: Genetic disorder that leads to the formation of mucus that is thick in the pancreas and various organs.
- Pancreatic Cancer: Tumors or cancer of the pancreas may obstruct the duct and lead to pancreatitis.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A procedure used to treat gallstones can sometimes cause pancreatitis as a complication.
- Genetic Mutations: Some genetic changes could increase the chance of developing pancreatitis.
- Indiscriminate: There are instances where the reason for pancreatitis is unknown, referred to as Idiopathic Pancreatitis.
Symptoms of Pancreatitis
-
-
-
- abdominal pain: Most often, it is described as an intense, sudden pain that can radiate to the back. It is often worse following a meal, especially when you consume high-fat food items. In cases of chronic pain, the pain may be constant or even intermittent.
- Vomiting and nausea: Common symptoms accompanying the pain.
- Fièvre: Elevated body temperature is common, particularly when pancreatitis is acute.
- Rapid Pulse The heart’s rate is increased. can be seen.
- Tender and swelling abdominal area: The inflammation may cause abdominal discomfort.
- Weight Loss: Particularly when there is chronic pancreatitis where nutritional malabsorption is due to the absence of pancreatic enzymes.
- Steatorrhea: Oily or fat-laden stools that are large and smell foul. The cause is the ineffective digestion of fats because of the lower levels of enzymes released.
- Jaundice: A yellowing effect on the eyes and skin may occur when the bile duct gets blocked.
- Diabetic: Chronic pancreatitis can cause insulin resistance, which can lead to the development of diabetes.
-
-
The symptoms can differ based on whether the pancreatitis is chronic or chronic. In acute cases, symptoms can manifest suddenly and can be more severe but chronic symptoms can manifest in time and become more sporadic but persist. In both instances, immediate medical attention is vital because pancreatitis may cause grave complications if it is not treated.
Diagnosis and Treatment of Pancreatitis
Diagnosis of Pancreatitis:
- Physical Exam: The doctor may look for abdominal swelling or tenderness.
- Blood tests: To measure levels of pancreatic enzymes. The presence of elevated levels of amylase and lipase may indicate pancreatitis.
- Stool test: In the case of chronic pancreatitis and other inflammatory conditions, a test for excess fat could indicate that the digestive tract isn’t absorbing the food correctly.
- Imaging Studies:
- Abdominal Ultrasound: Sound waves form images of the pancreas.
- Endoscopic Ultrasound (EUS): A thin tube, with an attached ultrasound device is inserted down the throat to capture precise images of the pancreas.
- Magnet Resonance Imaging (MRI): Provides precise photographs of the pancreas bile ducts and pancreatic duct.
- Computed Tomography (CT) Scan: Detailed images help to detect gallstones and determine the severity of pancreas inflammation.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): A dye is injected into the pancreatic and bile ducts through an endoscope, followed by X-ray imaging.
- Genetic Tests: If hereditary pancreatitis is suspected, it’s best to test for hereditary pancreatitis.
Treatment of Pancreatitis:
- Hospitalization: The majority of patients suffering from acute pancreatitis are admitted to hospital for treatment of the disease.
- fasting: The patient will not eat for a few hours in a hospital to allow the pancreas an opportunity to heal.
- Pain Management: The relief of pain is an essential aspect of treatment. It is achieved by using drugs like acetaminophen or Ibuprofen. In some instances, stronger pain relievers might be required.
- IV Fluids: to ensure adequate water hydration and to keep blood pressure in check.
- Food and Nutritional Assistance: After the swelling is lessened, you could start a diet that has a low-fat content and is simple to digest.
- surgery: In cases related to gallstones, an operation may be required to eliminate the gallbladder. Surgery is also possible to eliminate the fluid that has accumulated in the pancreas or to remove necrotic or damaged tissue.
- Alcohol Elimination: If drinking alcohol is the main cause, abstinence is vital. Counseling or a program for treatment might be recommended.
- Enzyme Supplements: for chronic pancreatitis to aid digestion of food.
- Dietary changes: A healthy, low-fat diet can ease symptoms and help in recovery.
- Insulin and Other Medicines: To treat diabetes when it is caused by the destruction of insulin-producing cells in the pancreas.
- Do not smoke: Smoking can exacerbate the condition and cause delays in the process of recovery.
Treatment is largely contingent upon the extent and nature of pancreatitis. Monitoring and continual treatment are crucial, particularly in chronic cases to avoid or control complications.
Gastritis and Pancreatitis in the comparison chart
Here’s a comparison chart for Gastritis and Pancreatitis:
| Aspect | Gastritis | Pancreatitis |
|---|---|---|
| Definition | Inflammation, irritation, or erosion of the stomach lining. | Inflammation of the pancreas. |
| Causes | – H. pylori infection<br>- NSAIDs<br>- Alcohol<br>- Autoimmune conditions<br>- Excessive stomach acid | – Gallstones<br>- Chronic alcohol consumption<br>- High triglycerides<br>- Medications<br>- Infections<br>- Abdominal injury |
| Symptoms | – Upper abdominal pain<br>- Nausea/vomiting<br>- Bloating<br>- Loss of appetite<br>- Black, tarry stools | – Severe abdominal pain<br>- Nausea/vomiting<br>- Fever<br>- Rapid pulse<br>- Swollen abdomen<br>- Jaundice (in some cases) |
| Diagnostic Methods | – Endoscopy<br>- Blood tests<br>- Breath tests<br>- Stool tests | – Blood tests<br>- Abdominal ultrasound<br>- MRI<br>- CT scan<br>- ERCP |
| Treatment | – Acid blockers<br>- Proton pump inhibitors<br>- Antacids<br>- Antibiotics (for H. pylori) | – Hospitalization<br>- Fasting<br>- Pain management<br>- IV fluids<br>- Surgery (in some cases)<br>- Enzyme supplements |
| Complications | – Stomach ulcers<br>- Stomach tumors<br>- Stomach cancer | – Pseudocysts<br>- Infection<br>- Breathing issues<br>- Diabetes<br>- Kidney failure |
| Associated Conditions | – Pernicious anemia | – Cystic fibrosis<br>- Hereditary pancreatitis |
| Prevention | – Limit NSAID use<br>- Moderation in alcohol<br>- Eat smaller meals<br>- Manage stress | – Avoid excessive alcohol<br>- Maintain a healthy diet<br>- No smoking |
Note: This chart provides a general overview of gastritis and pancreatitis. The information is not exhaustive, and individual experiences with each condition may vary. Always consult a healthcare professional for a comprehensive understanding and diagnosis.
The importance of distinguishing between the two
Differentiating between gastritis as well as pancreatitis is vital for many reasons:
- Accurate diagnosis and treatment: The signs of pancreatitis and gastritis may be similar, but their causes, treatment, and management are different. A correct diagnosis will ensure that the correct treatment is taken immediately to address the underlying cause of the problem.
- Preventing complications: Gastritis and pancreatitis can cause serious complications if they are not treated properly or if the incorrect condition is addressed. Pancreatitis, for instance, may progress into pseudocysts or pancreatic necrosis while gastritis could result in stomach ulcers and a higher chance of developing stomach cancer. Early intervention can reduce or prevent these problems.
- Optimizing the use of medications: The drugs that are used to treat gastritis and pancreatitis can vary. Making the wrong choice of medication or treatment strategy could prove detrimental or even ineffective. For example, certain medications for treating gastritis, like NSAIDs, can aggravate pancreatitis.
- Lifestyle and Dietary Modifications: Patients suffering from gastritis might need to adhere to specific diet guidelines to minimize irritation to the stomach lining. On the other hand, patients suffering from pancreatitis might require a diet low in fat to help ease the strain on the digestive tract. Differentiating between these two types of conditions will ensure that patients are provided with individualized dietary and lifestyle suggestions.
- Monitoring and Follow-up: Patients suffering from pancreatitis can require monitoring, particularly in cases of chronic occurrence to control complications such as malabsorption or diabetes. An accurate diagnosis will ensure that necessary follow-up treatment is offered.
- Prevention of mistaken diagnosis: A misdiagnosis of one condition for another can cause unnecessary treatment delay in the appropriate treatment as well as increased costs for healthcare. Making sure that misdiagnosis is avoided is crucial to the efficient and effective delivery of healthcare.
- Educational Patient: Accurate diagnosis allows health professionals to inform patients about their health condition, and its causes along with the necessity of adhering to the treatment plan and lifestyle guidelines. This allows patients to be active participants in their treatment.
The distinction between pancreatitis and gastritis is essential to ensure that patients are provided with the appropriate diagnosis, treatment, and treatment strategies. This does not only improve the outcomes of patients but can help avoid potential complications and lower the cost of healthcare that is caused by incorrect diagnosis and poor treatment.
Conclusion
Knowing the main differentiators between pancreatitis and gastritis is crucial for a precise diagnosis and proper treatment. Differentiating between these two conditions will ensure that patients receive the appropriate treatment, decrease the chance of complications, and encourage improved overall health outcomes.