Definition and Terms of Prediabetes and Diabetes
Definition and Terms of Prediabetes and Diabetes
- Prediabetes:
- Definition: A metabolic condition characterized by blood sugar levels that are higher than normal but not yet high enough to qualify as diabetes.
- Key Terms:
- Impaired Fasting Glucose (IFG): A fasting blood glucose level between 100 mg/dL (5.6 mmol/L) and 125 mg/dL (6.9 mmol/L).
- Impaired Glucose Tolerance (IGT): Blood glucose levels that are higher than normal two hours after an oral glucose tolerance test, specifically between 140 mg/dL (7.8 mmol/L) and 199 mg/dL (11.0 mmol/L).
- Insulin Resistance: A condition in which the body’s cells become less responsive to the insulin produced by the pancreas, leading to higher blood sugar.
- HbA1c (Glycated Hemoglobin): A test that measures the average blood sugar level over the past 2-3 months. Prediabetes is indicated by an HbA1c value between 5.7% and 6.4%
- Diabetes:
- Definition: A chronic metabolic disorder where the body either doesn’t produce enough insulin or can’t effectively use the insulin it does produce, resulting in high blood sugar levels.
- Key Terms:
- Type 1 Diabetes: An autoimmune condition where the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. It typically appears in childhood or adolescence.
- Type 2 Diabetes: A more common form of diabetes wherein the body becomes resistant to insulin and/or the pancreas cannot produce enough insulin. Often associated with older age, obesity, family history, and lack of exercise.
- Gestational Diabetes: Elevated blood sugar levels during pregnancy, which can pose risks to both mother and child.
- Insulin: A hormone produced by the pancreas that helps regulate blood sugar levels by facilitating the uptake of glucose into cells.
- Hyperglycemia: Elevated blood sugar levels, a key feature of diabetes.
- Diabetic Ketoacidosis (DKA): A serious condition that can develop in people with type 1 diabetes due to a lack of insulin, leading to the breakdown of fat for energy and resulting in a buildup of ketones in the blood.
- HbA1c (Glycated Hemoglobin): A test that measures the average blood sugar level over the past 2-3 months. Diabetes is diagnosed when the HbA1c level is 6.5% or higher.

Understanding these terms is pivotal in grasping the intricacies of both prediabetes and diabetes, and it aids in the effective management and communication of these conditions.
Prediabetes and Diabetes in the comparison chart
Here’s a comparison chart outlining the differences between prediabetes and diabetes:
| Criteria | Prediabetes | Diabetes |
|---|---|---|
| Definition | Elevated blood sugar levels, but not high enough for a diabetes diagnosis. | Chronic condition with persistently high blood sugar levels. |
| Blood Sugar Levels | Fasting blood glucose: 100-125 mg/dL (5.6-6.9 mmol/L) – 2 hours post-OGTT: 140-199 mg/dL (7.8-11.0 mmol/L) HbA1c: 5.7% to 6.4% | Fasting blood glucose: ≥126 mg/dL (≥7.0 mmol/L) – 2 hours post OGTT: ≥200 mg/dL (≥11.1 mmol/L) – HbA1c: ≥6.5% |
| Symptoms | Often asymptomatic or subtle signs. | Thirst, frequent urination, fatigue, blurred vision, slow healing wounds, etc. |
| Risk Factors | Obesity, sedentary lifestyle, high triglycerides, low HDL, high blood pressure, family history. | Similar to prediabetes plus progression from untreated prediabetes, genetic factors, autoimmune reactions (Type 1), etc. |
| Potential Complications | Progression to diabetes, increased risk of heart disease. | Heart disease, neuropathy, nephropathy, retinopathy, foot ulcers, increased infection risk, etc. |
| Management | Lifestyle modifications (diet, exercise), monitoring blood sugar levels. | Depending on type: insulin injections, oral medications, lifestyle modifications, regular monitoring, etc. |
| Prevention | Weight management, balanced diet, physical activity, regular screening. | Early diagnosis and treatment of prediabetes, maintaining a healthy lifestyle, and regular screenings. |
Importance of early detection and intervention
The importance of early detection and intervention for conditions like prediabetes and diabetes cannot be overstated. Recognizing and addressing these issues at an initial stage can prevent or delay the progression of the disease, reduce the risk of complications, and improve the overall prognosis.
Here are some key reasons why early detection and intervention are crucial:
- Prevention of Progression:
- Prediabetes: Early identification and management can prevent or delay the progression of type 2 diabetes. Lifestyle modifications, such as dietary changes and increased physical activity, can revert blood glucose levels to the normal range.
- Diabetes: Early intervention can prevent or delay the onset of complications associated with poorly controlled diabetes.
- Reduction of Complications:
- Early detection and management can reduce the risk of complications such as cardiovascular diseases, kidney damage (nephropathy), nerve damage (neuropathy), eye damage (retinopathy), and foot problems.
- Economic Savings:
- Early detection and intervention can reduce the financial burden on healthcare systems. Managing complications associated with advanced diabetes is often more expensive than early treatment and preventive measures.
- Improved Quality of Life:
- Timely management can prevent symptoms like excessive thirst, frequent urination, fatigue, and blurred vision, which can impact daily life. It can also prevent more severe outcomes such as hospitalizations for conditions like diabetic ketoacidosis or hyperosmolar hyperglycemic state.
- Optimal Management:
- Early diagnosis provides a window of opportunity to establish effective self-management practices, such as glucose monitoring, dietary adjustments, and exercise routines. This foundation is crucial for long-term disease management.
- Psychological Well-being:
- Knowledge of one’s condition and having the tools and resources to manage it can reduce anxiety and stress associated with uncertainty or unexplained health issues.
- Educational Opportunities:
- Early detection provides ample time for patients to educate themselves about their condition, making them active participants in their care, and leading to better compliance and outcomes.
- Prevention of Associated Conditions:
- Effective early management of blood sugar levels can also reduce the risk of associated conditions, such as high blood pressure and elevated cholesterol levels, which are common among people with diabetes.
- Reduced Mortality:
- Early intervention reduces the risk of life-threatening complications and, consequently, mortality associated with diabetes.
Early detection and intervention in prediabetes and diabetes are instrumental in halting or slowing disease progression, preventing complications, ensuring a better quality of life, and reducing both economic and health burdens.
Causes and Risk Factors
Prediabetes: Prediabetes is essentially a wake-up call, an amber light warning that without intervention, one is on the road to developing type 2 diabetes.
Its causes and risk factors include:
- Insulin Resistance: This is where the body’s cells don’t respond to insulin as effectively as they should.
- Genetics: A family history of diabetes can elevate the risk of prediabetes. Certain genes also make individuals more susceptible.
- Age: While it can occur at any age, the risk increases after the age of 45.
- Sedentary Lifestyle: Physical inactivity leads to weight gain and increases insulin resistance.
- Diet: High-calorie, high-fat, and low-fiber diets contribute to the risk of prediabetes.
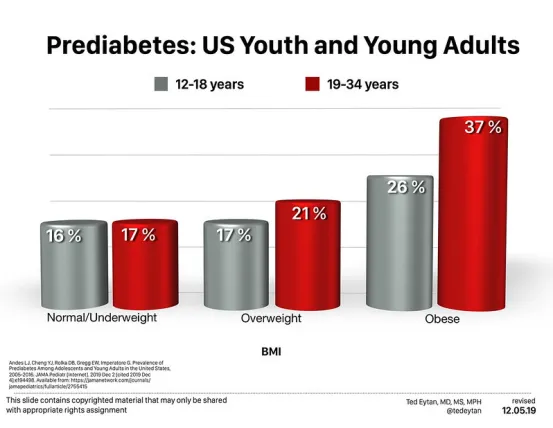
- Obesity: Especially central obesity, where fat accumulates around the abdomen, elevates the risk.
- Other Factors: These include conditions like polycystic ovary syndrome (PCOS), high blood pressure, and elevated cholesterol levels.
Diabetes: The causes of diabetes are more varied, depending on the type:
- Type 1 Diabetes: It is an autoimmune condition. The body mistakenly attacks and destroys insulin-producing beta cells in the pancreas. The exact cause remains unknown, but it’s believed to involve a combination of genetic and environmental factors, possibly viruses.
- Type 2 Diabetes: This form arises from a combination of genetics, lifestyle factors, and environmental elements. The same factors that increase the risk of prediabetes escalate the risk of type 2 diabetes.
- Gestational Diabetes: Occurs during pregnancy. Causes might include the presence of certain pregnancy hormones that induce insulin resistance, coupled with a shortage of insulin production.
Signs and Symptoms
Prediabetes: The insidious nature of prediabetes is that it often manifests with little to no overt symptoms.
However, some subtle signs can be noted:
- Acanthosis Nigricans: Darkened areas of skin, usually in the neck, armpits, elbows, and knuckles.
For many, symptoms only become noticeable when they escalate into diabetes, emphasizing the importance of regular check-ups.
Diabetes: The signs and symptoms of diabetes are more pronounced and can include:
- Increased Thirst and Urination: Elevated blood sugar levels lead to increased urine production, causing dehydration and, consequently, increased thirst.
- Hunger: Despite eating, the inability of cells to receive glucose triggers hunger.
- Fatigue: Insufficient sugar in the cells can lead to tiredness.
- Slow Healing: High blood sugar affects wound healing and increases the risk of infections.
- Tingling or Pain in the Feet or Hands: This can be an early sign of nerve damage (neuropathy).
Diagnostic Criteria
Prediabetes: To diagnose prediabetes, medical professionals rely on the following tests:
- Fasting Blood Sugar Test: Blood sugar levels are checked after an overnight fast. A level between 100 mg/dL (5.6 mmol/L) and 125 mg/dL (6.9 mmol/L) suggests prediabetes.
- Oral Glucose Tolerance Test (OGTT): After fasting, you’ll drink a sugary solution, and blood sugar levels are then tested several times over the next few hours. A level between 140 mg/dL (7.8 mmol/L) and 199 mg/dL (11.0 mmol/L) two hours after drinking the solution indicates prediabetes.
- HbA1c: This test gauges the average blood sugar level over the past 2 to 3 months. A level between 5.7% and 6.4% indicates prediabetes.
Diabetes: The same tests are used for diabetes, but the values that determine the diagnosis are different:
- Fasting Blood Sugar Test: A level of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes.
- Oral Glucose Tolerance Test: A level higher than 200 mg/dL (11.1 mmol/L) two hours after the drink signifies diabetes.
- HbA1c: A result of 6.5% or higher confirms diabetes.
Random blood sugar tests and screening for antibodies (in the case of Type 1 diabetes) can also be utilized.
Potential Complications
- Prediabetes:
Prediabetes might sound benign given its ‘pre’ prefix, but it is not without its risks. Complications associated with prediabetes include:
- Progression to Diabetes: If not managed properly, prediabetes can transition into type 2 diabetes, a more severe metabolic disorder.
- Cardiovascular Issues: People with prediabetes have a higher risk of heart disease and stroke even if they don’t progress to diabetes.
- Diabetes:
The complications of diabetes are varied and more severe, especially if the condition is poorly managed:
- Cardiovascular Diseases: Diabetes increases the risk of various cardiovascular problems, including coronary artery disease, heart attack, stroke, narrowing of the arteries, and more.
- Neuropathy: Elevated sugar levels can cause nerve damage, leading to tingling or numbness, especially in the extremities like feet.
- Nephropathy: Diabetes can damage the kidney’s filtering system, leading to kidney failure or irreversible end-stage kidney disease.
- Retinopathy: Diabetes can damage blood vessels of the retina, potentially leading to blindness.
- Foot Damage: Nerve damage or poor blood flow to the feet increases the risk of various foot complications, from fungal infections to severe ulcers that require amputation.
- Skin and Mouth Conditions: Diabetes may make one more susceptible to skin problems, including bacterial and fungal infections.
- Bone and Joint Problems: Diabetes may lead to a higher risk of bone fractures and osteoporosis.
Management and Treatment
- Prediabetes:
Management primarily focuses on halting its progression:
- Lifestyle Modifications: Incorporating a balanced diet and regular exercise is crucial. Losing even a small percentage of body weight can significantly reduce the risk of developing diabetes.
- Monitoring: Regular check-ups to monitor blood sugar levels are recommended to ensure they remain within a safe range.
- Diabetes:
Treatment involves a more comprehensive approach:
- Medication and Insulin Therapy: Depending on the type of diabetes, one might need to take oral medications or insulin injections to regulate blood sugar levels.
- Blood Sugar Monitoring: Regular and sometimes daily monitoring is essential to ensure sugar levels are within target ranges.
- Healthy Lifestyle: Like prediabetes, a balanced diet and regular exercise play a crucial role in managing diabetes.
- Regular Check-ups: Routine visits to healthcare providers are essential for monitoring potential complications.
Prevention Strategies
- Prediabetes:
- Weight Management: Maintaining a healthy weight is crucial as obesity is a significant risk factor.
- Balanced Diet: Opt for whole grains, and lean proteins, and avoid refined sugars and saturated fats.
- Physical Activity: Engage in at least 150 minutes of moderate-intensity exercise per week.
- Diabetes:
- Early Intervention in Prediabetes: Managing prediabetes effectively is a significant preventive strategy against type 2 diabetes.
- Regular Screenings: Especially if there are risk factors, regular screenings can lead to early detection and management.
- Avoid Tobacco: Smoking increases the risk of type 2 diabetes. Quitting reduces this risk considerably.
Conclusion
Prediabetes and diabetes, though closely related, stand apart in their implications, management, and preventive strategies. Understanding the subtle and overt differences between the two is vital for everyone, whether for personal health, caregiving, or general knowledge.
Prediabetes serves as an essential warning sign — a bellwether indicating that without intervention, more significant health issues loom on the horizon. Meanwhile, diabetes, with its potential complications, stresses the need for robust management and lifestyle modifications.
The shared narrative of both conditions underscores the importance of early detection, proactive health management, and lifestyle choices conducive to metabolic health. With the right knowledge and resources, both prediabetes and diabetes can be managed effectively, ensuring a better quality of life.
