The most common malignancies in the world are skin cancers. They come in many subtypes, each with their distinct characteristics. Keratoacanthoma and Squamous Cell Carcinoma are two skin lesions that can be difficult to diagnose.
Understanding the differences between these entities, despite their similarity in appearance and presentation is essential for an accurate diagnosis and proper management. This outline will explore the differences between KAs and SCCs, allowing for better differentiation and ensuring that patients receive optimal care.
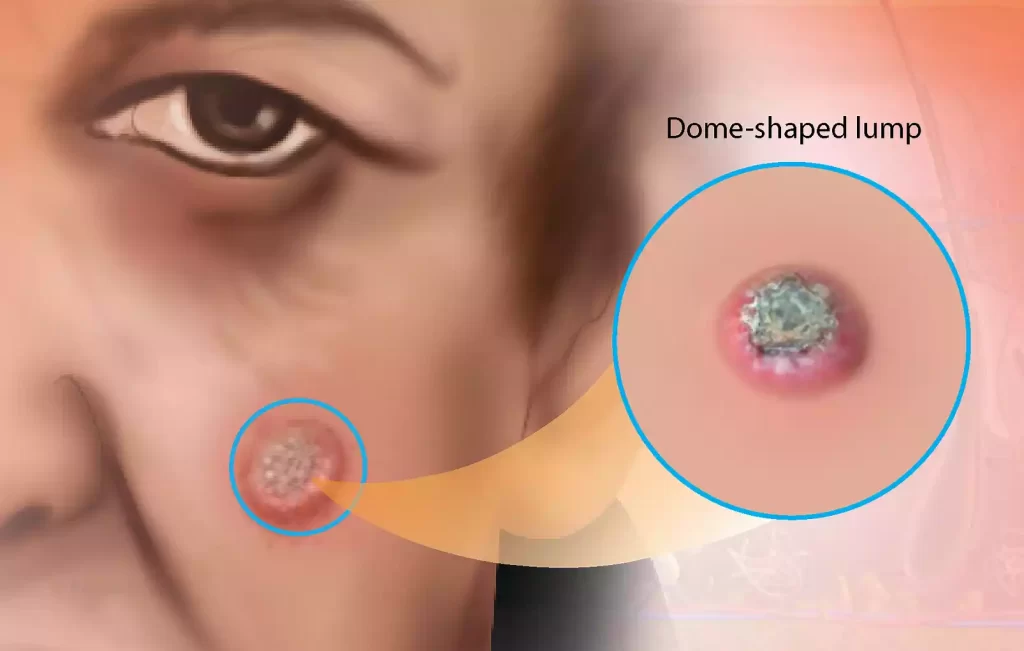
What is Keratoacanthoma (KA)?
Keratoacanthoma is a skin tumor or lesion that develops in the hair follicles, or on the epidermis (outermost layer). It’s a benign growth, but its rapid growth and initial appearance can make it look alarming.
Keratoacanthoma has some important characteristics and information:
- Rapid growth: One of the defining characteristics of KA, is its rapid expansion over weeks or months. It usually starts as a small flesh-colored bump or pink and can grow significantly over time.
- Dome Shape: The KAs have a dome shape with a central depression. This central depression can be filled with keratin, a thick white or yellowish substance.
- Location: KAs can be found in areas that are exposed to the sun, including the face, neck, and arms.
- Symptoms: Although KAs are usually painless, mild tenderness or itching can occur.
- Regression: Many KAs will spontaneously regress after reaching a certain height. They can shrink and the central keratin may fall out leaving a scar.
- Risk factors: KAs tend to be more prevalent in people with fair skin. Also, they are more common in older age groups.
- Differential Diagnoses: Because of the rapid growth and appearance of KA, it can be confused with SCC, an aggressive form of skin cancer. It is important to distinguish between KAs and SCCs for the right management.
- Diagnosis: The diagnosis of KA is usually made through a biopsy. This involves the removal and examination under a microscopical microscope of a small sample. This can help confirm the diagnosis, and exclude other skin conditions such as SCC.
- Treatment: Depending on the location, size, and patient characteristics, KA management can be different. Some treatment options include surgical excision (some KAs regress on their own), cryotherapy (freezing of the lesion), or laser therapy.
While KAs may initially resemble SCC, they tend to follow a benign course that resolves without aggressive treatment. A proper diagnosis is essential for ensuring appropriate care.
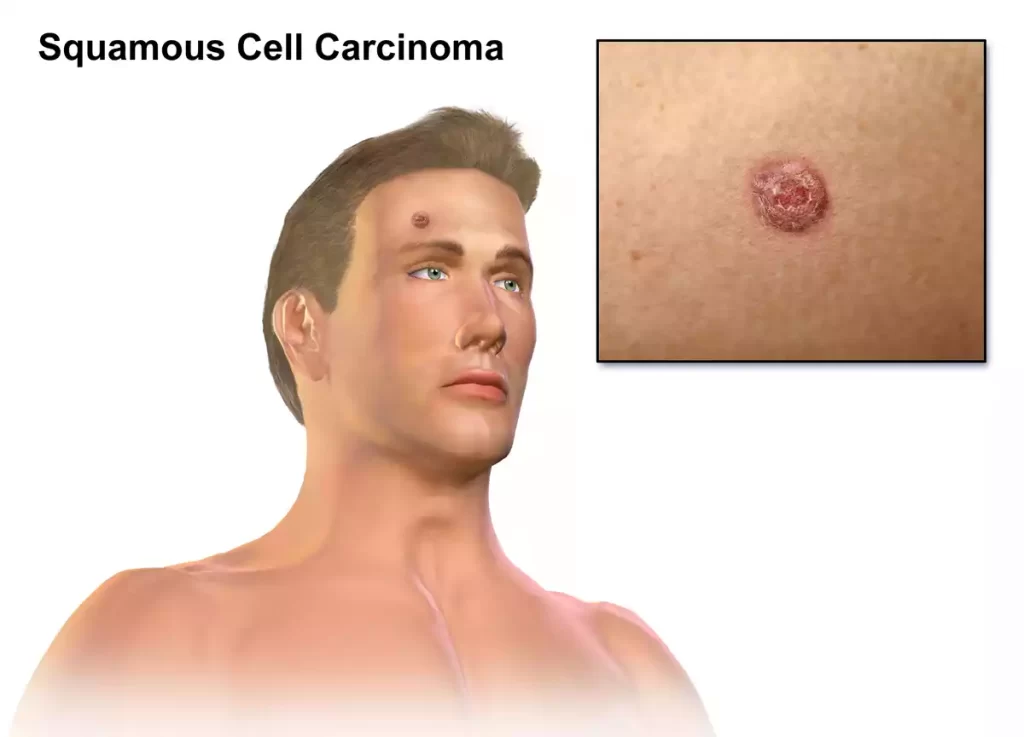
What is Squamous Cell Carcinoma (SCC)?
Squamous Cell Carcinoma (SCC) is a type of skin cancer that arises from the squamous cells, which are flat, thin cells found in the outermost layer of the skin (epidermis). SCC is one of the most common forms of skin cancer and is generally more aggressive than basal cell carcinoma but less aggressive than melanoma.
Here are key characteristics and information about Squamous Cell Carcinoma:
- Malignant Tumor: SCC is a malignant tumor, meaning it can invade nearby tissues and, in some cases, metastasize (spread) to other parts of the body if left untreated.
- Risk Factors: Several risk factors increase the likelihood of developing SCC, including prolonged and repeated exposure to ultraviolet (UV) radiation from the sun or artificial sources (tanning beds). Other risk factors include a history of precancerous skin lesions, a weakened immune system, older age, and certain genetic factors.
- Clinical Presentation: SCC often appears as a firm, red, scaly bump or nodule on the skin. It may also manifest as a non-healing sore, ulcer, or rough patch.
- Location: SCC can occur on any part of the body but is most frequently found on sun-exposed areas, such as the face, ears, neck, scalp, chest, back of the hands, and lower lip.
- Symptoms: Patients with SCC may experience symptoms such as tenderness, pain, itching, or bleeding at the site of the lesion.
- Growth: Unlike Keratoacanthoma (KA), SCC typically grows more slowly and progressively. It may enlarge over several months or years.
- Diagnosis: The diagnosis of SCC is usually confirmed through a skin biopsy. A small sample of the lesion is removed and examined under a microscope to determine if cancerous cells are present.
- Staging and Prognosis: SCC can be staged to assess the extent of its spread, with stages ranging from I (localized) to IV (advanced). Prognosis varies depending on the stage at diagnosis and the presence of risk factors, but early detection and treatment generally lead to better outcomes.
- Treatment: The treatment of SCC depends on its size, location, stage, and individual patient factors. Common treatment options include surgical excision (removal), Mohs micrographic surgery (a specialized surgical technique for precise removal), radiation therapy, and, in advanced cases, chemotherapy or targeted therapy.
- Prevention: Sun protection measures, such as wearing sunscreen, and protective clothing, and avoiding excessive sun exposure, are crucial in reducing the risk of SCC. Regular skin examinations and self-checks can help detect and address skin lesions early.
SCC is a serious skin cancer that should not be ignored. Early detection, prompt treatment, and preventive measures can significantly improve the prognosis and reduce the risk of complications associated with this type of skin cancer.
Keratoacanthoma and Squamous Cell Carcinoma comparison chart
Here’s a comparison chart highlighting the key differences between Keratoacanthoma (KA) and Squamous Cell Carcinoma (SCC):
| Characteristic | Keratoacanthoma (KA) | Squamous Cell Carcinoma (SCC) |
|---|---|---|
| Nature | Benign tumor with potential for spontaneous regression | Cancer with invasive potential |
| Growth Rate | Rapid growth over weeks to months | Slower, progressive growth |
| Appearance | Dome-shaped with a central keratin plug | Firm, red, scaly bumps or nodules, can ulcerate or crust |
| Risk Factors | Sun exposure, fair skin, older age | Sun exposure, precancerous lesions, weakened immune system, age |
| Location | Sun-exposed areas (face, neck, arms) | Sun-exposed areas, mucous membranes |
| Symptoms | Generally painless, mild itching or tenderness possible | May be tender, itchy, painful, or bleed |
| Regression | Spontaneous regression in many cases | Does not spontaneously regress |
| Diagnosis | Skin biopsy | Skin biopsy |
| Staging and Prognosis | Not typically staged; generally favorable prognosis | Staged based on the extent of invasion, the prognosis varies with stage |
| Treatment Options | Observation, surgical excision, cryotherapy, laser therapy | Surgical excision, Mohs micrographic surgery, radiation therapy, chemotherapy (in advanced cases) |
| Metastasis Risk | Rarely metastasizes | Can metastasize if left untreated |
| Importance of Distinction | Ensures appropriate management and avoids overtreatment | Ensures timely and appropriate treatment, improves prognosis |
| Patient Impact | Minimal emotional distress due to benign nature | Higher emotional distress due to cancer diagnosis |
| Healthcare Costs | Lower healthcare costs due to less aggressive treatment | Higher healthcare costs due to more intensive treatment |
Importance of distinguishing between keratoacanthoma and squamous cell carcinoma (SCC)
It is vital to distinguish between Keratoacanthoma and Squamous Cell Carcinoma in clinical practice, for several reasons.
- Treatment Method:
- Keratoacanthoma: can be a self-limiting lesion and may even regress by itself. Some KAs may not require aggressive treatment. They can be treated conservatively and with observation.
- Squamous cell carcinoma (SCC): is a malignant form of cancer that requires immediate and appropriate treatment. Squamous cell carcinoma (SCC) can spread to deeper tissues or even to other parts.
- Patient anxiety and quality of life:
- A misdiagnosis of KA as SCC may cause patients unnecessary anxiety and distress. SCC is associated with cancer, which can cause increased fear and anxiety.
- SCC patients require aggressive treatment, which can affect their quality of living due to surgery or radiation therapy. It is best to avoid overtreatment of patients when it is not necessary.
- Healthcare Costs:
- If KA is misdiagnosed as SCC, it can lead to additional costs for unnecessary surgeries, procedures, or treatments.
- Resource Allocation:
- SCC requires a different level and type of medical care than KA. By correctly identifying SCC, healthcare providers can allocate resources to aggressive cancers and not overload the healthcare system by treating benign or less aggressive cases.
- Research and Data Quality:
- For clinical research and epidemiological studies, an accurate diagnosis is crucial. A misclassification of KA as SCC may lead to distorted data that makes it difficult to determine the true prevalence and outcome of these conditions.
- Legal Considerations:
- A misdiagnosis of a benign condition can have ethical and legal implications for healthcare providers. Legal action may be pursued by patients who believe they have experienced unnecessary treatment or emotional trauma as the result of misdiagnosis.
- Long-term health outcomes:
- Early diagnosis and treatment of SCC will improve the long-term outcome of the disease and the chance of a cure.
- Public Awareness and Education:
- By educating the public on the difference between benign and malignant lesions of the skin, we can promote skin health and encourage individuals to seek medical attention for any suspicious growth.
It is important to distinguish between Keratoacanthoma (skin cancer) and Squamous-Cell Carcinoma to achieve accurate diagnosis, optimal treatment, and patient outcomes. Healthcare professionals must carefully evaluate and differentiate these skin lesions to provide the best possible care for patients while minimizing emotional distress and unnecessary interventions.
Clinical Importance of Accurate Diagnosis
Accurate diagnosis is crucial for healthcare because it can have a wide-ranging impact on patient care, treatment outcomes, and healthcare systems. Here are some key reasons why an accurate diagnosis is important:
- Appropriate treatment: An accurate diagnosis helps healthcare providers select the best treatment plan to treat a specific patient’s condition. The treatment plan will be more effective if it is tailored to the patient’s diagnosis. This reduces the need for unnecessary medications or procedures.
- Patient safety: A correct diagnosis can help ensure patient safety by avoiding interventions or treatments that may have risks, side effects, or complications. This reduces the chance of missing serious medical conditions that need immediate attention.
- Optimal Health Outcomes: Accurate diagnoses improve the odds of optimal health outcomes. Early and targeted interventions improve the chances of a successful outcome, a better quality of life, and fewer long-term complications.
- Resource Utilisation: This helps to allocate healthcare resources more efficiently. Accurate diagnosis prevents the overuse of resources for misdiagnosed patients and allows healthcare systems to concentrate their efforts and resources in areas where they are most needed.
- Cost Effectiveness: By avoiding misdiagnoses, and ineffective treatments, patients and the healthcare system can save money. Unnecessary treatments, tests, and hospitalizations can be costly for patients and burdensome.
- Patient satisfaction: Patients who receive an accurate diagnosis, and the appropriate treatment are more satisfied with their healthcare. It improves the patient-provider relationship and fosters trust.
- Preventative care: A correct diagnosis can identify risk factors or conditions that require lifestyle changes or preventative measures to reduce future health risks.
- Public Health and Epidemiology: Accurate diagnosis contributes to the accuracy and reliability of epidemiological data. This allows healthcare authorities to monitor trends in disease, plan public health interventions, and effectively allocate resources.
- Legal Considerations: Accurate diagnoses are essential both for ethical and legal reasons. Medical malpractice claims, legal liability, and ethical dilemmas are all possible if a misdiagnosis occurs.
- Continuity: Accurate diagnosis documentation ensures healthcare providers have an understanding of the patient’s medical background, allowing for better continuity of care in the future and more informed decision-making.
- Research and Development: Accurate diagnosis plays a crucial role in medical research. It allows for the identification of specific patient groups for clinical trials. This leads to new treatments and advances in medical knowledge.
- Psychosocial Effect: Misdiagnosis can cause anxiety, depression, and emotional distress in patients and their family members. Accurate diagnosis can help reduce these psychological effects.
Accurate diagnosis is the foundation of effective healthcare. This has a direct impact on patient safety, satisfaction, and well-being. It also benefits healthcare systems, research, and public health. Accurate diagnoses are a key component of high-quality care.
Conclusion
Accurate diagnosis ensures appropriate treatment, patient security, and optimal outcomes. Accurate diagnosis is crucial for preserving resources, fostering patient satisfaction, and promoting public health. To deliver high-quality healthcare and promote well-being, healthcare systems, and providers need to prioritize and maintain the accuracy of diagnoses.
