Definition of breast cancer
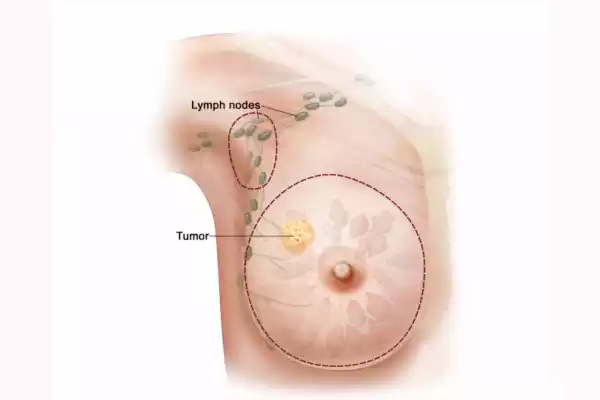
Breast cancer is malignant (cancer) and originates from the cells in the breast. The breast tissue is affected, including the glands (lobules), which produce milk, and the ducts transporting milk to the nipple. Breast cancer may also develop in the connective and fatty tissue of the breast.
Breast cancer is caused by abnormal cells that grow uncontrollably in the breast. These cells form a mass or tumor. These cancerous cells may invade healthy tissue and spread to other areas of the body via the lymphatic or bloodstream over time.
Breast cancer affects women more than men, although it is less common. Breast cancer can be treated more successfully if it is detected early through mammograms and other screenings. Treatment options for breast carcinoma may include radiation therapy, chemotherapy, and hormone therapy.
Stage 2 Breast Cancer
Stage 2 breast carcinoma is a stage in breast cancer where the cancer has spread beyond the initial tumor, but not to distant organs and tissues. The stage is further subdivided into Stages 2A and 2B depending on the size and extent of the lymph node involvement.
Stage 2 breast cancer – Key characteristics and information
1. Tumor Size: The size of the tumor can vary, but it is usually larger in stage 2 than in earlier stages. However, the primary tumor remains confined to either the breast or the nearby lymph nodes. Tumor size can vary but is usually between 2 and 5 centimeters.
2. Lymph Node involvement:
- Stage 1A: A tumor can be small but involves nearby lymph nodes, usually axillary lymph nodes or underarm nodes. It may also be large but not lymph node-involved.
- Stage 2B The tumor may be larger than stage 2A and may also involve lymph nodes nearby, but the extent to which lymph nodes are involved varies.
3. Breast Cancer Has Not Spread to Distant Organs or Tissues: At this stage breast cancer has not spread beyond the breast and adjacent lymph nodes.
4. 4. Symptoms: Stage 2 breast cancer can cause symptoms like a lump in the breast, changes to the breast’s size or shape, changes in skin over the breast or pain. Some women may not show any symptoms at all, which highlights the importance of routine breast cancer screenings.
5. Diagnosis: A combination of imaging tests, such as mammography or ultrasound, and a biopsy is usually used to diagnose cancer.
6. Treatment Options:
- Surgery: The majority of individuals with stage 2 breast cancer undergo surgery to remove their tumor. The procedure may include a lumpectomy, which involves removing the tumor along with the surrounding tissue. A mastectomy is also possible.
- Radiotherapy: After surgery, radiation therapy can be used to reduce the risk of cancer recurrence by targeting any cancer cells that remain.
- Chemotherapy: Patients with Stage 2 breast carcinoma, particularly those with larger tumors or lymph node involvement, will receive chemotherapy in order to eradicate any remaining cancer cells.
- Hormone Treatment: In cases where the cancer is hormone-receptor-positive, hormone therapy can be prescribed to block the hormones that are fueling cancer growth.
- Targeted Treatment: When cancer cells overexpress the HER2 proteins, targeted therapies like Herceptin can be used.
7. Prognosis: The prognosis of Stage 2 breast cancer depends on factors such as tumor size, lymph node involvement, hormone receptor, and HER2 status. In general, stage 2 breast cancer can be treated and the outlook for this stage is better than that of more advanced stages. The five-year survivability rate for Stage 2 is high, but the individual outcome can vary.
Individuals diagnosed with Stage 2 Breast Cancer must work closely with their healthcare provider to develop a customized treatment plan. They should also engage in regular follow-up care to check for signs of metastasis or recurrence. Early detection and timely treatments can improve outcomes for those with Stage 2 Breast Cancer.
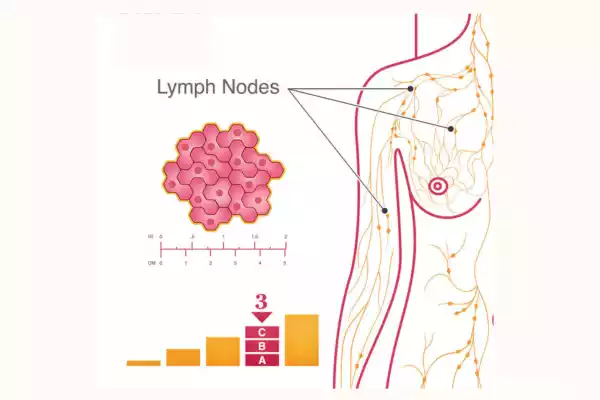
Stage 3 Breast Cancer
Stage 3 breast carcinoma is an advanced form of breast cancer where the cancer has spread to lymph nodes or other tissues in the chest or underarm region. This stage can be further subdivided into Stage 3A (the most common), Stage 3B (the second most common), and Stage 3C (the third most common) depending on factors such as the size of tumors, lymph node involvement, and other factors.
Here are some important characteristics and details:
1. Tumor Size: The tumor size can vary. In stage 3 breast cancer the primary tumor may be larger than earlier stages, and it could have spread to nearby tissues such as the chest wall or the skin. The size of the tumor can vary.
2. Lymph Node involvement:
- Stage 3A: The cancer has spread to lymph nodes below the collarbone or near the breastbone.
- Stage 3B: The tumor could have invaded either the skin or chest wall and it may or not have involved lymph nodes.
- Stage 3C: This stage indicates the presence of cancerous cells in lymphatic vessels on the chest wall and underarms, regardless of tumor size.
3. No distant metastasis: Breast cancer in Stage 3 has not spread to distant organs and tissues (M0) outside of the breast or nearby lymph nodes.
4. Symptoms: Stage 3 breast cancer patients may have symptoms like a lump in the breast, changes to the breast’s size or shape, skin changes around it, nipple discharge or pain. These symptoms can be more severe than those of earlier stages.
5. Diagnosis: A combination of imaging tests, such as mammography or ultrasound, and a biopsy is used to confirm the cancer’s presence and determine its characteristics.
6. Treatment Options:
- Surgery: Surgery may be part of a treatment plan. It can involve more complex procedures such as a mastectomy and removal of lymph nodes.
- Radiotherapy: After surgery, radiation therapy is used to reduce the chance of recurrence by focusing on the breasts and chest walls that are affected.
- Chemotherapy: The majority of individuals with stage 3 breast cancer receive chemotherapy. This can be given before surgery (neoadjuvant), or after surgery (adjuvant), to eliminate cancer cells and stop their spread.
- Hormone Treatment: When the cancer is hormone-receptor-positive, hormone therapy can be recommended.
- Targeted Treatment: Herceptin is a targeted therapy that may be used in cases where cancers overexpress the HER2 proteins.
- Immunotherapy: In certain cases, immunotherapy can be part of a treatment plan.
7. Prognosis: The prognosis of Stage 3 breast cancer depends on factors such as tumor size, lymph node involvement, and hormone receptor status. It also depends on the response to treatment. Although Stage 3 breast carcinoma is more advanced than earlier stages, treatment options are improving. Individual outcomes and survival rates can vary greatly.
Individuals diagnosed with stage 3 breast cancer must work closely with their healthcare provider to create a customized treatment plan. They should also engage in regular follow-up care to check for signs of metastasis or recurrence. Early detection, timely treatment, and comprehensive care are essential for effectively managing Stage 3 Breast Cancer.
Comparison table of Stage 2 and Stage 3 Breast Cancer
Here’s a comparison table highlighting the key differences between Stage 2 and Stage 3 breast cancer:
| Characteristic | Stage 2 Breast Cancer | Stage 3 Breast Cancer |
|---|---|---|
| Tumor Size | Generally smaller (2-5 cm) | Larger (varies, can be >5 cm) |
| Lymph Node Involvement | May involve nearby lymph nodes (Stage 2A) or may not (Stage 2B) | Often involves nearby lymph nodes, extensive in Stage 3C |
| Spread Beyond Breast | Tumor confined to the breast or involves nearby tissues | The tumor may invade the chest wall, skin, or lymphatic vessels |
| Distant Metastasis | No evidence of distant metastasis (M0) | No evidence of distant metastasis (M0) |
| Symptoms | May have breast lumps, skin changes, or nipple discharge | Symptoms more pronounced; potential skin ulceration |
| Diagnosis | Imaging tests, biopsy for confirmation | Imaging tests, biopsy for confirmation |
| Surgery | Lumpectomy or mastectomy | Mastectomy with extensive lymph node removal |
| Radiation Therapy | Common after surgery to target the breast or chest wall | Common after surgery to reduce recurrence risk |
| Chemotherapy | Administered to kill cancer cells, either before or after surgery | Administered to kill cancer cells, often before or after surgery |
| Hormone Therapy | Used if cancer is hormone receptor-positive | Used if cancer is hormone receptor-positive |
| Targeted Therapy | Administered if cancer overexpresses HER2 protein | Administered if cancer overexpresses HER2 protein |
| Immunotherapy | Not typically a standard treatment | Not typically a standard treatment |
| Prognosis | Generally more favorable compared to advanced stages | Prognosis varies, typically less favorable than Stage 2 |
| Five-Year Survival Rate | Relatively high varies by individual factors | Lower compared to Stage 2, varies by factors and substage |
Please be aware that individual factors, including tumor characteristics, hormone receptor status, and response to treatment can greatly vary the treatment plans and prognoses for Stage 2 and 3 breast cancer, making individual interaction between the healthcare team and those diagnosed essential.
It’s therefore critical for individuals diagnosed at either stage to work closely together on creating personalized plans tailored specifically for themselves with close monitoring from the healthcare team.
Importance of Early Detection and Screening
Screening and early detection of breast cancer is important for many reasons:
- Better Treatment Outcomes: Breast cancer detected at an earlier stage usually leads to a more successful outcome. Early stages of breast cancer (Stage 0, Stage 1 and in some cases, Stage 2) are more likely to be curable because the cancer is confined to one or two lymph nodes.
- Less aggressive Treatment: Early-stage breast cancer requires less aggressive treatments, such as smaller operations, less chemotherapy or shorter radiation sessions. It can lead to fewer side effects and an improved quality of life.
- Higher survival rates: Individuals diagnosed with breast cancer in the early stages of development have higher survival rates than those diagnosed later. Early detection increases the chance of long-term success.
- Preservation Breast Tissue: Early detection of breast cancer may allow lumpectomies to be performed instead of mastectomies, which remove the entire breast. This preserves a woman’s body image and breast tissue.
- Lower healthcare costs: Treating early-stage breast cancer is often cheaper than treating later-stage cancers, since it may require fewer interventions and shorter hospital stays.
- Less Psychological and Emotional Impact: Breast cancer can be emotionally and mentally challenging. Early detection of cancer may reduce the emotional distress that is associated with advanced stages.
- Cure Potential: Early detection of carcinoma in situ, which is limited to the milk ducts and lobules can result in a cure that has a high success rate.
- Screening High-Risk Individuals: Early and regular screening is important for individuals who have a family history or other risk factors. This can help detect cancer in its earliest stages when it’s most treatable.
- Risk reduction: Early screening can detect pre-cancerous lesions, allowing interventions to prevent invasive breast cancer.
- Impact on Public Health: Breast cancer screening programs are widely used in many countries and have led to a reduction in the mortality rate of breast cancer. This shows that early detection has a significant impact on public health.
Breast cancer screening methods include mammography and clinical breast exams performed by healthcare professionals. Individuals can also perform breast self-exams. Women should have regular screenings as they age. Mammograms are recommended at regular intervals.
Consult your healthcare provider for the best screening schedule, based on personal risk factors, family histories, and age. offers the best chance of successful treatment and better long-term outcomes.
Support and Resources
There are many resources and support available for individuals and families who are dealing with breast cancer. These resources and support can help them navigate the challenges of diagnosis, treatment, and recovery. Here are some of the most important sources of help and resources.
- Medical Team & Healthcare Providers:
- Breast cancer is a difficult disease to deal with. Your oncologist surgeon and other medical professionals can provide you with valuable information and support.
- Do not hesitate to discuss any concerns you may have with your healthcare team.
- Cancer Support Organizations:
- Many organizations, such as the American Cancer Society, Breast Cancer Now, Susan G. Komen, and others, provide educational materials and support services.
- You can often connect with other people facing similar issues through online communities, support groups, and helplines.
- Local Support Groups:
- Breast cancer support groups are available in many communities, either online or in person. These groups provide emotional support, sharing of information, and a feeling of community.
- Find out about local support groups by contacting your local hospital, cancer center, or community center.
- Mental Health Services and Counseling:
- It can be difficult to cope with breast cancer. Seek the help of a cancer-related therapist, social worker, or counselor.
- As part of their treatment, many cancer centers offer psychosocial support.
- Financial Assistance:
- Some organizations offer financial aid programs to help cover the costs of cancer treatment, medication, and other expenses.
- Consider programs offered by local cancer charities or organizations such as CancerCare.
- Online Resources:
- You can connect with other people and share your experiences on a number of reputable websites. Cancer.org and Breastcancer.org are examples.
- Patient Advocates and Navigators:
- Patient navigators and advocates are available at many hospitals and cancer centers to help you navigate the healthcare system. They can also provide resources and offer assistance with logistical issues.
- Clinical trials:
- Consider participating in clinical studies. They can give you access to the latest treatments and help with medical research. You can explore this option with your healthcare team.
- Education Materials:
- Many organizations provide booklets, brochures, and online materials covering various aspects of breast carcinoma, from treatment options to coping techniques.
- Peer Support:
- Connecting with someone else who has breast cancer can offer valuable insight and emotional support. Find programs that provide peer matching.
- Exercise Programs and Nutritional Programs:
- It is essential to maintain a healthy lifestyle during and after treatment for breast cancer. Some organizations provide nutrition and exercise programs for cancer patients.
- Complementary and Integrative therapies:
- These therapies can help complement conventional treatment and manage side effects.
- Employment and Legal Support:
- You can seek help from organizations that are experts in legal and workplace issues related to cancer if you have legal or workplace challenges relating to your breast cancer diagnosis.
You don’t need to face breast cancer alone. Explore the resources available to you and your healthcare team to get the information and support you need. There are many resources available to help you with your breast cancer journey.
conclusion
In the fight against cancer, early detection and resources and support are essential. Early detection of breast cancer and the use of available resources can help improve treatment outcomes and reduce emotional burden.
They can also enhance the quality of life during and after treatment. Breast cancer can be a difficult journey. However, with the right information and support, you can overcome it with more strength and resilience.
