A brief description of the respiratory system disorder of Interstitial Lung Disease and Bronchiectasis
The respiratory system controls the flow of carbon dioxide within the body. It is composed of several organs, such as the mouth, nose throat, trachea, lung bronchi, and lung. The respiratory system can be affected by various issues that can affect the operation of organs which can cause breathing problems and respiratory problems.
Here’s a quick review of the most commonly occurring respiratory problems:
Asthma: Asthma Chronic condition that is characterized by a narrowing and inflammation of the airways that result in repeated episodes of coughing, wheezing tightness in the chest, and breathlessness.
Chronic Obstructive Pulmonary Disorder (COPD): Chronic lung diseases include chronic bronchitis and Emphysema. It is due to long-term exposure to irritants, such as smoke from tobacco, resulting in breathing restrictions and airflow problems.
pneumonia: The infection creates inflammation in the lungs. It is usually caused by viruses, bacteria, or fungi. It can cause symptoms such as cough, fever chest pain, and breathing difficulties.
Chronic Bronchitis: A type of COPD that is characterized by chronic swelling and irritation to the bronchial tube, which can cause excessive production of mucus as well as coughing and difficulty breathing.
Emphysema: Another type of COPD in which the air sacs inside the lungs are damaged, which reduces their elasticity and affects gas exchange. It’s typically due to long-term exposure to irritating substances like smoke from cigarettes.
Lung cancer: An aggressive tumor that originates from the lungs, often due to exposure to carcinogens such as smoking cigarettes or environmental pollutants. It may cause symptoms like constant chest pain, cough loss of weight, and shortness of breath.
Sleep Apnea: A sleeping disorder that is characterized by pauses or shallow breathing in sleep, usually associated with loud snoring. It could lead to excessive sleepiness during the day and other health problems.
Pulmonary Fibrosis: A class of lung conditions characterized by the gradual scarring and stiffening of lung tissue. It affects the ability of the lungs to contract and expand and can cause breathing problems and a decrease in oxygen levels.
Cystic Fibrosis: Genetic disorder that impacts many organs, with a focus on the digestive system and lungs. It causes the production of sticky, thick mucus, which can lead to recurring lung infections as well as breathing issues.
Interstitial lung disease: An assortment of diseases that can cause irritation and scarring lung tissue, particularly the interstitium. It may be caused by a variety of sources, including occupational exposures, autoimmune disorders, and certain medicines.
These are only the most common respiratory system issues, and there are numerous other ailments that can affect the normal functioning of airways and lungs. A proper diagnosis, treatment, and treatment of these conditions are essential to maintain good health in the respiratory system and overall well-being.
Importance of understanding interstitial lung disease (ILD) and bronchiectasis
Understanding interstitial lung disease (ILD) and bronchiectasis is of significant importance for several reasons:
Accurate Diagnosis: ILD and bronchiectasis may share similar symptoms, including chronic coughing, shortness of breath, and frequent respiratory infections. However, their underlying causes, pathophysiology, and treatment approaches differ. Understanding the distinctive features of ILD and bronchiectasis allows healthcare professionals to make an accurate diagnosis and provide appropriate treatment.
Tailored Treatment: ILD and bronchiectasis require specific treatment strategies tailored to each condition. ILD often involves inflammation and scarring of the lung tissue, necessitating therapies such as immunosuppressants or antifibrotic medications. Bronchiectasis, on the other hand, focuses on managing airway clearance, controlling infections, and preventing exacerbations. A thorough understanding of these conditions ensures that patients receive targeted treatment to improve their outcomes.
Disease Progression and Prognosis: ILD and bronchiectasis have different courses of progression and prognoses. ILD can lead to progressive fibrosis and lung function decline, potentially necessitating lung transplantation in severe cases. Bronchiectasis, while chronic, may have a more stable or fluctuating course with periodic exacerbations. Understanding the natural history and prognosis of these diseases enables healthcare providers to educate patients about their condition and develop appropriate care plans.
Comorbidities and Complications: Both ILD and bronchiectasis are associated with various comorbidities and complications that can affect patient management. ILD may be linked with autoimmune conditions, pulmonary hypertension, or lung cancer while bronchiectasis has been associated with frequent infections, respiratory failure, and systemic diseases related to its presence. Identifying and managing these associated conditions is essential for comprehensive patient care.
Research and Advances: Research into ILD and bronchiectasis continues, leading to advances in diagnosis techniques, treatment options, and therapeutic interventions that benefit these conditions. Staying abreast of these developments enables healthcare professionals to deliver cutting-edge care while participating in clinical trials or research studies to advance the field.
Patient Education and Support: Understanding ILD and bronchiectasis helps patients and their caregivers comprehend the nature of their condition, manage symptoms, adhere to treatment plans, and recognize when to seek medical attention. Education and support play crucial roles in empowering patients to actively participate in their healthcare and improve their quality of life.
Having an in-depth knowledge of ILD and bronchiectasis helps healthcare providers accurately diagnose, treat, and manage these conditions – leading to improved patient outcomes, higher quality of life, and enhanced overall respiratory care.
Interstitial Lung Disease (ILD)
Interstitial Lung Disease (ILD) refers to a group of respiratory conditions characterized by inflammation and scarring (fibrosis) of the interstitium – tissue that supports air sacs called alveoli in our lungs – within it. ILD affects the lung’s ability to expand and contract properly, leading to breathing difficulties and impaired oxygen exchange.
Here are some key aspects of ILD:
Etiology and Risk Factors: ILD may result from various sources, including occupational and environmental exposures (asbestos, silica, or certain chemicals), autoimmune conditions like rheumatoid arthritis or systemic sclerosis, medication-induced lung injury due to anticoagulant treatments or predisposition genes and genetic predisposition, and finally cases with unknown causes ie Idiopathic causes (no known cause). Smoking and certain viral infections may also contribute to the development of ILD.
Pathophysiology: The exact mechanisms underlying ILD are not fully understood. Many times this condition results from an abnormal response of your immune system to injuries, which leads to chronic inflammation and the formation of fibrous tissue within the interstitium. Over time, this fibrosis can progressively worsen and impair lung function.
Clinical Presentation and Symptoms: The symptoms of ILD can vary depending on the specific type and stage of the disease. Common signs include a frequent dry cough, breath shortness (especially when you exert yourself) fatigue, tiredness, weight loss in the chest, and hands that are rounded (enlargement and rounded fingers). As ILD progresses, it can lead to respiratory failure and significant limitations in daily activities.
Diagnostic Methods and Tests: Diagnosing ILD requires a comprehensive evaluation, including medical history review, physical examination, lung function tests (such as spirometry and diffusion capacity), imaging studies (chest X-ray or high-resolution computed tomography – HRCT), and sometimes lung biopsies. These tests help identify the presence of interstitial abnormalities, assess lung function, and exclude other potential causes of lung disease.
Treatment Options and Management: The treatment approach for ILD depends on the underlying cause and the extent of fibrosis. In some cases, treating the underlying condition or removing the exposure to the causative agent can slow or halt disease progression. Corticosteroids are used as antifibrotic medicines as well as immunosuppressants and lung rehabilitation programs are prescribed to reduce symptoms, decrease inflammation and enhance lung function. Oxygen therapy and lung transplantation can be considered in severe cases.
Prognosis and Long-term Outcomes: The prognosis of ILD varies depending on the specific type and stage of the disease. Some forms of ILD have a more indolent course, while others can progress rapidly and lead to respiratory failure. A prompt diagnosis and proper treatment can stop the progression of fibrosis, and enhance the quality of life. However, in advanced stages, ILD may be irreversible, and lung transplantation may be the only option for survival.
It is important for individuals with ILD to work closely with healthcare professionals specializing in lung diseases to receive a proper diagnosis, develop a personalized treatment plan, and manage the symptoms effectively.

Regular follow-up visits, lifestyle modifications (such as smoking cessation), and support from patient advocacy groups can also be beneficial for individuals living with ILD.
Definition and basic characteristics
Interstitial Lung Disease (ILD) refers to a group of respiratory conditions characterized by inflammation and scarring (fibrosis) of the interstitium tissue which surrounds and supports alveoli in your lungs.
The interstitium, composed of connective tissue and tiny blood vessels, plays a significant role in exchanging carbon dioxide and oxygen between the bloodstream and alveoli.
It plays this role by providing support of exchange rates that allow oxygen-rich air into alveoli while carbon dioxide-rich air remains out.
Basic characteristics of ILD include:
Inflammation: ILD involves chronic inflammation within the interstitium of the lungs. Inflammation may result from various sources, including autoimmunity reactions or exposure to environmental agents; or as the result of diseases.
Fibrosis: Over time, the inflammation in ILD leads to the accumulation of fibrous tissue in the interstitium. This fibrosis causes scarring and stiffening of the lung tissue, impairing its ability to expand and contract effectively during breathing. The fibrosis can also disrupt the normal architecture of the lung, further compromising lung function.
Progressive Nature: ILD is typically a progressive condition, meaning that it tends to worsen over time. The fibrosis and scarring gradually increase, leading to a decline in lung function and respiratory symptoms. The rate of progression can vary depending on the specific type of ILD and individual factors.
Impaired Gas Exchange: The inflammation and fibrosis in ILD interfere with the normal exchange of oxygen and carbon dioxide in the lungs. The stiffened lung tissue reduces the surface area available for gas exchange, leading to reduced oxygen levels in the bloodstream and impaired removal of carbon dioxide.
Heterogeneity: ILD encompasses a broad range of diseases with diverse causes and clinical presentations. Interstitial Lung Disease, more commonly referred to as ILD covers over 200 unique forms. Common diagnoses of Interstitial Lung Disease include Idiopathic Pulmonary Fibrosis (IPF), Sarcoidosis, Hypersensitivity Pneumonitis Connective Tissue Disease-Associated ILD, and Drug-Induced ILD are among them. Each type of ILD has unique characteristics, risk factors, and treatment approaches.
Symptoms: Common symptoms of ILD include persistent dry cough, shortness of breath (especially with physical activity), fatigue, weight loss, chest discomfort, and clubbing of the fingers. The severity and progression of symptoms can vary depending on the specific type and stage of ILD.
It is important to note that ILD can have significant implications for a person’s overall health and quality of life. Early diagnosis, appropriate treatment, and ongoing management are essential to slow the progression of fibrosis, manage symptoms, and improve outcomes for individuals with ILD.
Bronchiectasis
Bronchiectasis is a long-lasting respiratory disorder that is characterized by an abnormal and persistent expansion (dilation) of bronchioles and bronchi, which are the bigger and less crowded airways within the lungs, according to.
The widening usually occurs due to an injury to the airway’s walls and can lead to loss of elasticity and reduced elimination of mucus and other bacteria out of the lung.
Here are the most important features of bronchiectasis:
The Etiology of the Disease and Risk Factors: Bronchiectasis is classified as acquired or congenital. Congenital bronchiectasis is uncommon and typically results from genetic disorders that alter the function and structure of the lungs. Acute bronchiectasis is more prevalent and could be brought on by multiple causes, including respiratory illnesses (like pneumonia ) COPD cystic fibrosis immune deficiencies as well as inhaling toxic substances that clog the airways.
Chronic Inflammation and Infection: Bronchiectasis can be a result of ongoing and persistent respiratory infections. The enlarged and damaged bronchi can become a breeding place for bacteria, which can lead to chronic inflammation. This inflammation could cause further damage to the airway wall and prolong the cycle of infections.
Signs and symptoms: Symptoms of bronchiectasis may differ for each person but generally include chronic cough with mucus production and frequent respiratory illnesses, breathlessness chest pain wheezing fatigue as well as rare instances of bleeding blood. The symptoms can become more severe during times of acute exacerbation. It is which is characterized by a rise in symptoms of cough and sputum creation and respiratory distress.
Diagnostic Procedures and Tests: A diagnosis for bronchiectasis usually involves an amalgamation of medical history assessment physical examinations along with diagnostic tests. Imaging studies like High-Resolution Computed Tomography (HRCT) scans give precise pictures of the lung. They also can detect the characteristic dilation of the bronchial tract. A sputum culture can be collected to detect any underlying infection. Lung function tests and bronchoscopy can also help evaluate lung performance and rule out other potential lung issues.
Therapy and Treatment: The treatment for bronchiectasis seeks to ease symptoms, avoid exacerbations and slow the progression of the disease. Treatment can include airway-clearing methods, like postural drainage, chest physiotherapy, and mechanical devices to aid in the removal of mucus from airways. Antibiotics can be prescribed to treat the underlying infection. Mucolytics and bronchodilators may help relieve symptoms while increasing airflow, thus decreasing discomfort and improving lung capacity. In extreme cases, or when conventional measures fail surgical removal of portions of the lung that are severely affected could be thought of.
Diagnosis and Long-term Results: The prognosis for bronchiectasis depends upon its root cause, severity of damage to lung tissue damage and effectiveness of treatment options available to address them. If properly managed, many sufferers of bronchiectasis live fairly normal lives. However, this condition can quickly escalate into complications such as respiratory failure and hemoptysis (coughing up blood). Furthermore, quality of life could significantly decline with time.
People suffering from bronchiectasis must work in partnership with health professionals specializing in respiratory illnesses to develop an individualized treatment plan designed to control symptoms and avoid complications.
Maintaining good health and overall wellness requires maintaining regular checkups and following prescribed treatments.
Definition and basic characteristics
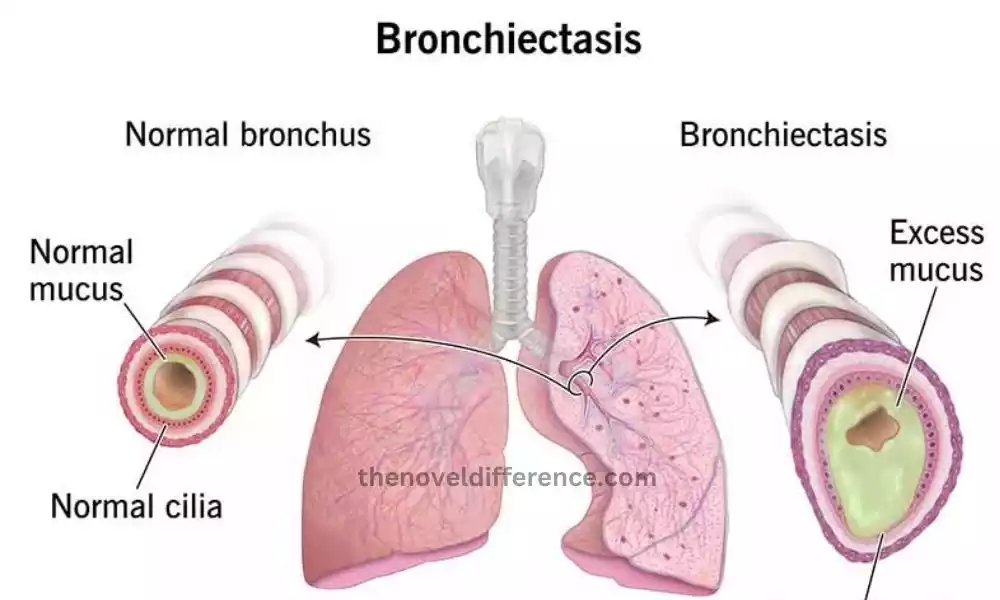
Bronchiectasis can be described as a chronic respiratory disease that manifests as persistent and unavoidable broadening (dilation) of bronchioles and bronchioles which are the bigger and smaller airways of the lung.
This dilation occurs due to damage to the walls of the airways, leading to a loss of elasticity and impaired clearance of mucus and bacteria from the lungs. This condition results in the accumulation of mucus and recurrent respiratory infections.
Here are some basic characteristics of bronchiectasis:
Acute Airway Injury: Bronchiectasis is typically caused due to damage to the airway wall. The damage may be due to infections, such as pneumonia or tuberculosis, or other underlying conditions that obstruct the airways. Genetic disorders like cystic fibrosis can also contribute to the development of bronchiectasis.
Mucus Accumulation: The damaged and widened bronchi in bronchiectasis do not effectively clear mucus and bacteria from the lungs. This leads to the accumulation of mucus, which provides a breeding ground for bacteria. Excessive mucus production is a hallmark of bronchiectasis.
Recurrent Infections: The impaired clearance of mucus and bacteria in bronchiectasis makes individuals more susceptible to recurrent respiratory infections. These infections can further damage the airways and exacerbate the condition. Common symptoms during infections include increased cough, sputum production, and worsening respiratory symptoms.
Chronic Symptoms: Bronchiectasis is characterized by chronic symptoms that persist over time. The symptoms can include a chronic cough or a rise in the quantity of sputum, shortness of breath, fatigue due to wheezing chest pain and, sometimes it is a case of coughing up blood. The severity of symptoms can vary among individuals.
Diagnostic Methods: The diagnosis of bronchiectasis typically involves a combination of medical history evaluation, physical examination, and diagnostic tests. HDCT (HRCT) scans are often employed to detect the dilation of the bronchial tubes and to determine the severity of the condition. Sputum cultures may be collected to identify any underlying infections, and lung function tests can assess lung function and airflow limitation.
Treatment Approaches: The management of bronchiectasis focuses on reducing symptoms, preventing complications, and managing underlying infections. Treatment can include airway-clearing techniques for removing mucus, medicines like antibiotics for treating ailments, bronchodilators for better airflow, and mucolytic agents to reduce mucus. In severe cases, surgery to remove damaged lung tissue may be considered.
Prognosis: The prognosis for bronchiectasis is different dependent on the root reason, the severity of the damage to lung tissue, as well as the efficacy of treatment. With proper management and adherence to treatment plans, individuals with bronchiectasis can lead relatively normal lives. This condition may slowly worsen and cause complications such as respiratory failure or diminished level of living.
Individuals living with bronchiectasis must collaborate closely with healthcare providers who specialize in respiratory diseases to create an individualized treatment plan, manage symptoms effectively, and avoid further complications.
Regular monitoring and adherence to prescribed therapies are crucial for maintaining lung health and overall well-being.
Difference between Interstitial Lung Disease and Bronchiectasis
In comparing interstitial lung diseases (ILD) as well as bronchiectasis many key differences can be seen in relation to the affected lung structures, their symptoms, diagnostic procedures treatments, as well as the long-term effects.
It’s also important to remember that these conditions may be co-existent in certain instances and people may show the same signs or risk factors.
Here is a comparison between ILD and bronchiectasis:
Affected Lung Structures:
ILD: In ILD, the interstitium, which is the tissue that surrounds and supports the air sacs (alveoli), is primarily affected. It involves inflammation and fibrosis within the interstitial spaces, leading to lung stiffness and reduced lung capacity.
Bronchiectasis: Bronchiectasis involves the dilation and damage of the bronchi and bronchioles, the larger and smaller airways in the lungs. The damage causes permanent widening and impaired clearance of mucus, leading to recurrent infections and chronic inflammation.
Clinical Presentation and Symptoms:
ILD: Common symptoms of ILD include persistent dry cough, shortness of breath (especially with exertion), fatigue, weight loss, chest discomfort, and clubbing of the fingers.
Bronchiectasis: The symptoms of bronchiectasis are typically chronic cough, which is characterized by the production of a large amount of mucus. It can also cause recurring respiratory infections, shortness of breath chest pain, wheezing, and fatigue.
Diagnostic Methods and Tests:
ILD: Diagnosis of ILD involves a combination of medical history evaluation, physical examination, lung function tests (spirometry, diffusion capacity), imaging studies (chest X-ray, high-resolution computed tomography – HRCT), and sometimes lung biopsies.
Bronchiectasis: Diagnostic methods for bronchiectasis may include medical history assessment, physical examination, chest X-ray, HRCT scan, sputum cultures to identify underlying infections and lung function tests.
Treatment Approaches:
ILD: Treatment for ILD depends on the specific type and underlying cause. It may involve immunosuppressants, antifibrotic medications, and supportive care measures such as oxygen therapy and pulmonary rehabilitation.
Bronchiectasis: Management of bronchiectasis focuses on airway clearance techniques (chest physiotherapy, postural drainage), antibiotics to treat infections, bronchodilators to improve airflow, and mucolytics to thin mucus. Surgery may be considered in severe cases.
Long-term Outcomes and Prognosis:
ILD: The prognosis for ILD will vary based on the type and severity of the illness. Certain types of ILD like Idiopathic Pulmonary Fibrosis (IPF) have an unfavorable prognosis. This is due to progressive fibrosis causing respiratory failure. Others may have a more indolent course.
Bronchiectasis: The long-term outcomes of bronchiectasis also vary depending on the underlying cause, severity, and management. If treated appropriately, many people can live relatively normal lives, however, problems such as respiratory failure or a decrease in quality of life can occur in more severe instances.
It is crucial to accurately differentiate between ILD and bronchiectasis as the treatment approaches and management strategies differ. Proper diagnosis by healthcare professionals specializing in respiratory diseases is essential for determining the appropriate treatment and improving patient outcomes.
What are the similarities Between Interstitial Lung Disease and Bronchiectasis?
While Interstitial Lung Disease (ILD) and bronchiectasis have distinct characteristics, there are some similarities between the two respiratory conditions.
These similarities include:
Chronic Respiratory Conditions: Both ILD and bronchiectasis are chronic lung disorders that involve long-term inflammation and damage to the lungs. They are not transient or acute conditions but rather ongoing and persistent.
Respiratory Symptoms: ILD and bronchiectasis can present with similar respiratory symptoms. Both conditions may cause chronic cough, shortness of breath, and fatigue. These symptoms can vary in severity and may worsen over time.
Risk Factors: There are certain risk factors that can contribute to the development of both ILD and bronchiectasis. Risk factors comprise a previous history of recurring respiratory infections and exposure to irritants from the environment, auto-immune diseases, and genetic predisposition. smoking. However, the specific risk factors may differ depending on the subtype or underlying cause of each condition.
Overlapping Comorbidities: Both ILD and bronchiectasis are associated with certain comorbidities. For instance, gastroesophageal illness (GERD) is an illness that may occur in patients suffering from both ILD and bronchiectasis. Other comorbidities may include pulmonary hypertension and lung cancer, although their prevalence can vary between ILD and bronchiectasis cases.
Diagnostic Challenges: Both ILD and bronchiectasis can be challenging to diagnose accurately. They could require a full examination, including a medical history assessments physical exam as well as lung function tests. Scans (such as chest X-rays or high-resolution computed tomography scans) and, sometimes, procedures that require invasive procedures, like lung biopsies. The diagnostic process for both conditions often involves ruling out other potential causes of lung disease.
Treatment and Management: While the specific treatment approaches may differ, both ILD and bronchiectasis require a comprehensive management plan. Treatment goals of CFS aim to control symptoms, slow disease progression, manage any associated infections and enhance the quality of life. Management strategies may include medications, airway clearance techniques, pulmonary rehabilitation, and lifestyle modifications.
Impact on Quality of Life: Both ILD and bronchiectasis can significantly impact an individual’s quality of life. The chronic nature of these illnesses and the associated symptoms like breathlessness and fatigue can result in a decrease in activities that are routine, and a decline in general health.
It’s important to note that despite these similarities, ILD and bronchiectasis are distinct entities with different underlying mechanisms, affected lung structures, diagnostic approaches, and treatment options.
Therefore, accurate diagnosis by healthcare professionals specializing in respiratory diseases is essential for providing appropriate care and optimizing patient outcomes.
Interstitial Lung Disease vs Bronchiectasis in Tabular Form
Certainly! Here’s a tabular comparison between Interstitial Lung Disease (ILD) and Bronchiectasis:
| aspect | Interstitial Lung Disease (ILD) | Bronchiectasis |
|---|---|---|
| Definition | A chronic respiratory disorder characterized by | A chronic respiratory condition characterized by |
| inflammation and scarring of the interstitium | abnormal and permanent widening of the bronchi | |
| Affected Lung Structures | Interstitium (tissue supporting the air sacs) | Bronchi and bronchioles (airways) |
| Etiology | Various causes: occupational exposures, | Various causes: recurrent infections, chronic |
| autoimmune diseases, medications, genetic | obstructive pulmonary disease (COPD), cystic | |
| predisposition, idiopathic (unknown cause) | fibrosis, immune deficiencies, underlying | |
| conditions obstructing airways, genetic disorders | ||
| Clinical Presentation | Persistent dry cough, shortness of breath, | Chronic cough with the production of large amounts |
| and Symptoms | fatigue, weight loss, chest discomfort, | of mucus, recurrent respiratory infections, |
| clubbing of fingers | shortness of breath, wheezing, chest pain, fatigue | |
| Diagnostic Methods | Medical history, physical examination, lung | Medical history, physical examination, chest |
| and Tests | function tests (spirometry, diffusion capacity), | X-ray, high-resolution computed tomography (HRCT) |
| imaging studies (chest X-ray, HRCT), lung | scan, sputum cultures, lung function tests | |
| biopsies | ||
| Treatment | Specific to underlying cause: immunosuppressants, | Airway clearance techniques (chest physiotherapy, |
| antifibrotic medications, supportive care | postural drainage), antibiotics, bronchodilators, | |
| mucolytics, surgery (in severe cases) | ||
| Prognosis | Varies depending on the type and stage of disease | Varies depending on the underlying cause, severity, |
| Some forms have poor prognoses, which may lead to | and management, with appropriate treatment | |
| respiratory failure | outcomes can be relatively normal | |
| Impact on Quality of | Significant impact on quality of life, | Significant impact on quality of life, potential |
| Life | limitations in daily activities | for limitations in daily activities |
Please note that this table provides a general overview, and there may be variations and overlaps between individual cases. It’s always best to consult healthcare professionals for accurate diagnosis, treatment, and management of specific cases of ILD or bronchiectasis.
Conclusion
Interstitial Lung Disease (ILD) and Bronchiectasis are distinct respiratory conditions with unique characteristics. ILD typically affects the interstitium, leading to inflammation and fibrosis; while bronchiectasis involves dilation and damage of bronchi and bronchioles.
They are caused by different causes such as clinical presentation, treatments, diagnostic techniques, and long-term results.
Understanding the differences between ILD and bronchiectasis is crucial for accurate diagnosis, appropriate treatment, and effective management.
