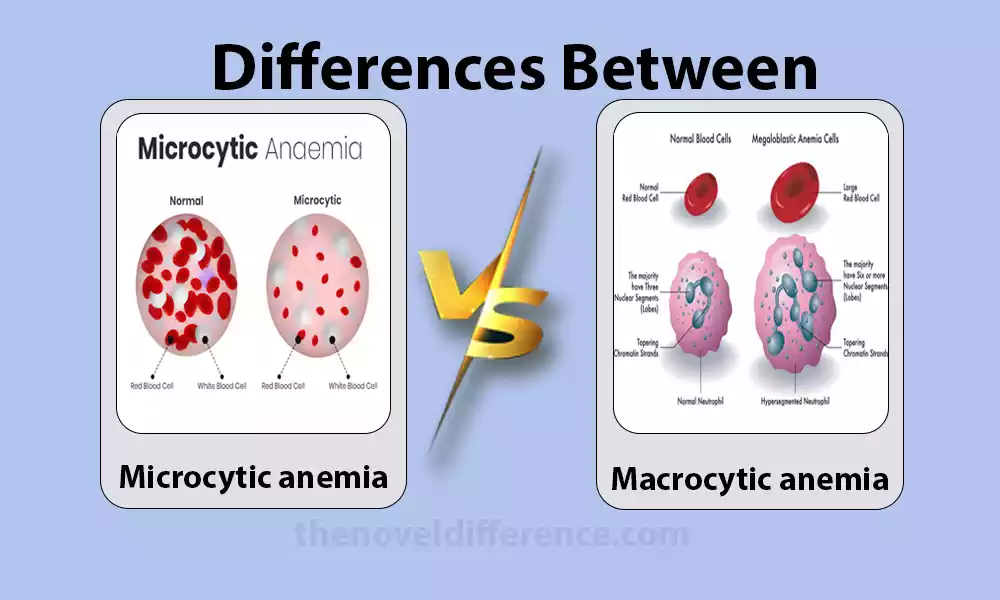
Microcytic anemia and macrocytic anemia. In spite of the fact that they both drop beneath the umbrella of frailty, these conditions vary essentially in terms of causes, indications, and treatment approaches. Understanding the refinement between microcytic and macrocytic iron deficiency is pivotal for exact determination and viable administration. Let’s delve deeper into the characteristics, causes, and treatment options for each type.
Definition of Microcytic and Macrocytic Anemia
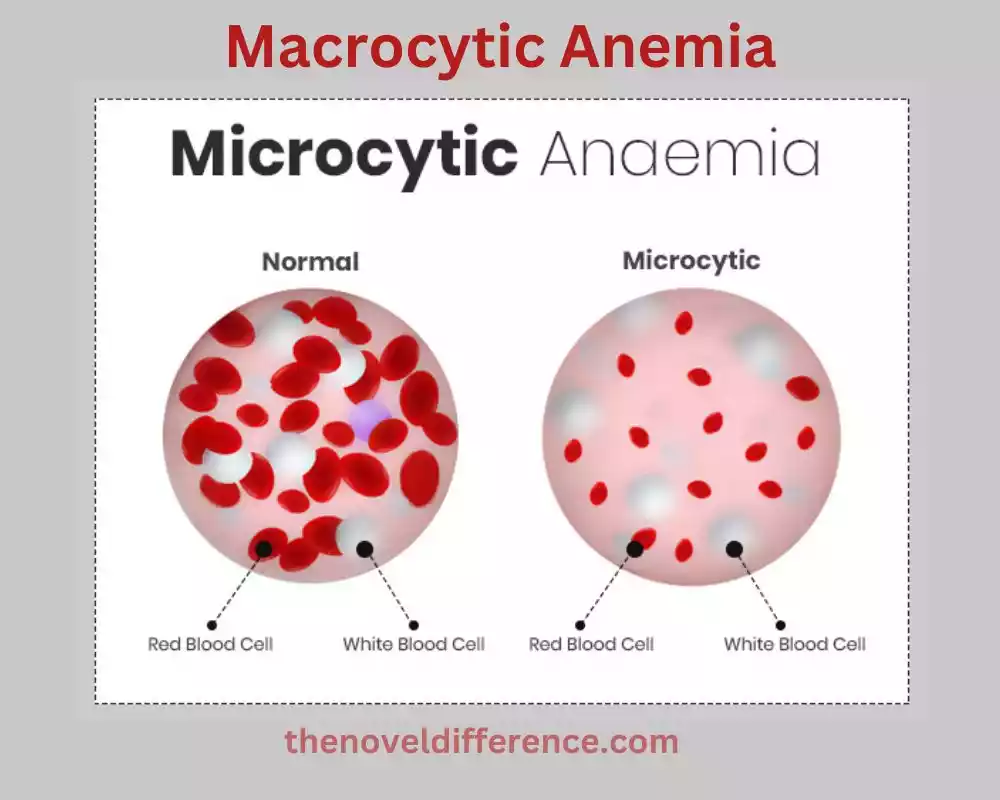
Microcytic Anemia: Microcytic Anemia is a Type of Anemia Characterized by Abnormally Small Red Blood Cells (RBCs). It is typically defined by a decreased mean corpuscular volume (MCV), which reflects the average size of the RBCs. In microcytic anemia, the MCV is usually less than 80 femtoliters (fL). The reduced size of the RBCs can result from various underlying conditions, including iron deficiency anemia, thalassemia, anemia of chronic disease, and sideroblastic anemia. Microcytic Anemia is Often Associated With a Decreased Hemoglobin Content Within the RBCs, Leading to a Condition Known as Hypochromia.
Macrocytic Anemia: Macrocytic Anemia is a Type of Anemia Characterized by Abnormally Large Red Blood Cells (RBCs). It is defined by an increased mean corpuscular volume (MCV), which reflects the average size of the RBCs. In macrocytic anemia, the MCV is usually greater than 100 femtoliters (fL). The Larger Size of the RBCs Can Be Attributed to Various Underlying Causes, Including Vitamin B12 Deficiency, Folate Deficiency, Alcoholism, and Certain Medications. The RBCs may also exhibit abnormal cellular maturation, known as megaloblastic changes, which can be observed in the bone marrow.
Classification of anemia based on red blood cell (RBC) size
Anemia Can Be Classified Based on the Size of Red Blood Cells (RBCs) Into Three Main Categories.
Microcytic Anemia, Normocytic Anemia, and Macrocytic Anemia:
1. Microcytic Anemia:
• Definition: Microcytic anemia is characterized by abnormally small RBCs.
• Key feature: Decreased mean corpuscular volume (MCV), usually less than 80 femtoliters (fL).
• Common causes: Iron deficiency anemia, thalassemia, anemia of chronic disease, sideroblastic anemia.
• Pathophysiology: Reduced hemoglobin synthesis or abnormal hemoglobin structure leading to smaller RBCs.
• Diagnostic features: Hypochromic RBCs (pale appearance) and decreased MCV.
2. Normocytic Anemia:
• Definition: Normocytic anemia is characterized by RBCs that are within the normal size range.
• Key feature: Normal mean corpuscular volume (MCV), typically ranging from 80 to 100 femtoliters (fL).
• Common causes: Acute blood loss, chronic diseases, kidney disease, bone marrow disorders, and some nutritional deficiencies.
• Pathophysiology: Various mechanisms can lead to normocytic anemia, such as decreased production, increased destruction, or blood loss.
• Diagnostic features: RBCs appear relatively normal in size and color, with a normal MCV.
3. Macrocytic Anemia:
• Definition: Macrocytic anemia is characterized by abnormally large RBCs.
• Key feature: Increased mean corpuscular volume (MCV), usually greater than 100 femtoliters (fL).
• Common causes: Vitamin B12 deficiency, folate deficiency, alcoholism, certain medications.
• Pathophysiology: Impaired DNA synthesis affects RBC maturation, leading to larger and immature RBCs.
• Diagnostic features: Megaloblastic changes in the bone marrow, larger RBCs, and increased MCV.
It’s critical to note that these categories are not commonly elite, and there can be covered or blended highlights in a few cases of anemia. Proper diagnosis and identification of the underlying cause are crucial for effective management and treatment.
What is Microcytic Anemia?
Microcytic Anemia is a Type of Anemia Characterized by Abnormally Small Red Blood Cells (RBCs). It is typically defined by a decreased mean corpuscular volume (MCV), which reflects the average size of the RBCs. In microcytic anemia, the MCV is usually less than 80 femtoliters (fL).
Microcytic Anemia Can Be Caused by Various Underlying Conditions, With the Most Common Being Iron Deficiency Anemia. Iron deficiency leads to insufficient production of hemoglobin, the oxygen-carrying protein within RBCs. As a result, the RBCs are smaller and have a reduced hemoglobin content. Other causes of microcytic anemia include thalassemia (inherited blood disorders affecting hemoglobin production), anemia of chronic disease (associated with chronic infections, inflammatory conditions, or malignancies), and sideroblastic anemia (impaired iron utilization in RBC production).
The smaller size of the RBCs in microcytic anemia can be observed under a microscope. They are often described as hypochromic, meaning they have a paler appearance due to decreased hemoglobin content. Microcytic Anemia Can Result in Reduced Oxygen-Carrying Capacity, Leading to Symptoms Such as Fatigue, Weakness, Pale Skin, Shortness of Breath, and Rapid Heart Rate.
Diagnosis of microcytic anemia involves assessing the MCV and other blood tests, including iron studies (serum iron, ferritin, transferrin), total iron-binding capacity (TIBC), and transferrin saturation. These tests help determine the underlying cause of the microcytic anemia.
Treatment of microcytic anemia focuses on addressing the underlying cause. In cases of iron deficiency anemia, iron supplementation is usually prescribed to replenish iron stores. Treatment approaches for other causes may involve managing the associated conditions or employing specific therapies based on the underlying disorder. It is essential to identify and treat microcytic anemia to alleviate symptoms and improve overall health and well-being.
Causes and underlying conditions
Microcytic anemia can be caused by various underlying conditions. The most common causes include:
1. Iron deficiency anemia: This is the most frequent cause of microcytic anemia. It happens when the body doesn’t have a sufficient press to deliver satisfactory sums of hemoglobin. Iron deficiency can be caused by deficient dietary admissions, destitute press assimilation, blood misfortune (e.g., from overwhelming menstrual periods or gastrointestinal dying), or expanded press prerequisites (e.g., amid pregnancy).
2. Thalassemia: Thalassemia is a group of inherited blood disorders that affect the production of hemoglobin. It leads to reduced synthesis of one or more globin chains of hemoglobin, resulting in small and fragile RBCs. There are different sorts and seriousness levels of thalassemia, counting alpha thalassemia and beta thalassemia.
3. Anemia of chronic disease (ACD): ACD is a type of anemia that occurs in the setting of chronic inflammatory diseases, such as infections, autoimmune disorders, or malignancies. In ACD, the body’s ability to use iron for red blood cell production is impaired, leading to decreased production of normal-sized RBCs and subsequent microcytic anemia.
4. Sideroblastic anemia: Sideroblastic anemia is a rare type of anemia characterized by impaired iron utilization in the bone marrow. It can be inherited (congenital) or acquired. In this condition, RBCs are small and contain abnormal iron deposits called sideroblasts. Sideroblastic anemia can be caused by genetic mutations, certain medications, alcohol abuse, or underlying conditions such as myelodysplastic syndromes.
Other less common causes of microcytic anemia include:
• Lead poisoning: Exposure to high levels of lead can interfere with heme synthesis and result in microcytic anemia.
• Some chronic kidney diseases: Certain kidney disorders can lead to inadequate production of erythropoietin, a hormone necessary for red blood cell production, causing microcytic anemia.
• Other rare genetic disorders: Conditions like congenital dyserythropoietic anemia, pyridoxine-refractory anemia, or Pearson syndrome can also cause microcytic anemia.
It’s Important to Note That the Specific Cause of Microcytic Anemia Can Vary Depending on the Individual and Their Medical History. Proper diagnosis and identification of the underlying cause are crucial for appropriate treatment and management.
Iron deficiency anemia
Iron Deficiency Anemia is a Type of Microcytic Anemia That Occurs When the Body Lacks Sufficient Iron to Produce an Adequate Amount of Hemoglobin. Hemoglobin is the Protein in Ruddy Blood Cells That Carries Oxygen From the Lungs to the Tissues All Through the Body. The press is a fundamental component of hemoglobin, and without a sufficient press, the body cannot create sufficient sound ruddy blood cells.
Causes of Iron Deficiency Anemia:
1. Inadequate iron intake: A diet lacking in iron-rich foods can lead to insufficient iron levels in the body, especially in individuals with poor dietary choices or restricted diets.
2. Blood loss: Chronic or acute blood loss can deplete the body’s iron stores. Common causes of blood loss include heavy menstrual periods, gastrointestinal bleeding (such as from ulcers, polyps, or colon cancer), frequent blood donation, or injury/trauma.
3. Poor iron absorption: Certain conditions can interfere with the absorption of iron from the diet. Illustrations incorporate celiac infection, incendiary bowel illness, gastric bypass surgery, and conditions influencing the stomach or little digestive system.
4. Increased iron requirements: Some life stages or situations require higher iron intake. These include pregnancy, rapid growth in adolescence, and breastfeeding. If iron intake does not match the increased requirements, iron deficiency anemia may occur.
Signs and Symptoms:
The signs and symptoms of iron deficiency anemia can vary in severity but may include:
• Fatigue and weakness
• Pale skin and mucous membranes
• Shortness of breath and rapid heartbeat
• Headaches and dizziness
• Brittle nails and hair loss
• Restless legs syndrome (a strong urge to move the legs)
• Pica (craving and eating non-food substances like ice, dirt, or clay)
Diagnosis and Treatment: Determination of press insufficiency iron deficiency includes a physical examination, restorative history audit, blood tests to degree hemoglobin levels, hematocrit, serum press levels, ferritin levels, and add up to iron-binding capacity (TIBC). These tests help determine the iron status and the underlying cause of the anemia.
Treatment for iron deficiency anemia typically involves iron supplementation through oral iron supplements. In severe cases or when oral supplements are not well-tolerated or ineffective, intravenous iron therapy may be necessary. Addressing the underlying cause, such as treating gastrointestinal bleeding or adjusting dietary habits, is also important to prevent a recurrence.
Anticipation of press lack frailty includes devouring an adjusted count of calories wealthy in press sources such as incline meats, poultry, angle, vegetables, verdant greens, and braced cereals. Press assimilation can be improved by expending vitamin C-rich nourishments alongside iron-rich nourishments.
Regular monitoring and follow-up with healthcare providers are important to assess the response to treatment and ensure optimal iron levels are maintained.
Thalassemia
Thalassemia alludes to a bunch of acquired blood disarranges characterized by anomalous hemoglobin generation. Hemoglobin is the protein inside ruddy blood cells (RBCs) that carries oxygen all through the body. Thalassemia results from genetic mutations that affect the production of one or more of the globin chains that make up hemoglobin.
There are two main types of thalassemia: alpha thalassemia and beta thalassemia. The severity and symptoms of thalassemia vary depending on the number of affected globin chains and the specific genetic mutations involved.
1. Alpha Thalassemia:
• Alpha thalassemia occurs when there are defects in the genes responsible for alpha globin production.
• The severity of alpha thalassemia depends on the number of affected gene copies.
• Silent carrier: One gene copy is affected, usually causing no symptoms.
• Alpha thalassemia trait: Two gene copies are affected, resulting in mild anemia.
• Hemoglobin H disease: Three gene copies are affected, leading to moderate to severe anemia and possible complications.
• Hemoglobin Bart syndrome: All four gene copies are affected, resulting in a severe and life-threatening condition in newborns.
2. Beta Thalassemia:
• Beta thalassemia occurs when there are defects in the genes responsible for beta-globin production.
• The severity of beta thalassemia also depends on the specific genetic mutations involved.
• Thalassemia minor or beta thalassemia trait: One gene copy is affected, causing mild anemia.
• Thalassemia intermedia: Two gene copies are affected, resulting in moderate to severe anemia.
• Thalassemia major or Cooley’s anemia: Both gene copies are affected, leading to severe anemia requiring lifelong treatment and blood transfusions.
Common features and complications of thalassemia include:
• Chronic anemia: Thalassemia leads to a reduced lifespan of red blood cells, resulting in chronic anemia.
• Fatigue, weakness, and pale skin.
• Enlarged spleen and liver.
• Bone deformities and growth abnormalities (in severe cases).
• Iron overload: Repeated blood transfusions can lead to excess iron accumulation in the body, requiring iron chelation therapy.
• Increased infection risk: Thalassemia can weaken the immune system, making individuals more susceptible to infections.
Diagnosis of Thalassemia Involves a Combination of Blood Tests, Including a Complete Blood Count (CBC), Hemoglobin Electrophoresis, and Genetic Testing. Prenatal testing is available to diagnose thalassemia in the fetus during pregnancy.
Treatment for Thalassemia Aims to Manage Symptoms, Prevent Complications, and Improve Quality of Life. Treatments May Include Regular Blood Transfusions, Iron Chelation Therapy, Folic Acid Supplementation, And, in Severe Cases, Bone Marrow transplantation. Genetic Counseling is Crucial for Individuals With Thalassemia or Those With a Family History of the Condition to Understand the Inheritance Pattern and Make Informed Decisions Regarding Family Planning.
What is Macrocytic Anemia?
Macrocytic anemia is a type of anemia characterized by the presence of abnormally large red blood cells (RBCs). It is defined by an increased mean corpuscular volume (MCV), which reflects the average size of the RBCs. In macrocytic anemia, the MCV is usually greater than 100 femtoliters (fL).
Macrocytic anemia can occur due to various underlying causes, most commonly related to deficiencies in vitamin B12 or folate. These two nutrients play essential roles in DNA synthesis and red blood cell production. When there is a deficiency of vitamin B12 or folate, the process of RBC maturation is impaired, resulting in larger and immature RBCs.
Causes of Macrocytic Anemia:
1. Vitamin B12 deficiency: This can occur due to inadequate dietary intake of vitamin B12 (found in animal products), malabsorption (e.g., pernicious anemia, gastrointestinal disorders), or impaired utilization of vitamin B12 by the body. Pernicious anemia is an autoimmune condition where the body cannot produce intrinsic factors, a protein required for vitamin B12 absorption.
2. Folate deficiency: Inadequate dietary intake of folate (found in leafy greens, legumes, and fortified cereals), malabsorption, increased requirements (e.g., pregnancy), or certain medications (such as methotrexate) can lead to folate deficiency.
Other less common causes of macrocytic anemia include:
• Alcoholism: Chronic alcohol consumption can interfere with folate absorption and utilization, leading to macrocytic anemia.
• Medications: Some medications, such as certain anticonvulsants or chemotherapy drugs, can cause macrocytic anemia as a side effect.
• Bone marrow disorders: Certain bone marrow disorders, such as myelodysplastic syndromes or leukemia, can result in macrocytic anemia.
Signs and Symptoms: The signs and symptoms of macrocytic anemia are similar to those of other types of anemia and may include:
• Fatigue and weakness
• Shortness of breath and rapid heartbeat
• Pale skin and mucous membranes
• Dizziness and lightheadedness
• Glossitis (inflammation of the tongue)
• Numbness or tingling in the extremities (due to nerve damage in vitamin B12 deficiency)
Diagnosis and Treatment: Diagnosis of Macrocytic Anemia Involves a Physical Examination, Medical History Review, Blood Tests (Including Complete Blood Count, MCV, Vitamin B12 Levels, and Folate Levels), and Sometimes Additional Tests to Identify the Underlying Cause.
Treatment for macrocytic anemia primarily focuses on addressing the underlying cause:
• Vitamin B12 deficiency: Vitamin B12 supplementation, either through oral or injectable forms, is used to correct the deficiency. In pernicious anemia or cases of malabsorption, lifelong supplementation may be necessary.
• Folate deficiency: Folate supplementation, either through diet or supplements, is prescribed to replenish folate levels.
It’s important to identify and treat macrocytic anemia to alleviate symptoms, improve red blood cell production, and prevent complications associated with vitamin deficiencies. Regular follow-up with healthcare providers is essential to monitor response to treatment and ensure optimal outcomes.
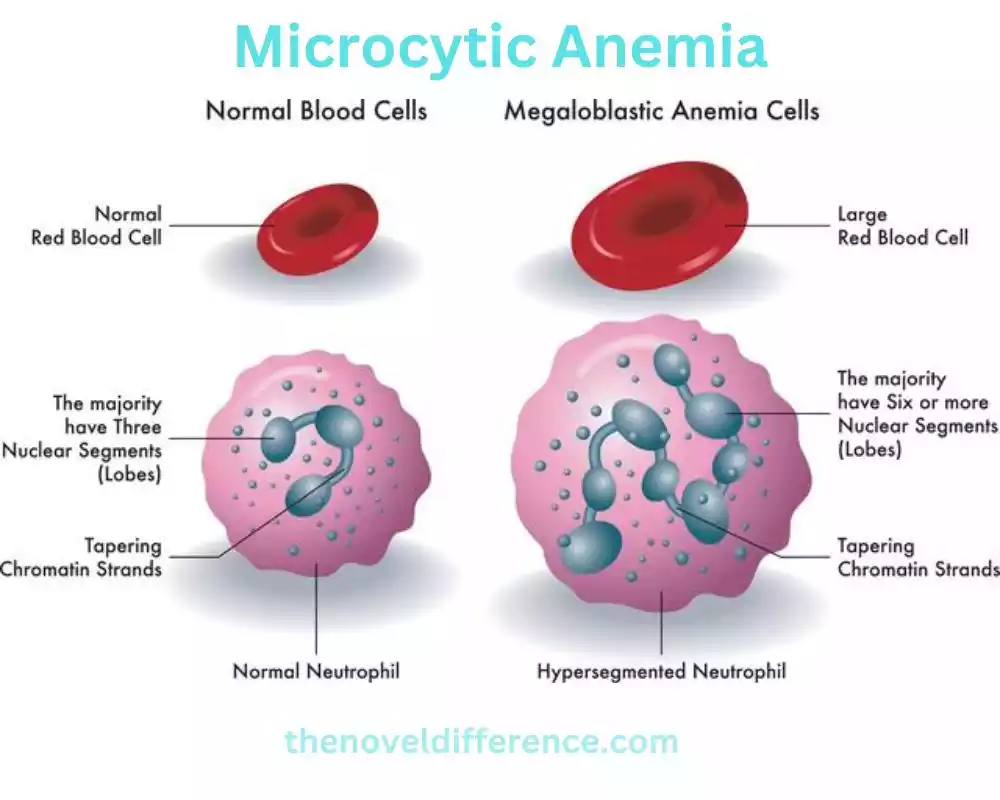
Pathophysiology and RBC characteristics
Pathophysiology of Macrocytic Anemia: Macrocytic anemia occurs when there is a disruption in the normal process of red blood cell (RBC) production and maturation. The underlying causes, such as vitamin B12 or folate deficiencies, affect DNA synthesis and impair the maturation of RBCs in the bone marrow.
1. Vitamin B12 Deficiency: Impaired absorption or utilization of vitamin B12 leads to reduced availability of this essential nutrient. Vitamin B12 is necessary for the normal function of folate metabolism and DNA synthesis in RBC precursors. Without sufficient vitamin B12, cell division and maturation in the bone marrow are hindered, resulting in large and immature RBCs.
2. Folate Deficiency: Folate is essential for DNA synthesis, including the synthesis of thymidine, a component of DNA. In folate deficiency, there is a lack of folate available for RBC precursors. This deficiency impairs DNA synthesis, leading to impaired cell division and maturation. As a result, larger RBCs are produced.
RBC Characteristics in Macrocytic Anemia: The hallmark characteristic of macrocytic anemia is the presence of larger-than-normal red blood cells. These enlarged RBCs, also known as macrocytes, can be observed under a microscope. The increased size is reflected in the mean corpuscular volume (MCV) measurement, which is typically elevated in macrocytic anemia (greater than 100 fL).
Additional RBC characteristics in macrocytic anemia include:
1. Ovalocytes: Macrocytic anemia may also be associated with the presence of ovalocytes, which are oval-shaped RBCs. Ovalocytes can occur in various types of macrocytic anemias, including those caused by vitamin B12 or folate deficiencies.
2. Hypersegmented Neutrophils: Macrocytic anemia, particularly due to vitamin B12 deficiency, can lead to hypersegmented neutrophils. Neutrophils are a type of white blood cell involved in immune responses. In vitamin B12 deficiency, neutrophils may exhibit an increased number of lobes in their nucleus, known as hypersegmentation.
3. Anisocytosis: Anisocytosis refers to an abnormal variation in RBC size. In macrocytic anemia, anisocytosis may be present, with a mixture of macrocytes and normocytes (normal-sized RBCs) observed in the blood smear.
It’s important to note that the specific characteristics and morphological changes in RBCs can vary depending on the underlying cause of macrocytic anemia. Close examination of blood smears and additional laboratory tests can help in identifying the specific etiology and guiding appropriate treatment.
Increased mean corpuscular volume (MCV)
An increased mean corpuscular volume (MCV) is a hematological parameter that indicates the average size of red blood cells (RBCs) in a blood sample. The MCV is reported in femtoliters (fL). An elevated MCV value is typically associated with macrocytic anemia, where the RBCs are larger than normal.
The MCV is calculated by dividing the hematocrit (the volume of RBCs in a given blood sample) by the RBC count and multiplying it by 10. It provides valuable information about the size of RBCs and helps in the classification of anemia.
Causes of Increased MCV:
1. Vitamin B12 Deficiency: Vitamin B12 deficiency is a common cause of macrocytic anemia. In this condition, the impaired DNA synthesis and maturation of RBCs result in larger-sized cells. The MCV is typically increased in vitamin B12 deficiency anemia.
2. Folate Deficiency: Folate (vitamin B9) deficiency is another cause of macrocytic anemia. Similar to vitamin B12 deficiency, folate deficiency affects DNA synthesis and leads to larger RBCs, resulting in an increased MCV.
3. Alcoholism: Chronic alcohol abuse can contribute to macrocytic anemia. The exact mechanism is not fully understood, but it is thought to be related to the direct toxic effects of alcohol on bone marrow and RBC precursors. Alcohol-related macrocytic anemia is characterized by an elevated MCV.
4. Liver Disease: Certain liver diseases, such as cirrhosis, can be associated with macrocytic anemia and an increased MCV. Liver dysfunction affects the metabolism and utilization of folate and vitamin B12, leading to impaired RBC production and larger RBCs.
5. Myelodysplastic Syndromes: Myelodysplastic syndromes are a group of disorders characterized by abnormal bone marrow function. In these conditions, ineffective hematopoiesis (formation of blood cells) can result in macrocytic anemia and an increased MCV.
6. Medications: Some medications, such as certain chemotherapy drugs and antiretroviral medications, can cause macrocytic anemia and an elevated MCV as a side effect.
It’s important to note that an elevated MCV is not exclusive to macrocytic anemia, and other factors, such as reticulocytosis (an increased number of immature RBCs) or certain medications, can also influence the MCV. Therefore, a thorough evaluation, including additional laboratory tests and clinical assessment, is necessary to determine the underlying cause of an increased MCV and guide appropriate diagnosis and treatment.
Megaloblastic RBCs
Megaloblastic red blood cells (RBCs) are abnormally large and immature RBCs that are commonly observed in certain types of anemia, specifically megaloblastic anemias. Megaloblastic anemias are characterized by impaired DNA synthesis, resulting in delayed maturation of RBC precursors in the bone marrow.
The main causes of megaloblastic anemia are deficiencies in vitamin B12 (cobalamin) or folate (vitamin B9), both of which are essential for normal DNA synthesis and cell division. When there is a deficiency of these vitamins, RBC precursors undergo abnormal and asynchronous maturation, leading to the production of megaloblastic RBCs.
Characteristics of Megaloblastic RBCs:
1. Increased Size: Megaloblastic RBCs are larger than normal RBCs. They have an increased mean corpuscular volume (MCV), which reflects the average size of RBCs. The elevated MCV indicates macrocytosis, where the RBCs are larger than the typical size.
2. Oval Shape: Megaloblastic RBCs often have an oval or elongated shape, which is a characteristic feature. This is in contrast to the normal biconcave disk shape of mature RBCs.
3. Nuclear Changes: One of the distinguishing features of megaloblastic RBCs is the presence of nuclear abnormalities. The nucleus of the RBC precursor remains large and immature, with delayed maturation. These abnormal nuclei are often described as having a “giant” or “bulging” appearance.
4. Cytoplasmic Changes: The cytoplasm of megaloblastic RBCs is usually basophilic or bluish in color. It may contain remnants of RNA, reflecting the delayed nuclear maturation.
The presence of megaloblastic RBCs, along with an elevated MCV, is a key indicator of megaloblastic anemia. It’s important to note that megaloblastic changes can also be observed in other conditions, such as certain medications or rare inherited disorders.
Identifying megaloblastic RBCs through peripheral blood smear examination helps in the diagnosis and differentiation of megaloblastic anemias from other types of anemias. It is crucial to determine the underlying cause of megaloblastic anemia, as treatment involves addressing the specific vitamin deficiency (vitamin B12 or folate) through supplementation or dietary modifications.
Difference between Microcytic and Macrocytic Anemia
Microcytic Anemia:
1. Definition: Microcytic anemia is characterized by the presence of abnormally small red blood cells (RBCs), typically with a decreased mean corpuscular volume (MCV). The MCV value is usually less than 80 femtoliters (fL).
2. Causes: Microcytic anemia is commonly caused by conditions that result in impaired hemoglobin synthesis or iron metabolism disorders. The primary causes include iron deficiency anemia, thalassemia, and anemia of chronic disease.
3. RBC Characteristics: The RBCs are smaller than normal. They have a reduced size and volume compared to healthy RBCs. The cells may appear hypochromic (paler in color) due to decreased hemoglobin content.
4. Symptoms: Symptoms of microcytic anemia include fatigue, weakness, pale skin, shortness of breath, and cold intolerance. Other symptoms may be present depending on the underlying cause.
5. Diagnostic Tests: Diagnosis involves a complete blood count (CBC), peripheral blood smear examination, and additional tests to determine the underlying cause, such as iron studies and hemoglobin electrophoresis.
6. Treatment: Treatment of microcytic anemia focuses on addressing the underlying cause. This may include iron supplementation, dietary changes, blood transfusions (in severe cases), or management of the underlying disease.
Macrocytic Anemia:
1. Definition: Macrocytic anemia is characterized by the presence of abnormally large red blood cells (RBCs), typically with an increased mean corpuscular volume (MCV). The MCV value is usually greater than 100 femtoliters (fL).
2. Causes: Macrocytic anemia is commonly caused by deficiencies in vitamin B12 or folate. Other causes include alcoholism, liver disease, certain medications, and bone marrow disorders.
3. RBC Characteristics: The RBCs are larger than normal. They have an increased size and volume compared to healthy RBCs. The cells may be oval-shaped or show other abnormal morphological features.
4. Symptoms: Symptoms of macrocytic anemia are similar to other types of anemia and may include fatigue, weakness, shortness of breath, pale skin, and other symptoms associated with the underlying cause.
5. Diagnostic Tests: Diagnosis involves a complete blood count (CBC), peripheral blood smear examination, measurement of vitamin B12 and folate levels, and other tests to determine the underlying cause.
6. Treatment: Treatment of macrocytic anemia focuses on addressing the underlying cause. This may include vitamin B12 or folate supplementation, dietary changes, management of underlying diseases, or discontinuation of causative medications.
The main difference between microcytic and macrocytic anemia lies in the size of the red blood cells. Microcytic anemia is characterized by small RBCs, while macrocytic anemia is characterized by large RBCs. The underlying causes, symptoms, diagnostic tests, and treatment approaches also differ between the two types of anemia.
Comparison Chart
Sure! Here’s a comparison chart highlighting the key differences between microcytic and macrocytic anemia:
| Category | Microcytic Anemia | Macrocytic Anemia |
|---|---|---|
| RBC Size | Abnormally small RBCs | Abnormally large RBCs |
| Mean Corpuscular Volume (MCV) | Decreased MCV (less than 80 fL) | Increased MCV (greater than 100 fL) |
| Common Causes | Iron deficiency anemia, thalassemia, anemia of chronic disease | Vitamin B12 deficiency, folate deficiency, alcoholism, liver disease, medications, bone marrow disorders |
| RBC Characteristics | Smaller-sized RBCs, reduced volume, hypochromic appearance | Larger-sized RBCs, increased volume, abnormal morphology |
| Symptoms | Fatigue, weakness, pale skin, shortness of breath | Fatigue, weakness, shortness of breath, pale skin |
| Diagnostic Tests | Complete blood count (CBC), peripheral blood smear, iron studies | CBC, peripheral blood smear, measurement of vitamin B12 and folate levels |
| Treatment | Iron supplementation, dietary changes, transfusions (if severe) | Vitamin B12 or folate supplementation, dietary changes, management of underlying causes |
| Examples | Iron deficiency anemia, thalassemia, anemia of chronic disease | Vitamin B12 deficiency, folate deficiency, alcohol-related anemia, liver disease-related anemia |
Please note that this is a general comparison, and individual cases may have specific variations and additional factors to consider. Always consult with a healthcare professional for accurate diagnosis, treatment, and management of anemia.
Conclusion
Microcytic and macrocytic anemia differ in terms of red blood cell size, causes, symptoms, and treatment approaches. Microcytic anemia is characterized by small red blood cells and is commonly caused by iron deficiency, thalassemia, or chronic diseases. On the other hand, macrocytic anemia involves large red blood cells and often stems from deficiencies in vitamin B12 or folate, medication side effects, or alcohol abuse.
Accurate diagnosis and tailored treatment plans are essential for managing these types of anemia effectively. If you suspect you may have microcytic or macrocytic anemia, consult with a healthcare professional for proper evaluation and guidance.