Definition of Prevention and Cure
These are the definitions of “Prevention” and “Cure”:
Preventive: A method or procedure of preventing something bad from taking place. In the realm of medicine and health, it is a term that refers to actions that are taken to decrease the chance of developing or acquiring an illness or condition. It can include a variety of practices, including vaccination or lifestyle changes (like eating habits and exercises) as well as health education and routine screenings or checks.
Examples:
- The vaccination process is a way to avoid certain illnesses.
- A healthy diet and participating in regular physical activity to avoid heart disease or obesity.
- Smoking less is a good way to avoid lung cancer as well as other respiratory illnesses.
The cure: The restoration of health after an illness or disease. A cure indicates that the condition or disease is eliminated completely in the body. It is not likely to return, unlike treatment that can help or relieve symptoms, without actually eliminating the illness.
Examples:
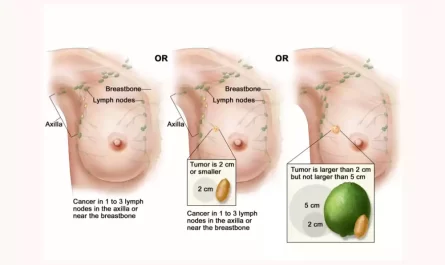
- Antibiotics are able to treat certain infections caused by bacteria.
- The removal of benign tumors may be curative if the entire growth is removed successfully.
- Certain antiviral medicines may cause a prolonged viral response in conditions like Hepatitis C, which is believed to be a cure.

It’s important to keep in mind that, while certain illnesses have cures that are known others are best treated or controlled without any known cure. Furthermore, preventing the onset of a disease is generally more affordable and may yield better results for health instead of waiting to treat or cure a condition once it has begun.
Brief overview of their significance in healthcare
The notions that “prevention” and “cure” provide the fundamental pillars of healthcare, and each plays a crucial role in the overall health of both individuals and groups.
Here’s a quick outline of their importance:
Prevention:
- Reduces the burden of disease: By taking proactive steps to slow the progression of illness, prevention can reduce the incidence of illness within populations, leading to healthier societies.
- Cost-effective: Preventive measures, although sometimes requiring upfront investments (like the vaccination campaign) can result in large savings over the long term in healthcare through avoiding the need for costly treatments or hospitalizations.
- Improves the quality of life: Prevention usually is about healthy lifestyle choices, that not only lower the risk of developing diseases but also improve the quality of life overall. Examples include regular exercise and an energizing diet can not only protect against certain illnesses but also improve overall health.
- Population-Wide Benefits: Certain preventive measures, like vaccinations, may lead to herd immunity that protects those who aren’t vaccinated.
Cure:
- Restoring health: The goal of the treatments is to remove all conditions or diseases of the body allowing people to restore their health and live their regular life.
- Psychology Relief: A chance or success of a cure may bring immense emotional relief to those suffering from the disease and their families in the knowledge that the illness is completely cured.
- Reduces the need for ongoing healthcare: Curing a disease typically signifies that the person doesn’t require constant treatment, freeing medical resources and reducing costs for healthcare.
- is the engine behind Medical Research: The quest for cures drives the medical field forward. The investment in finding cures leads to advances in the field of medical technology as well as pharmaceuticals and the understanding of the causes.
Interdependence in Healthcare:
- Integrative Methodology: While prevention and treatment are both viewed separately however the most efficient healthcare systems are aware of the necessity of the integration of both. Prevention measures can ease the burden upon healthcare providers, which allows them to focus more on curing patients who are already afflicted by illnesses.
- Development of Diseases: As diseases evolve new health risks emerge new health threats emerge, and the balance between treatment and prevention shifts. For instance, if an illness is prevented through vaccination or lifestyle changes The focus shifts from curative to preventative.

Prevention and treatment are crucial to the successful functioning of health systems. They are both complementary and ensure that both current problems with health are taken care of as well as future problems are avoided or reduced.
Comparative Chart of Prevention and Cure
Here’s a comparative chart of “Prevention” and “Cure” in a textual format. In an actual presentation or document, this would be best represented using a table or infographic for clearer visualization.
Prevention vs. Cure Comparative Chart:
| Aspect | Prevention | Cure |
| Definition | Measures taken to reduce the risk of acquiring or developing a disease or condition. | Restoration of health by eradicating a disease or condition from the body. |
| Objective | Stop the disease before it starts. | Eliminate disease after it has started. |
| Cost Implication | Often more cost-effective in the long run due to reduced healthcare needs and hospitalizations. | Can be expensive, especially for complex treatments and long-term diseases. |
| Time Frame | A long-term approach aiming at risk reduction. | Typically a reactive approach is after disease onset. |
| Methods | Vaccination, lifestyle changes, health education, regular screenings. | Medications, surgeries, therapies, alternative treatments. |
| Population Impact | Can benefit entire populations (e.g., herd immunity from vaccinations). | Primarily impacts the individual receiving the cure, though can have societal benefits. |
| Research Focus | Understand risk factors, develop vaccines, and promote healthy behaviors. | Understand disease mechanisms, develop treatments, and improve surgical techniques. |
| Health System Strain | Can reduce strain on health systems by decreasing disease incidence. | Requires robust health systems for treatment, which can strain resources, especially in epidemics. |
| Psychological Aspect | Promotes peace of mind by reducing disease risk. | Offers relief and hope after disease diagnosis. |
| Examples | Flu vaccination, anti-smoking campaigns, regular exercise. | Antibiotic treatment for bacterial infections, chemotherapy for cancer, surgery for tumors. |
This chart provides a general overview and may not capture all nuances of prevention and cure in various specific contexts. However, it offers a comparative snapshot of the two concepts in healthcare.
Historical Context of Prevention and Cure
The history behind “prevention” and “cure” is extensive and covers centuries of public health and medical initiatives.
A full history requires exhaustive research, here’s an overview of the basics:
Ancient Civilizations (c. 3000 BCE – 500 CE)
Prevention:
- Ancient civilizations, such as the Egyptians, Greeks, and Chinese understood the importance of personal hygiene and sanitation. hygiene.
- The Greeks particularly Hippocrates stressed the importance of a healthy lifestyle and diet to maintain good health.
Cure:
- The first medical procedures included a mix of religious ceremonies, natural remedies surgeries, and rituals. For example, the practice of trepanation (drilling holes in the skull) was practiced during the Neolithic period.
- Acupuncture and herbal medicine were popular in ancient China.
Medieval Period (c. 500 CE – 1500 CE)
Prevention:
- Quarantines were introduced in order to limit the spread of infectious diseases particularly those afflicted by the Bubonic Plague.
- A basic understanding of the relationship between water contamination and diseases was in place.
Cure:
- Medical practices were heavily influenced by the church, and numerous illnesses were often blamed on the wrath of God or evil spirits.
- The use of herbal medicines, bloodletting, and purging were the most common methods of treatment.
Renaissance to Early Modern Period (c. 1500 CE – 1800 CE)
Prevention:
- The knowledge of the transmission of diseases was evolving, which led to better healthcare measures for the public.
- The introduction of the smallpox vaccine throughout Europe during the 1800s was an important preventive step.
Cure:
- The results of scientific research resulted in more precise methods of medicine.
- It was the discovery that led to the development of circulation as well and advances in anatomy and physiology have influenced the treatment.
- There was still a strong dependence on leeches, herbs as well and other methods of traditional use.
19th Century
Prevention:
- John Snow’s efforts in London demonstrated the importance of water that is clean in the fight against cholera, highlighting the importance of health care measures for the public.
- The Germ Theory of Disease proposed by Louis Pasteur and Robert Koch revolutionized knowledge of prevention of diseases which led to the creation of vaccines and antiseptics.
Cure:
- The use of chloroform and ether revolutionized the field of surgery, allowing for anesthesia.
- Aspirin was among the earliest drugs to be marketed as a pharmaceutical.
- The discovery of X-rays by Wilhelm Roentgen marked a significant technological advancement in the field of diagnostics.
20th Century to Present
Prevention:
- The widespread vaccination campaign has brought about the eradication (e.g. smallpox, for example)) or reduction in the incidence of a variety of fatal illnesses.
- The World Health Organization and other worldwide organizations have played crucial roles in promoting preventive actions across the globe.
- A focus on lifestyle diseases like heart and diabetes has led to prevention strategies centered around exercise, diet, and abstaining from smoking.
Cure:
- Penicillin was discovered, and the subsequent discovery of antibiotics revolutionized the treatment of bacterial infections.
- The 20th century witnessed rapid advances in surgical methods, including organ transplants.
- The second decade saw improvements in the treatment of chronic illnesses such as HIV/AIDS.
Through time, the focus on prevention and cure has fluctuated in accordance with the current conditions, social needs technological advancements, as well as changing medical expertise. Both have played a crucial role in determining the general health of populations as well as increasing the life expectancy of people.
Understanding Prevention
Understanding the importance of prevention, particularly when it comes to medical and health is vital for people and groups. Prevention is about preventing possible health problems before they develop or get to be severe.
This is an extended look into the prevention process:
Types of Prevention:
- Primary Prevention:
-
- The goal is to: Stop a condition or disease prior to the onset.
- Methods:
-
-
- Immunizations to prevent diseases (e.g. measles the polio virus,).
- Good nutrition is the foundation of health education along with regular workouts.
- Policies and legislation like those that regulate sales of alcohol and tobacco, or require the use of seat belts.
- The provision of safe water for drinking as well as sanitation facilities.
-
- Secondary Prevention:
-
- Goal: Diagnose and treat diseases in the early stages.
- Methods:
-
-
- Regularly scheduled screenings and examinations (e.g. mammograms for colonoscopies, breast cancer screenings, colon cancer, etc.).
- Tests of blood pressure and cholesterol levels test to determine the likelihood of heart disease.
- Encourage self-exams such as self-exams for testicular or breast health.
-
- Tertiary Prevention:
-
- The goal is to: Reduce and manage the complications of a disease that is already diagnosed.
- Methods:
-
-
- Rehabilitation programs for injury or stroke patients.
- Programs for managing chronic diseases such as diabetes or COPD.
- Counseling and support groups for mental health problems.
-
Benefits of Prevention:
- Reduces Health Costs: Effective preventive strategies can result in fewer patients suffering from illnesses which reduces the burden on the healthcare system.
- Cost-effective: Even though preventive measures may incur upfront costs (e.g. financing an entire vaccination campaign) they usually provide substantial long-term health savings by avoiding costly treatment or hospitalizations.
- Enhances the quality of life: Prevention measures, particularly ones that concentrate on lifestyle factors could lead to improved mental and physical health which allows people to live more fulfilled lives.
- Long-Term Impact: Effective prevention, particularly through public health policies and initiatives, can be beneficial to future generations as well as current ones. For instance, a well-planned vaccine program for children can safeguard people throughout their lives and ensure that the next generation is born into a world that has a lesser prevalence of diseases.
Challenges in Prevention:
- awareness: Adequate education and awareness are essential to make preventive measures effective. This is difficult in areas that have limited resources and access to data.
- Social and Cultural Obstacles: Certain preventive strategies could be in conflict with the norms of society or culture and make their implementation difficult.
- Economic Constraints: Countries in the developing world may have difficulty funding large-scale preventive efforts or infrastructure development.
- Complacency: When prevention is effective and rates of disease decrease, individuals may get comfortable, believing that certain measures aren’t required. This is evident in vaccination hesitancy among populations who haven’t suffered the devastating consequences of preventable diseases.
Prevention plays an essential function in the healthcare system by actively taking care of health concerns that could arise which can lead to healthier people and communities. Prevention isn’t only a health-related strategy, it’s also a societal and economic one.
Understanding Cure
“Cure” is a term which, in its simplest sense is the process of restoring health after a condition of illness or disease.
In the field of health, the search for cures is the primary focus of research into medical treatments and development. Delving deeper:
Definition of Cure:
The term “cure” refers to a drug or treatment that cures an illness like a medication surgical procedure lifestyle change or even a philosophic approach to life that eliminates an individual’s illness. It is basically the notion that following medical treatment is completed, the patient does not have that specific disease.
Aspects of Cure:
- Complete vs. Partial:
-
- The Complete Cure: It is completely eradicated from the body, and there is zero chance of repeating.
- Partial Cure: It is managed, and the symptoms could be reduced, but the possibility of recurrence remains.
- Temporal Aspect:
-
- Permanent Cure: This disease has been eliminated forever.
- Temporary Cure: The disease has been eliminated for a short time, but there’s a possibility of the disease recurring.
- The symptomatic as opposed to. Radical:
-
- The Symptomatic Cure: It addresses just the signs of the condition but does not address the underlying causes.
- Radial Cure: The treatment targets the source of the illness, resulting in the elimination of the disease.
Achieving a Cure:
- research: Continuous research is crucial in understanding diseases and finding cures. This includes figuring out the causes of disease and genetics, environmental influences, and much more.
- Clinical Tests: Prior to being considered as a cure, treatments go through strict clinical tests to make sure that they’re safe and effective.
- Technological Developments: Modern tools, from genetic sequencing to the most advanced imaging methods, are revolutionizing our ability to detect, comprehend, and treat illnesses.
Challenges in Achieving a Cure:
- Complexity of diseases: Certain illnesses, specifically ones with multiple causes, such as numerous cancers and autoimmune diseases are inherently complicated which makes them difficult to treat.
- Resistance: Diseases, particularly microbes, may develop resistance to treatment, which makes earlier effective treatments less effective (e.g. resistant bacteria to antibiotics).
- Economic Barriers: Finding cures, specifically sophisticated treatments such as gene therapies could be costly. Access to these treatments may be limited due to differences in the economy.
- Unintended side effects: When searching for a cure, certain treatments can cause negative side effects, often extreme, that could compromise the overall health.
Implications of a Cure:
- Health and Well-being of Patients: A successful treatment can dramatically improve the quality of life of patients, returning their health and extending their lives.
- Economic Effect: Curing diseases can reduce the cost of healthcare over the long term because those who are cured don’t require continuous treatments.
- Social Effects: Curing diseases, particularly those that are infectious, may be beneficial to society in general by decreasing or eliminating the risk of transmission.
The idea that “cure” in healthcare is both a goal and a journey. It is the ultimate level of medical excellence, but it also emphasizes the challenges and complexities that are inherent in tackling illnesses. The search for cures fuels the development of research, innovation, and hope for thousands of people around the globe.
The Interplay Between Prevention and Cure
The connection between treatment and prevention is complex and dynamic. Both play crucial roles in the field of healthcare and their interaction is crucial in ensuring health holistically.
Here’s an investigation of their relationship:
Complementary Nature:
- spectrum of Healthcare: Prevention and treatment can be viewed as two distinct points in a spectrum of healthcare. Prevention seeks to prevent diseases before they develop and cure is focused on dealing with illnesses once they have manifested. Health systems that are effective incorporate both.
- Holistic Methodology: In many instances the lines between cure and prevention blur. For example, tackling hypertension through lifestyle changes and medications does more than treat the problem (cure) however, it also helps prevent possible complications such as strokes or heart attacks (prevention).
Economic Implications:
- Cost savings: Effective prevention can result in significant savings over the long term. For example, vaccination of a population against a particular illness can be more economical than treating thousands of possible cases.
- Resource Allocation: The amount of money that should be invested in preventive measures and curing is a significant policy issue. Some believe that preventive measures can help reduce the burden of healthcare in the future, whereas others advocate the allocation of more resources to search for cures for existing ailments.
Public Health Implications:
- Public Health: Large preventive steps like sanitation programs and mass vaccinations may improve the overall health of a population, and reduce requirements for therapeutic intervention.
- Epidemiological shifts: In the context of preventive measures to help reduce the spread of the spread of infectious diseases, non-communicable illnesses like cardiovascular or diabetes are often more prevalent and the focus shifts to the prevention of and treatment.
Research and Development:
- Guided The focus is: Understanding the potential of diseases and their impact can inform research. If a disease can be prevented research could focus on the development of vaccines or preventive strategies. If the condition is less likely to be prevented but it has a significant impact on the population, finding a cure could be the top priority.
- Feedback Loop: Results from curative therapies can inform preventive strategies. For example, knowing the process by which a disease develops or responds to treatment could result in early detection strategies or changes to risk factors.
Behavioral Aspects:
- The perception of risks: If people believe there’s a solution to a specific disease, they could be less likely to adopt preventive measures. However, the absence of a cure could lead to more rigorous preventive steps.
- Health Literacy: The process of educating the population about prevention as well as available treatments helps make informed choices about the health of people and their treatments.
Ethical Considerations:
- access and equity: The balance between prevention and cure raises ethical questions regarding who has access to which resources. For instance, could money be diverted from treatment programs in order to invest in preventive strategies that could help future generations?
- Informed Choices: The public should be aware of the benefits and dangers of both curative and preventive treatments as well as ensuring autonomy in the making of health-related choices.
Prevention and treatment aren’t necessarily mutually exclusive but are rather interconnected elements of a comprehensive health system. Their interplay illustrates the complexity of healthcare decisions, resource allocations, and societal expectations.
Both are crucial and the best health strategy is often found in making use of the strengths of both to provide the long-term as well as immediate health benefits for people and their communities.
Future Trends in Healthcare
Future healthcare will be shaped by the advancement of technology, the changing demands of patients as well as global health challenges as well as changes in economic and political conditions.
When we look towards the future, a number of key developments are predicted to revolutionize the world of health care:
- The Internet of Things (HTML0) and remote healthcare: The COVID-19 pandemic has accelerated the acceptance of telehealth solutions. In the near future, there will be more follow-ups, and consultations as well as some diagnostics that could be conducted via telemedicine, thereby facilitating convenience and expanding access to healthcare.
- Artificial Intelligence (AI) and Machine Learning: These technologies are set to further be integrated into the field of diagnostics as well as treatment planning and healthcare management. AI aids in the early detection of disease and personalized treatment plans and even helps in predicting patient demands.
- Wearable Health Technology: Devices like smartwatches and fitness trackers are currently monitoring vital indicators and levels of activity. Future wearables could provide more extensive health monitoring that includes everything from glucose levels to the brain’s activity.
- precision Medicine: Treatment will be more tailored to the individual patients. Through advancements in the field of genomics and personalized medicine treatments will be tailored according to the genetic makeup of the patient as well as specific characteristics of the disease.
- Decentralized Clinical Trials: Utilizing wearables and digital tools pharmaceutical businesses can carry out virtual or decentralized clinical trials that allow for the participation of more patients from different backgrounds and possibly expediting the development of new drugs.
- Mental Health Integration: The world is gaining awareness of the significance of mental well-being. Future models of healthcare will be more seamless in integrating physical and mental healthcare.
- 3D Printing: You can use it for making prosthetics, specific surgical instruments, or the possibility of producing organs with 3D printers, 3D printing could take on a larger role in the world of healthcare.
- Augmented Reality (AR) and Virtual Reality (VR): These tools can aid in planning surgical procedures as well as medical education and even therapy (like for PTSD or phobias).
- Blockchains in Healthcare: Blockchain technology is a secure, traceable, and effective way to manage medical records electronically, oversee clinical trials, and verify the authenticity of medicines.
- Healthcare Consumerism: The patients are now more active and knowledgeable of their condition. They’ll be demanding greater transparency, choice, and control in their health choices.
- Value-based Care: Instead of fee-for-service models there’s a shift toward value-based care where the providers are compensated according to the results of their patients.
- sustainable healthcare: With an aging global population and a rising number of chronic illnesses, there’s a demand for sustainable healthcare models that balance high-quality care with the resources available.
- Global Health Collaboration: Pandemics and antibiotic resistance call for global collaboration. Look for more global collaboration in health strategy as well as information-sharing platforms.
- Regenerative medicine: Methods such as CRISPR to edit genes as well as advances in stem cell therapy are paving the way for treatments that help repair or regenerate damaged organs and tissues.
- Fusion of Life Sciences and Technology: Traditional tech and pharmaceutical companies will be more collaborative and will result in rapid technological advancements in healthcare.
- Resolving Health Disparities: The government will place an increased focus on the issue of healthcare disparities and ensuring that all people have equal access to top-quality care.
As exciting as these developments appear, they are not without issues like ethical concerns privacy issues, as well as the possibility of a rise in health disparities if they are not implemented with care. The overall trend indicates a future in which healthcare is more customized accessible, efficient, and cost-effective.
Conclusion
The changing healthcare landscape is characterized by technological advances as well as a better understanding of the needs of patients, and the development of global collaborative strategies. As we move into our future healthcare, it is set to become more individualized accessible, efficient, and affordable.
Although there are still challenges the confluence of technological advances and changing paradigms will bring a new era of wellbeing and health. The potential lies not only in treating illnesses but an overall approach that focuses on the well-being, prevention, and empowerment of patients.