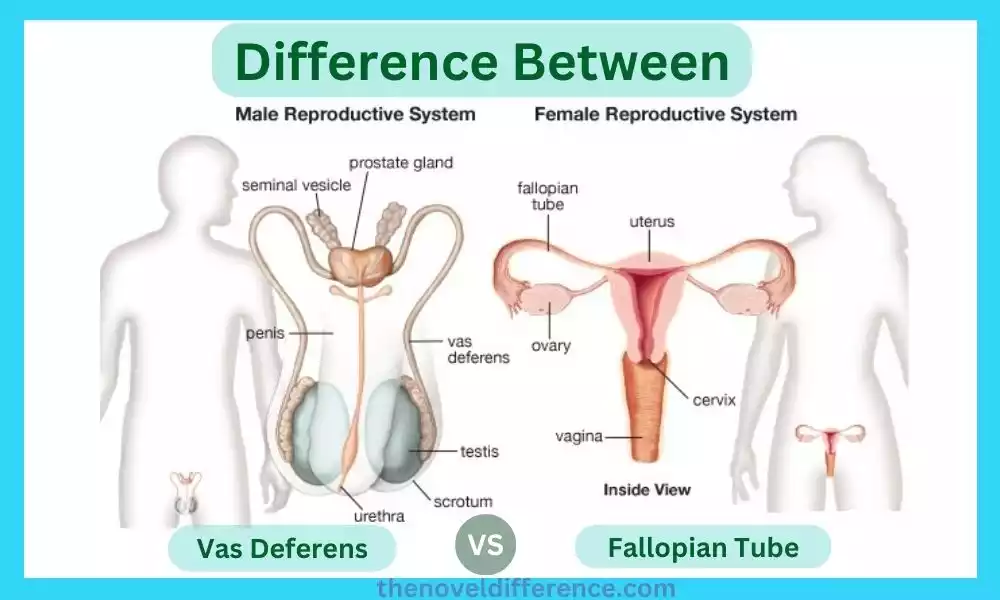
The male and female reproductive systems exhibit fascinating intricacies and differences, which contribute to the miracle of life. Within these systems, the vas deferens and fallopian tube play crucial roles in transporting reproductive cells. While both structures facilitate the movement of essential cells, they have distinct anatomical features and functions. We’ll dive into the contrasts between the vas deferens and the fallopian tube, shedding light on their special characteristics.
Introduction
Understanding the human regenerative framework can be an intriguing and complex theme. We are going to dig into the complexities of the male and female regenerative frameworks by investigating the key contrasts between two imperative structures: the vas deferens and the fallopian tube. While both play crucial roles in fertility, they are distinct in their anatomy, function, and overall purpose. So, let’s embark on this educational journey and unravel the mysteries of the vas deferens and fallopian tubes.
Importance of understanding the specific structures within the reproductive systems
Understanding the specific structures within the reproductive system is of significant importance for several reasons:
1. Reproductive Health: Knowledge about the structures enables individuals to make informed decisions regarding their reproductive health. Understanding how the reproductive organs function and interact helps in recognizing signs of potential issues or abnormalities. It energizes people to look for therapeutic counsel and experience customary check-ups, driving to early locations and treatment of regenerative well-being conditions.
2. Fertility and Family Planning: A thorough understanding of the reproductive structures is crucial for individuals or couples planning to conceive. Knowing the forms included, such as sperm and egg generation, transportation, and fertilization, permits them to optimize their chances of effective conception. Awareness of factors that can affect fertility, such as blocked fallopian tubes or low sperm count, helps in seeking appropriate medical interventions or fertility treatments.
3. Contraception and Safe Sex: Familiarity with the structures aids in making informed choices regarding contraception methods and practicing safe sex. Information almost the male and female regenerative frameworks empowers people to get it how different prophylactic strategies, such as condoms or hormonal birth control, work to anticipate pregnancy. It advances mindful sexual behavior and decreases the hazard of unintended pregnancies or sexually transmitted diseases.
4. Reproductive Disorders and Diseases: Understanding the specific structures facilitates the recognition and understanding of reproductive disorders and diseases. Information around conditions like endometriosis, polycystic ovary disorder (PCOS), or prostate issues makes a difference in people recognizing side effects and looking for opportune restorative consideration. It empowers individuals to engage in discussions with healthcare professionals, leading to proper diagnosis and effective treatment options.
5. Patient-Healthcare Provider Communication: Knowing the reproductive structures enhances communication between patients and healthcare providers. It enables individuals to articulate their concerns, ask relevant questions, and actively participate in discussions about their reproductive health. This open exchange cultivates a collaborative approach to healthcare, driving us to make strides in determination, treatment, and general well-being.
6. Education and Empowerment: Understanding the reproductive structures contributes to overall sexual and reproductive education. It engages people to form educated choices almost their bodies, connections, and sexual well-being. By promoting comprehensive and accurate knowledge, it helps dispel myths, reduce stigma, and promote a healthy attitude toward reproductive health and sexuality.
A thorough understanding of the specific structures within the reproductive system is crucial for reproductive health, fertility, contraception, disease prevention, effective communication with healthcare providers, and overall education and empowerment. It plays a crucial part in guaranteeing individuals’ well-being, empowering them to create educated choices, and effectively taking an interest in overseeing their regenerative well-being.
Definition of Vas Deferens and Fallopian Tube
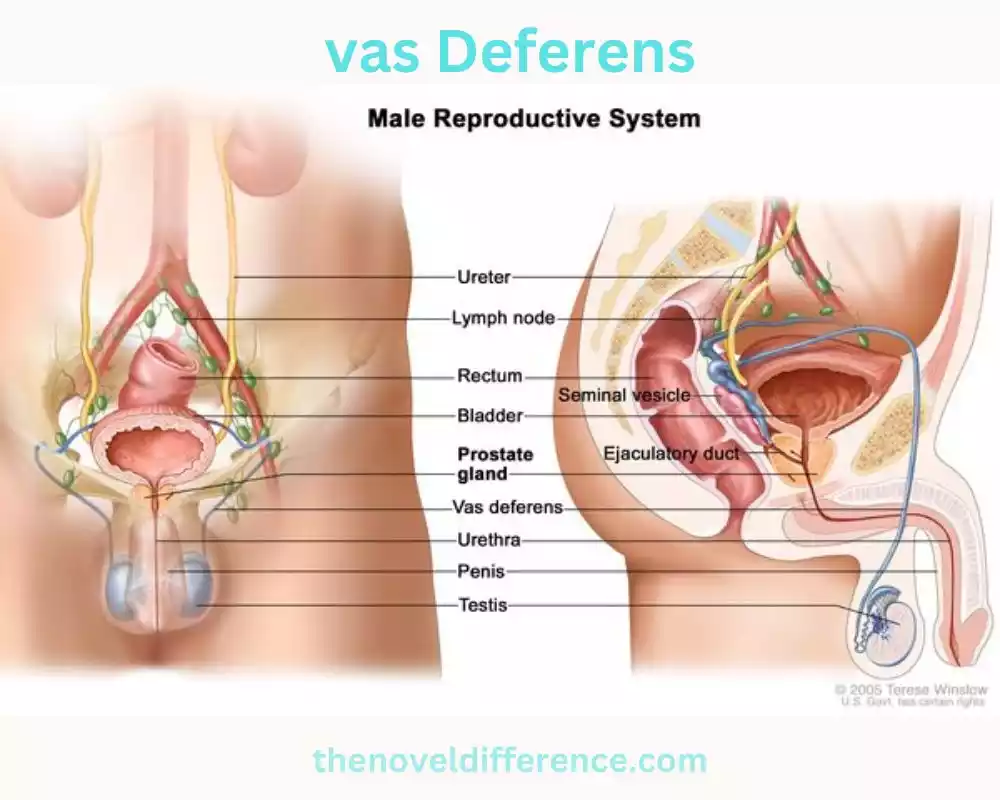
Vas Deferens: The vas deferens, moreover known as the ductus deferens, could be a long, strong tube that shapes a portion of the male regenerative framework. It is dependable for transporting develop sperm from the epididymis, where they are put away and experience development, to the ejaculatory channels and eventually to the urethra. The vas deferens play a basic part in the drive of sperm amid ejaculation, permitting them to be discharged from the body amid sexual movement. It is found inside the spermatic line and voyages from the testicles, through the inguinal canal, and into the pelvic locale.
Fallopian Tube: The fallopian tubes, moreover called uterine tubes or oviducts, are a match of slim tubes found within the female regenerative framework. They extend from the sides of the uterus and open near the ovaries. The fallopian tubes play an imperative part in the preparation of fertilization and early embryonic improvement. Amid ovulation, an egg (ovum) is discharged from the ovary and captured by the funnel-shaped conclusion of the fallopian tube called the infundibulum.
The cilia lining the inner walls of the fallopian tube help to move the egg toward the uterus. If fertilization happens, it regularly happens inside the fallopian tube as sperm travel from the uterus to meet the egg. The fertilized egg at that point voyages through the fallopian tube and into the uterus for implantation and advanced advancement.
Both the vas deferens and the fallopian tube are pivotal structures inside the particular male and female regenerative frameworks, serving as conduits for the transportation of regenerative cells—sperm within the case of the vas deferens and eggs within the case of the fallopian tube.
What is Vas Deferens?
The vas deferens, moreover known as the ductus deferens, could be a part of the male regenerative framework. It could be a long, solid tube that interfaces the epididymis, a coiled structure on the back of each gonad, to the ejaculatory conduits. The vas deferens serve as a conduit for the transportation of developing sperm from the epididymis to the urethra amid ejaculation.
The vas deferens are responsible for propelling sperm forward through peristaltic contractions of its muscular walls. It transports sperm from the gonads, where they are conveyed, to the urethra, the tube that carries both pee and semen out of the body.
Amid sexual excitement, sperm move from the epididymis into the vas deferens, where they are put away and experience advanced development. When ejaculation happens, cadenced withdrawals of the vas deferens move sperm into the ejaculatory channels, where they blend with seminal liquid delivered by the seminal vesicles, prostate organ, and bulbourethral organs. This combination forms semen, which is expelled through the urethra.
The vas deferens play a vital part within the regenerative handle by encouraging the transport of sperm for fertilization. It is an imperative component of male richness and is additionally focused on amid vasectomy, a surgical strategy for male contraception, where the vas deferens are cut and fixed to avoid the discharge of sperm amid ejaculation.
Function and Role in sperm transportation
The vas deferens plays an imperative work in the transportation of sperm inside the male regenerative framework. Its role can be summarized as follows:
1. Sperm Storage: After sperm are delivered within the testicles, they travel through a structure called the epididymis, where they experience development and are put away. The vas deferens interface with the epididymis, serving as a supply for developing sperm until they are required for ejaculation.
2. Sperm Transportation: During sexual arousal and ejaculation, the muscular walls of the vas deferens contract, propelling the stored sperm forward. These compressions, known as peristalsis, make wave-like developments that thrust the sperm along the length of the vas deferens.
3. Mixing with Seminal Fluid: As the sperm travel through the vas deferens, they mix with seminal fluid produced by the seminal vesicles, prostate gland, and bulbourethral glands. This fluid provides nourishment and various substances that support the survival, motility, and function of the sperm.
4. Junction with the Ejaculatory Duct: Near the base of the bladder, the vas deferens join with the seminal vesicle to form the ejaculatory duct. The ejaculatory conduits pass through the prostate organ and purge into the urethra. This junction allows the sperm and seminal fluid to combine and continue their journey toward the urethra.
5. Final Path to the Urethra: The urethra serves as a shared passageway for both urine and semen. Amid ejaculation, the sperm, in conjunction with the seminal liquid, enter the urethra using the ejaculatory channels. From there, they are expelled from the body through the penis.
The vas deferens act as a conduit for creating sperm, allowing them to be transported from the epididymis to the urethra for ejaculation. Its muscular contractions, along with the interaction with seminal fluid, facilitate the movement and successful delivery of sperm during the reproductive process.
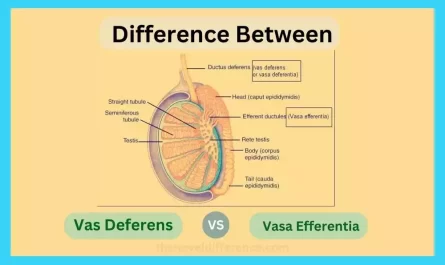
Structure and composition of the vas deferens
The vas deferens have a specific structure and composition that supports their function in sperm transportation.
Here are the key aspects of the structure and composition of the vas deferens:
1. Tubular Structure: The vas deferens could be a long, lean tube that measures approximately 30 centimeters (12 inches) in length. It is coiled and convoluted in shape, located within the spermatic cord, and runs from each testicle, through the inguinal canal, and into the pelvic region.
2. Three Layers of Tissue: The walls of the vas deferens are composed of three layers of tissue, each with its function.
a. Inner Mucosa: The innermost layer is the mucosa, which is lined with a specialized epithelial tissue called the pseudostratified columnar epithelium. This lining has numerous microvilli that increase the surface area for absorption and secretion.
b. Middle Muscular Layer: The middle layer of the vas deferens is composed of smooth muscle fibers. These muscle fibers provide the contractile force needed for peristaltic movements, propelling the sperm forward during ejaculation.
c. Outer Connective Tissue Layer: The furthest layer is made up of connective tissue, which gives basic bolster and makes a difference to grapple the vas deferens inside the encompassing tissues.
3. Lumen: The central hollow space within the vas deferens is known as the lumen. It serves as the pathway for the transportation of sperm.
4. Ciliated Epithelium: The mucosal lining of the vas deferens is lined with ciliated epithelial cells. These cilia beat in coordinated motions, aiding the movement of sperm by creating currents and directing them along the length of the vas deferens.
5. Spermatic Ducts: At the proximal end of the vas deferens, it connects with the epididymis, which serves as a storage and maturation site for sperm. At the distal conclusion, the vas deferens join with the seminal vesicle to create the ejaculatory conduit, which at that point consolidates with the urethra.
The structure and composition of the vas deferens are planned to encourage the transport of developed sperm cells from the epididymis to the urethra amid ejaculation. The muscular contractions, ciliary movements, and specialized tissue layers work together to ensure the smooth and efficient passage of sperm through this important reproductive duct.
What is the Fallopian Tube?
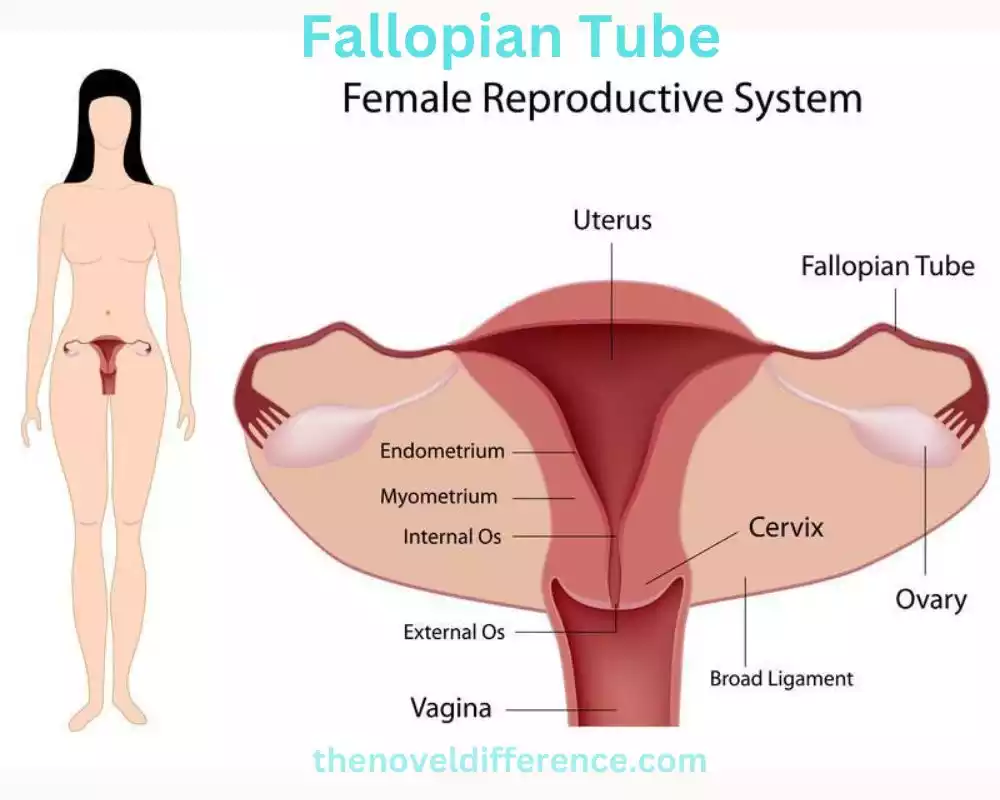
The fallopian tubes, moreover known as uterine tubes or oviducts, are a combination of slim, tube-like structures within the female regenerative framework. Each fallopian tube extends from the upper lateral region of the uterus and opens near the ovaries. The fallopian tubes play a significant part in the reproductive handle, especially within the transportation of eggs and the location of fertilization.
Here are key aspects of the fallopian tube:
1. Structure and Location: The fallopian tubes are around 10-12 centimeters (4-5 inches) long and are arranged on each side of the uterus. They consist of several segments, including the infundibulum, the ampulla, and the isthmus. The infundibulum is the funnel-shaped, outermost portion with finger-like projections called fimbriae that help capture the released egg from the ovary.
2. Pathway for Egg: The fallopian tubes provide a pathway for eggs (ova) to travel from the ovaries to the uterus. Amid ovulation, which ordinarily happens once a month, an egg is discharged from one of the ovaries. The fimbriae of the fallopian tube sweep over the ovary to capture the egg, drawing it into the fallopian tube’s opening.
3. Ciliary Movement: The inner lining of the fallopian tubes is covered with tiny, hair-like structures called cilia. These cilia create coordinated, wave-like movements that help propel the egg along the length of the fallopian tube toward the uterus. The ciliary movement also assists in moving sperm toward the egg for fertilization.
4. Site of Fertilization: The fallopian tubes are the primary site of fertilization in the female reproductive system. On the off chance that sperm are displayed within the fallopian tubes amid ovulation, they can meet the egg and fertilize it inside the ampulla, the largest and longest portion of the fallopian tube. Fertilization happens when a sperm enters the external layer of the egg, driving the arrangement of a fertilized developing life.
5. Transportation and Nourishment: The fallopian tubes serve as a conduit for the fertilized egg, also known as a zygote, to travel from the site of fertilization to the uterus. The ciliary movement and muscular contractions of the fallopian tubes help propel the fertilized egg toward the uterus. The fallopian tubes also provide a supportive environment and nourishment for the early-developing embryo during its journey.
6. Ectopic Pregnancy: A fertilized egg may implant and develop outside of the uterus, most commonly within the fallopian tube. Usually known as ectopic pregnancy and can be a medical crisis as the fallopian tube isn’t outlined to back the development of developing life. Ectopic pregnancies require immediate medical attention.
The fallopian tubes are necessary for the method of fertilization and early embryonic advancement. They encourage the transportation of eggs, give a location for fertilization, and serve as a pivotal pathway for the fertilized egg to reach the uterus for implantation and advanced improvement.
Function and Role in the fertilization process
The fallopian tubes play a pivotal work in the process of fertilization within the female regenerative framework.
Their role can be summarized as follows:
1. Capture and Transport of Eggs: The fallopian tubes capture eggs (ova) that are released from the ovaries during ovulation. The fimbriae, finger-like projections after the fallopian tubes, clear over the ovaries, making a tender suction that makes a difference and draws the egg into the fallopian tube. The fimbriae guide the egg into the tube’s opening and initiate its journey toward the uterus.
2. Site of Fertilization: The fallopian tubes serve as the primary site of fertilization. In case sexual intercut happens close to the time of ovulation, sperm can rise through the cervix, enter the uterus, and reach the fallopian tubes. Fertilization occurs within the fallopian tube when sperm encounter the egg. Sperm cells discharge proteins that offer assistance break down the defensive external layer of the egg, permitting one sperm to enter and fertilize the egg. The fertilized egg, presently called a zygote, starts its early improvement inside the fallopian tube.
3. Transportation of the Fertilized Egg: Once fertilization occurs, the fallopian tubes facilitate the transportation of the fertilized egg from the site of fertilization toward the uterus. The ciliary movement, the coordinated beating of tiny hair-like structures called cilia lining the fallopian tubes, creates currents that help propel the fertilized egg through the tube. The muscular contractions of the fallopian tube walls also aid in moving the embryo along its journey.
4. Nourishment and Support: The fallopian tubes provide a nurturing environment for the developing embryo during its passage toward the uterus. The tube’s secretions and ciliary movement help nourish and protect the fertilized egg, allowing it to undergo early cell divisions and development. The fallopian tubes create an optimal environment for the early stages of embryonic growth.
5. Implantation and Pregnancy: After several days of traveling through the fallopian tube, the fertilized egg reaches the uterus. If conditions are favorable, the developing life inserts into the uterine lining, where it sets up an association with the maternal blood supply and proceeds to develop and create. The fallopian tubes play an imperative part in directing the fertilized egg to the uterus, setting the organization for the potential foundation of pregnancy.
The fallopian tubes capture and transport eggs, give the location for fertilization, help with the transportation of the fertilized egg toward the uterus, and make a supportive environment for early embryonic advancement. They are critical structures in the reproductive system, facilitating the union of sperm and egg and supporting the initial stages of pregnancy.
Structure and composition of the fallopian tube
The fallopian tubes, moreover known as uterine tubes or oviducts, have a particular structure and composition that underpins their work within the female regenerative framework.
Here are the key angles of the structure and composition of the fallopian tube:
1. Tubular Structure: Each fallopian tube may be a slim, empty tube that measures approximately 10-12 centimeters (4-5 inches) in length. They are paired structures located on each side of the uterus.
2. Segments: The fallopian tube can be divided into three main segments.
a. Infundibulum: The infundibulum is the funnel-shaped, outermost part of the fallopian tube. It is characterized by finger-like projections called fimbriae. The fimbriae make a periphery after the fallopian tube, with the biggest one, known as the ovarian fimbria, coming toward the ovary. The fimbriae help capture the released egg (ovum) from the ovary during ovulation.
b. Ampulla: The ampulla is the wider and longer middle segment of the fallopian tube. It is the most common site for fertilization to occur when sperm and egg meet. The ampulla provides an optimal environment for fertilization due to its size and the presence of nourishing secretions.
c. Isthmus: The isthmus is the narrowest and shortest segment of the fallopian tube. It connects the ampulla to the uterine cavity.
3. Lining: The inner lining of the fallopian tube is composed of various types of epithelial cells. The cells within the fallopian tube are specialized to carry out particular capacities related to the transport and food of the egg and developing life. The lining is covered with cilia, which are tiny hair-like structures that beat in coordinated waves to create currents and move the egg and embryo along the fallopian tube.
4. Smooth Muscle: The walls of the fallopian tubes contain layers of smooth muscle tissue. These muscles are responsible for the rhythmic contractions that help propel the egg and embryo through the tube toward the uterus. The muscular contractions, along with the ciliary movement, facilitate the transportation of the egg and early embryo.
5. Blood Supply: The fallopian tubes receive blood supply from branches of the uterine arteries. The blood vessels provide oxygen and nutrients to the tubal tissues, supporting their proper function.
The structure and composition of the fallopian tube are particularly planned to encourage the capture of eggs, give a reasonable environment for fertilization, help with the transportation of the fertilized egg, and back early embryonic improvement. The combination of ciliary movement, muscular contractions, and specialized epithelial cells enables the fallopian tubes to fulfill their essential role in the reproductive process.
Differences Between Vas Deferens and Fallopian Tube
The vas deferens and fallopian tubes are two unmistakable structures within the regenerative frameworks of guys and females, separately.
Here are the key differences between the vas deferens and the fallopian tube:
1. Location and Orientation:
• Vas Deferens: The vas deferens are located within the male reproductive system. It expands from the epididymis, which is arranged on the back of each gonad, up through the spermatic rope, and enters the pelvic depression.
• Fallopian Tube: The fallopian tubes are part of the female reproductive system. They are positioned on each side of the uterus, extending from the upper lateral region and reaching toward the ovaries.
2. Function:
• Vas Deferens: The essential work of the vas deferens is to transport developed sperm from the epididymis to the urethra amid ejaculation. It acts as a conduit for sperm delivery.
• Fallopian Tube: The fallopian tubes serve as the passageway for eggs (ova) to travel from the ovaries to the uterus. They are moreover the location of fertilization, where sperm can meet and fertilize the egg.
3. Composition and Structure:
• Vas Deferens: The walls of the vas deferens consist of three layers: inner mucosa, middle muscular layer, and outer connective tissue layer. The inner lining is composed of pseudostratified columnar epithelium, and the middle layer contains smooth muscle fibers responsible for peristaltic contractions.
• Fallopian Tube: The fallopian tubes also have three layers: inner mucosa, middle muscular layer, and outer serosa. The inner lining is lined with specialized epithelial cells, including ciliated cells that aid in egg and embryo transportation. The muscular layer helps propel the egg through the tube.
4. Role in Reproductive Process:
• Vas Deferens: The vas deferens play a critical role in sperm transportation and the delivery of sperm for fertilization. It carries sperm from the testicles to the urethra, permitting ejaculation amid sexual action.
• Fallopian Tube: The fallopian tubes are essential for the transport of eggs, the site of fertilization, and the initial stages of embryo development. They capture the released eggs, facilitate the meeting of sperm and egg, and transport the fertilized egg (zygote) toward the uterus.
5. Reproductive Impact:
• Vas Deferens: If the vas deferens are surgically interrupted or blocked, such as through vasectomy, it prevents the passage of sperm during ejaculation, resulting in male infertility.
• Fallopian Tube: If the fallopian tubes are damaged, blocked, or impaired, it can hinder the fertilization process and increase the risk of infertility or ectopic pregnancy.
The vas deferens and fallopian tubes contrast in their area, work, composition, and part within the regenerative preparation. The vas deferens are included in sperm transportation in guys, whereas the fallopian tubes encourage egg transport, fertilization, and early embryonic advancement in females.
Similarities Between Vas Deferens and Fallopian Tube
Whereas the vas deferens and fallopian tubes are particular structures with diverse capacities within the male and female reproductive systems.
There are many similitudes between them:
1. Tubular Structure: Both the vas deferens and fallopian tubes have a tubular structure. They are long, slender, and hollow, providing a pathway for the transportation of reproductive cells.
2. Muscular Walls: Both the vas deferens and fallopian tubes have muscular walls that aid in the movement of contents within the tubes. The muscular contractions help propel sperm in the vas deferens and eggs/embryos in the fallopian tubes.
3. Epithelial Lining: Both structures have an inner lining composed of specialized epithelial cells. These cells play a role in the transport and support of reproductive cells. The lining of the fallopian tubes includes ciliated cells that create coordinated movements to facilitate the movement of eggs and embryos.
4. Connection to Reproductive Organs: Both the vas deferens and fallopian tubes are connected to other reproductive organs. The vas deferens interface the epididymis to the urethra in guys, whereas the fallopian tubes interface the ovaries to the uterus in females.
5. Role in Reproductive Process: Both structures are involved in the reproductive process, albeit in different capacities. The Vas Deferens Transports Sperm From the Epididymis to the Urethra for Ejaculation, While the Fallopian Tubes Transport Eggs and Provide an Area for Fertilization and Early Embryonic Headway.
Whereas the vas deferens and fallopian tubes have these likenesses, it is imperative to note that their capacities and parts contrast essentially due to the unmistakable regenerative forms happening in guys and females.
Clinical Relevance and Health Considerations
Both the vas deferens and fallopian tubes have clinical relevance and health considerations associated with them.
Here are some key points:
Clinical Relevance of Vas Deferens:
1. Vasectomy: Vasectomy is a surgical procedure that involves cutting or blocking the vas deferens to prevent the passage of sperm. It is a form of permanent male contraception.
2. Vasectomy Reversal: Vasectomy reversal is a surgical procedure aimed at reconnecting the vas deferens to restore fertility in men who have previously undergone vasectomy.
3. Congenital Anomalies: Some individuals may be born with abnormalities or malformations of the vas deferens, such as absence or blockage, which can impact fertility.
Health Considerations for Vas Deferens:
1. Infections: Inflammation or infection of the vas deferens, known as epididymitis, can occur and may cause pain, swelling, and discomfort.
2. Obstruction: Blockage or obstruction of the vas deferens can lead to infertility as it prevents the passage of sperm during ejaculation.
3. Sperm Abnormalities: Some genetic or structural abnormalities can affect the quality or movement of sperm within the vas deferens, leading to fertility issues.
Clinical Relevance of Fallopian Tubes:
1. Tubal Factor Infertility: Blockage or damage to the fallopian tubes can result in tubal factor infertility, where eggs cannot reach the uterus or sperm cannot meet the egg for fertilization.
2. Ectopic Pregnancy: When a fertilized egg inserts and creates the exterior of the uterus, most commonly inside the fallopian tube, it leads to an ectopic pregnancy. This condition can be life-threatening and requires prompt restorative intercession.
3. Tubal Ligation: Tubal ligation, also known as “getting one’s tubes tied,” is a surgical procedure in which the fallopian tubes are blocked or sealed to prevent pregnancy permanently.
Health Considerations for Fallopian Tubes:
1. Infections: Diseases of the fallopian tubes, such as pelvic incendiary illness (PID), can cause irritation, scarring, and harm to the tubes, driving to barrenness or expanded hazard of ectopic pregnancy.
2. Tubal Blockage: Blockage or obstruction of the fallopian tubes can prevent the passage of eggs or sperm, resulting in fertility issues.
3. Hydrosalpinx: Hydrosalpinx is a condition where the fallopian tube is blocked and filled with fluid, which can impair fertility and the success of assisted reproductive techniques such as in vitro fertilization (IVF).
Understanding the clinical relevance and health considerations associated with the vas deferens and fallopian tubes is crucial for diagnosing and addressing reproductive health issues, implementing contraceptive measures, and managing fertility-related concerns.
Conclusion
The vas deferens and fallopian tubes, despite being integral components of the reproductive system, exhibit distinctive features. Whereas the vas deferens encourage the transportation of sperm, the fallopian tube gives a pathway for eggs and serves as the location of fertilization. Recognizing the structural and functional dissimilarities between these two structures is essential for comprehending reproductive health, fertility treatments, and associated clinical implications.