Candida Albicans and Candida Auris Importance
Candida albicans is an important species in the Candida genus. However, it has different characteristics.
Here are some of the most important aspects that highlight their importance:
Candida albicans and its importance:
- Prevalence & Clinical Impact: Candida Albicans is most commonly associated with human infections. It can cause a variety of symptoms, such as oral thrush and vaginal infections. Healthcare systems face an immense financial strain from this infection, particularly among immunocompromised individuals.
- Commensal Microbiota: Candida Albicans is part of the normal human microbiota and can be found both inside the digestive system as well as the oral cavity or even the urinary system. When the balance of microbes is disturbed, they can change from commensal bacteria to pathogenic ones.
- Pathogenic mechanisms: Candida Albicans contains several virulence factors which contribute to its pathogenicity, such as adhering to tissue, producing enzymes that damage cells, and evasion from host immune responses. Understanding these mechanisms will help you develop effective strategies for fighting candidiasis.
- Antifungal Resistant: Candida albicans, while generally susceptible to antifungal drugs is a cause for concern. Antifungal Resistance can limit treatment options and complicate the treatment process.
Candida auris – Importance:
- Emerging global health threat: Candida Auris has attracted significant attention as it is a multidrug resistant pathogen. It has caused healthcare-associated outbreaks in different regions of the world, posing challenges for infection control and patient management. The ability of the bacteria to survive on surfaces and resist routine disinfection contributes to their global spread.
- Antifungal Resistant: Candida Auris is resistant to multiple antifungal drug classes, including azoles and echinocandins. In some cases, it also shows resistance to amphotericin. The limited treatment options due to this resistance profile make it difficult to treat. Global spread of Candida auris multidrug resistant strains highlights the need for new antifungal drugs and infection control measures.
- Diagnostic Challenges: Candida Auris may be misidentified by laboratory tests or not detected at all. For the proper management of patients and infection control, it is important to make an accurate and timely diagnosis. To address these challenges, improved diagnostic techniques for Candida auris were developed.
- Healthcare-Associated Infections: Candida auris primarily affects vulnerable individuals in healthcare settings, such as those with prolonged hospital stays, invasive medical procedures, or compromised immune systems. It can cause invasive infections that increase mortality and morbidity.
It is important for healthcare professionals, policymakers, and researchers to understand the importance of Candida albicans as well as Candida auris. This will assist them in diagnosing, treating and preventing candidiasis as well as handling multidrug-resistant Candida strains more effectively.
A brief overview of Candida Species
Candida is a genus of yeast that belongs to the fungal kingdom. It encompasses various species, some of which are commensal organisms found naturally in the human body, while others can cause infections under certain conditions.
Candida species are opportunistic pathogens, meaning they take advantage of weakened immune systems or imbalanced microbial environments to cause infections.
The most common and well-known species within the Candida genus is Candida albicans. It is a normal inhabitant of the human microbiota, particularly in the gastrointestinal tract and mucous membranes.
However, it can become pathogenic and cause a wide range of infections, collectively known as candidiasis, in susceptible individuals. Candida albicans is responsible for most cases of candidiasis and often leads to oral thrush, vaginal yeast infections, and systemic infections in immunocompromised patients.
In recent years, another species called Candida auris has emerged as a significant healthcare-associated pathogen. Unlike Candida albicans, Candida auris is less common in the human microbiota and is characterized by its multidrug-resistant properties.
It can cause severe invasive infections and has the ability to persist on environmental surfaces, leading to outbreaks in healthcare settings. Candida auris is considered a global health threat due to its resistance to multiple antifungal drugs and the challenges it poses for diagnosis and control.
Besides Candida albicans and Candida auris, there are several other Candida species that can cause infections in humans, albeit less frequently.
These include Candida glabrata, Candida parapsilosis, Candida tropicalis, and Candida krusei. Each species has distinct characteristics and may exhibit variations in their pathogenicity, antifungal susceptibility, and clinical manifestations.
Understanding the differences among Candida species is paramount to accurate diagnosis, effective therapy and successful candidiasis management.
Candida Albicans
Candida albicans is a species of yeast that is part of the normal microbiota in many individuals. Humans typically contain it in their digestive system, oral cavity and genitourinary tract. While it typically exists as a harmless commensal organism, under certain conditions, it can become pathogenic and cause infections.
Here are some key aspects of Candida albicans:
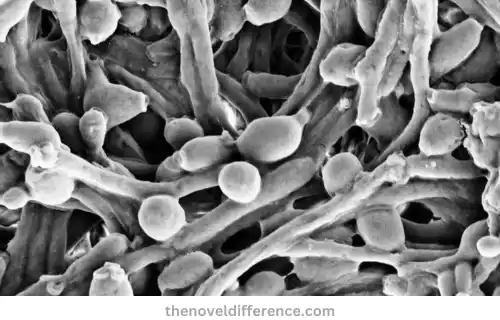
Morphology: Candida albicans is an oval-shaped yeast with one nucleus. It reproduces asexually by budding, forming daughter cells that detach and mature into independent organisms. It can also form pseudohyphae and true hyphae, which are filamentous structures that aid in tissue invasion.
Pathogenicity: Candida albicans can cause a variety of infections collectively known as candidiasis. Common manifestations include oral thrush (white patches in the mouth), vaginal yeast infections, and invasive candidiasis. It possesses several virulence factors, such as adhesins, hydrolytic enzymes, and the ability to switch between different forms (yeast, pseudohyphae, and hyphae), which contribute to its pathogenic potential.
Risk Factors: Certain factors can increase the likelihood of Candida albicans infections. Examples include immunosuppression due to HIV/AIDS infection or organ transplantation; use of broad-spectrum antibiotics; uncontrolled diabetes mellitus; pregnancy; hormone fluctuations or use of immunosuppressant drugs. These conditions disrupt the natural balance of microbial communities, enabling Candida albicans overgrowth.
Infections: Candida albicans infections can occur in various body sites. Oral candidiasis affects the mouth and throat, causing discomfort, pain, and difficulty swallowing. Vaginal candidiasis leads to itching, burning, abnormal discharge, and discomfort in the vaginal area. Invasive candidiasis occurs when the yeast enters the bloodstream and can affect multiple organs, posing a significant risk, particularly to immunocompromised individuals.
Treatment: Candida albicans infections are typically treated with antifungal medications. The choice of antifungal agent depends on the severity and location of the infection. Commonly used antifungal drugs include fluconazole, itraconazole, and echinocandins. However, the emergence of antifungal resistance, particularly in recurrent or chronic infections, poses challenges in treatment and requires alternative therapeutic strategies.
Prevention: Preventive measures for Candida albicans infections include maintaining good hygiene, practicing safe sex, avoiding unnecessary use of antibiotics, managing underlying medical conditions, and following a balanced diet. In healthcare settings, adherence to infection control protocols, such as proper hand hygiene, catheter care, and environmental disinfection, is essential to minimize the risk of transmission.
Healthcare professionals need a full grasp of Candida albicans’ characteristics, pathogenicity and treatment options in order to properly identify, treat and prevent candidiasis.
Candida Auris
Candida auris is a species of yeast that has emerged as a significant healthcare-associated pathogen in recent years. Candida auris has gained widespread notice because of its multidrug resistance properties and subsequent challenges that it presents for diagnosis, treatment and infection control measures.

Here are some key aspects of Candida auris:
Morphology: Candida auris appears under a microscopical microscope as small, oval-shaped cells. It is often arranged in clusters called “a bunch of grapes” due to its characteristic budding pattern.
Candida auris: Candida auris is well known for being resistant to multiple classes of antifungal drugs, including azoles and echinocandins – and even amphotericin B in some instances. This resistance can complicate treatment and limit therapeutic options, requiring the use of less commonly used antifungal agents.
Global Spread: Candida auris has rapidly spread across the world, affecting healthcare facilities in different countries. An outbreak was linked with it occurring at hospitals, long-term care facilities, and other healthcare settings. Its ability to persist on environmental surfaces contributes to its transmission potential.
Diagnostic Challenges: Identifying Candida auris can be challenging using routine laboratory methods. Conventional identification techniques may misidentify it as another Candida species, leading to delays in the appropriate management and implementation of infection control measures. Accurate and timely diagnosis requires specific laboratory tests such as molecular techniques.
Clinical Manifestations: Candida auris primarily causes invasive infections, particularly bloodstream infections (candidemia). It can also affect other sites, such as the respiratory tract, urinary tract, and wounds. Candida auris infections have been associated with higher rates of mortality among critically ill and immunocompromised individuals, particularly among critically ill individuals who cannot defend against infections on their own.
Infection Control Measures: Due to its ability to persist on surfaces and its resistance to routine disinfection, preventing the transmission of Candida auris requires robust infection control measures. These include strict adherence to hand hygiene, appropriate use of personal protective equipment, patient isolation, and environmental cleaning and disinfection protocols.
Research and Surveillance: Ongoing studies aim to gain greater insights into the epidemiology, transmission dynamics and mechanisms underlying antifungal resistance within Candida auris.Surveillance efforts have been strengthened to monitor its global spread and identify new cases promptly.
The emergence and global spread of multidrug-resistant Candida auris highlight the importance of early detection, appropriate treatment strategies, and rigorous infection control practices in healthcare settings.
Improvement in laboratory diagnostics, antimicrobial stewardship, and research efforts is crucial in confronting Candida auris infections head on and mitigating its negative impacts on public health.
General characteristics
Candida species (C. albicans and C. auris) possess several key features, as outlined here:
Yeast: Candida species are unicellular fungi that belong to the yeast family. They exist as individual cells rather than forming multicellular structures like molds.
Ubiquitous Distribution: Candida species are commonly found in various environments, including soil, water, and the human body. They are part of the normal microbial flora in the oral cavity, gastrointestinal tract, and female genital tract.
Dimorphic: Many Candida species, including Candida albicans, exhibit a dimorphic growth pattern. Based on environmental conditions, they can switch between yeast form (unicellular) and filamentous form (hyphal or pseudohyphal).
Opportunistic Pathogens: Candida species are considered opportunistic pathogens. Healthy individuals typically don’t experience adverse reactions from microbes found on mosquito bites; however, those with compromised immunity such as those living with HIV/AIDS or cancer could become infected by them.
Candidiasis: Candida species are associated with a spectrum of infections collectively known as candidiasis. These infections range from superficial, such as oral thrush and vaginal yeast infections, to more invasive forms like bloodstream infections or deep organ involvement.
Biofilm Formation: Candida species have the ability to form biofilms, which are complex communities of cells embedded in a matrix. Biofilms contribute to the virulence and resistance of Candida infections, making them challenging to treat.
Antifungal Resistance: Candida species, including Candida auris, have shown varying degrees of resistance to antifungal drugs. This resistance can limit treatment options and complicate the management of Candida infections.
Laboratory Identification: Identification of Candida species typically involves culturing the organism on specific media and performing biochemical tests. To facilitate accurate and timely identification, molecular techniques like DNA sequencing or polymerase chain reactions (PCR) may be employed.
Infection Control Measures: Preventing the transmission of Candida infections requires strict adherence to infection control measures, particularly in healthcare settings. These measures include hand hygiene, appropriate use of personal protective equipment, and disinfection of environmental surfaces.
Understanding the basic characteristics of Candida species is crucial in order to diagnose, treat, and prevent candidiasis. It enables healthcare professionals to implement appropriate strategies for infection control and patient management.
Candida Albicans vs Candida Auris in Tabular Form
Certainly! Here’s a tabular comparison between Candida albicans and Candida auris:
| Aspect | Candida albicans | Candida auris |
|---|---|---|
| Morphology | Oval-shaped yeast with budding ability | Oval-shaped yeast, often clustered like a “bunch of grapes” |
| Filamentation | Forms pseudohyphae and true hyphae | Limited filamentation ability |
| Pathogenicity | Can cause a wide range of infections | Primarily causes invasive infections, especially bloodstream infections (candidemia) |
| Antifungal Resistance | Generally susceptible to common antifungals | Multidrug-resistant, high resistance to multiple antifungal classes, including azoles and echinocandins |
| Epidemiology | Widespread in human microbiota, no specific geographic clustering | Global spread, associated with healthcare-associated outbreaks |
| Diagnostic Challenges | Generally identifiable with routine laboratory methods | Difficult to identify accurately, requires specialized identification techniques |
| Clinical Impact | The common pathogen in candidiasis, various clinical manifestations | Significant morbidity and mortality rates, especially in immunocompromised patients |
| Infection Control | Standard infection control measures apply | Requires strict infection control measures due to persistence on surfaces and resistance to routine disinfection |
| Public Health Implications | Significant but not a major public health concern | Considered a serious public health threat, necessitating vigilant surveillance and control measures |
Please be aware that this table provides an accessible summary of the main differences between Candida albicans and Candida auris. It is important to consider that the characteristics and impacts of these species may vary in different clinical and geographical contexts.
Morphological differences
Candida albicans and Candida auris exhibit some morphological differences, which can be observed under a microscope.
Below are the distinguishing morphological features of both species:
Candida albicans:
Shape: Candida albicans is an oval-shaped yeast. It typically appears as single, rounded cells with a clear cell wall.
Budding: Candida albicans reproduce asexually by budding. This process involves the formation of smaller daughter cells (buds) that grow on the surface of the parent cell before separating.
Filamentation: Candida albicans have the ability to produce pseudohyphae and true hyphae, which are elongated, filamentous structures. These hyphal forms facilitate tissue invasion and contribute to the pathogenicity of Candida albicans.
Candida auris:
Shape: Candida auris also appears as oval-shaped yeast cells, similar to Candida albicans.
Clustering: Candida auris cells have a tendency to cluster together, forming dense groups that resemble a “bunch of grapes” when observed under a microscope. This clustering pattern is one of the distinguishing features of Candida auris.
Limited Filamentation: Unlike Candida albicans, Candida auris has reduced filamentation ability. It typically does not form extensive pseudohyphae or true hyphae.
Candida albicans and Candida auris both share an oval form common among many yeast species; however, two distinctive features distinguishing Candida auris from its close relative are its clustered pattern of growth and reduced filamentation ability as opposed to Candida albicans.
These morphological distinctions can aid in the laboratory identification and differentiation of the two species.
What are the similarities between Candida Albicans and Candida Auris?
While Candida albicans and Candida auris have distinct characteristics, they also share some similarities.
Here are the commonalities between the two species:
Candida Genus: Candida albicans and Candida auris are two species within the Candida genus that commonly inhabit human microbiota.
Opportunistic Pathogens: Candida albicans and Candida auris are opportunistic pathogens, meaning they cause infections primarily in individuals with compromised immune systems or in specific clinical settings, such as healthcare facilities.
Candidiasis: Both species can cause candidiasis, a group of fungal infections that can occur in various body sites. Candidiasis can range from mild localized infections, such as oral thrush and vaginal yeast infections, to more severe systemic infections.
Candida Species: Candida albicans and Candida auris are part of a larger family of Candida species that can cause infections in humans. Common pathogenic Candida species include Candida glabrata, Candida parapsilosis, Candida tropicalis and Candida krusei.
Diagnostic Challenges: Both species may present diagnostic challenges in the laboratory. Candida albicans can sometimes be misidentified or overlooked due to its similarities to other Candida species, while Candida auris requires specialized identification techniques for accurate diagnosis.
Antifungal Treatment: Candida albicans and Candida auris can both be effectively managed using antifungal medication. However, the choice of antifungal agents and the management approach may differ due to the multidrug resistance exhibited by some Candida auris strains.
Infection Control Measures: Effective infection control measures are crucial in preventing the transmission of both Candida albicans and Candida auris infections. Proper hand hygiene, patient isolation, environmental disinfection, and adherence to infection control protocols are essential in healthcare settings to minimize the spread of these pathogens.
Although Candida albicans and Candida auris have differences in their clinical impact, antifungal resistance, and morphological characteristics, they are both significant species within the Candida genus and require attention in the diagnosis, management, and prevention of candidiasis.
Conclusion
Both Candida albicans and Candida auris are important members of the Candida genus; however, each strain exhibits unique features and has significant clinical ramifications.
Candida albicans is an infectious yeast often encountered and responsible for infections like oral thrush, vaginal yeast infections, and invasive candidiasis. With its distinctive pseudohyphae and hyphae formation it typically responds well to antifungal medication used against it.
Candida auris is becoming an increasing global health threat associated with increased morbidity and death rates among immunocompromised people.
Candida auris has an easily distinguishable clustering morphology with limited filamentation ability posed challenges when diagnosing and controlling infection due to resistance and persistence on surfaces.
Understanding the differences between Candida albicans and Candida auris is paramount to accurate diagnosis, appropriate treatment selection, and successful candidiasis management.
