Brief Overview of Ankylosing Spondylitis and Degenerative Disc Disease
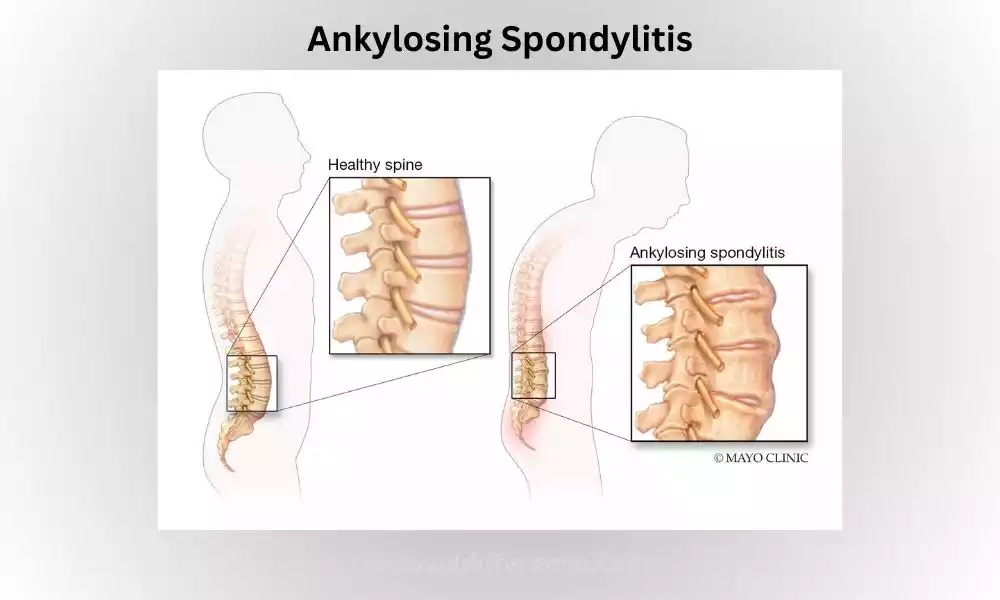
Ankylosing Spondylitis (AS): Ankylosing Spondylitis (AS) is an inflammatory, persistent condition that primarily impacts the spine. As its name implies, ASD causes pain and stiffness around it.
It is classified as a form of arthritis, specifically a type of spondyloarthritis. AS primarily affects the joints and ligaments of the spine, leading to inflammation, fusion of the vertebrae, and reduced flexibility.
The exact cause of AS is unknown, but it is believed to involve a combination of genetic and environmental factors. The presence of a specific genetic marker called HLA-B27 is strongly associated with the development of AS.
AS typically begins in early adulthood, often affecting individuals in their late teens or twenties. It affects men more frequently than women. The symptoms of AS can vary from person to person, but common features include chronic lower back pain, stiffness, and reduced range of motion.
The pain and stiffness are usually worse in the morning or after periods of inactivity, and they tend to improve with exercise or physical activity.
Diagnosing AS involves a combination of clinical evaluation, imaging tests (such as X-rays and magnetic resonance imaging), and blood tests to detect markers of inflammation, including HLA-B27. Early diagnosis is important to initiate appropriate treatment and prevent long-term complications.
Treatment for AS aims to relieve symptoms, reduce inflammation, and improve function. It typically involves a multidisciplinary approach, combining medication, physical therapy, exercise, and lifestyle modifications.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are widely utilized to manage pain and inflammation. In more severe cases, biologic medications that target specific molecules involved in inflammation may be prescribed. Regular exercise and postural exercises are also important to maintain flexibility and reduce stiffness.
If left untreated, AS can lead to complications such as fusion of the spine (ankylosis), reduced lung function, and involvement of other joints, eyes, or organs. However, with appropriate management and treatment, many individuals with AS are able to lead active and fulfilling lives.
Degenerative Disc Disease (DDD): Degenerative Disc Disease (DDD) is a condition marked by the gradual breakdown and degeneration of intervertebral discs located throughout the spine, acting as shock absorbers while permitting flexibility for movement in between vertebrae. DDD typically affects the cervical (neck) and lumbar regions of the spine.
DDD often results from natural aging processes; however, injury, repetitive strain, and genetics may also contribute to its development. Over time, discs lose water content, becoming thinner and thus becoming less capable of absorbing shocks evenly while dispersing forces evenly; less flexible discs could then become painful or cause discomfort for those living with DDD.
DDD symptoms vary considerably between individuals; some may show no visible symptoms whatsoever while others can suffer chronic backache, stiffness, and reduced mobility. The pain usually starts in one area of the spine but could travel into arms or legs depending on where its discs lie – activities like bending forward can aggravate it further.
Diagnosing DDD involves a comprehensive examination, medical history review, and imaging tests such as x-rays, magnetic resonance imaging (MRI), or computed tomography scans – these will allow doctors to visualize disc degeneration as well as identify any additional possible sources for symptoms.
Treatment for DDD usually entails relieving symptoms and improving quality of life, using conservative approaches like rest, physical therapy, and exercises designed to strengthen surrounding muscles and increase flexibility. In extreme cases, nerve blocks or epidural steroid injectables can provide temporary relief.
Surgery should only be considered for severe cases of DDD that do not respond to conservative treatments, including discectomy (removal of part of the damaged disc), spinal fusion, or artificial disc replacement surgery.
Important to know, while degeneration in discs cannot be reversed, symptoms associated with DDD may often be managed successfully through conservative treatments and lifestyle modifications.
Maintaining a healthy weight and following good posture practices, refraining from smoking, and engaging in physical activities on an ongoing basis, these factors could all help stop or slow the progression of DDD.
Importance of understanding the difference between Ankylosing Spondylitis and Degenerative Disc Disease
It is important to understand the differences between Ankylosing spondylitis (AS), and Degenerative Disc Disease(DDD) for many reasons:
Accurate Diagnosis: Ankylosing Spondylitis and Degenerative Disc Disease differ significantly in terms of causes, pathophysiology, and treatment approaches. By understanding the differences, healthcare professionals can make an accurate diagnosis, ensuring appropriate management and preventing delays in treatment.
Treatment Planning: Ankylosing Spondylitis and Degenerative Disc Disease require different treatment strategies. AS is an inflammatory condition that often requires medications targeting inflammation, such as NSAIDs or biologics. DDD, on the other hand, typically focuses on pain management and physical therapy. Knowing the specific condition helps tailor treatment plans to address the underlying mechanisms and optimize outcomes.
Prognosis and Long-Term Management: Ankylosing Spondylitis and Degenerative Disc Disease have different long-term implications. AS is a chronic condition that can lead to spinal fusion, reduced mobility, and extra-spinal manifestations. DDD involves the degeneration of intervertebral discs and may lead to chronic pain and limited mobility. Understanding the prognosis and potential complications associated with each condition enables healthcare providers to develop appropriate long-term management plans and provide the necessary support.
Patient Education and Empowerment: Patients benefit from understanding their diagnosis, including the differences between Ankylosing Spondylitis and Degenerative Disc Disease. It helps them comprehend their condition, manage expectations, and actively participate in their treatment plans. Educating patients about their condition can also promote self-management strategies and lifestyle modifications that can improve their quality of life.
Research and Advancements: Distinguishing between Ankylosing Spondylitis and Degenerative Disc Disease is essential for research purposes. By studying these conditions separately, researchers can gain insights into the underlying mechanisms, develop targeted therapies, and advance medical knowledge.
Referrals and Collaborative Care: Understanding the differences between Ankylosing Spondylitis and Degenerative Disc Disease enables appropriate referrals and collaboration among healthcare professionals. Patients may require input from rheumatologists, Orthopedic specialists, physical therapists, and other healthcare providers depending on their diagnosis. Accurate communication and collaboration among specialists lead to comprehensive care for patients.
Understanding the difference between Ankylosing Spondylitis and Degenerative Disc Disease is vital for accurate diagnosis, individualized treatment planning, long-term management, patient education, research advancements, and collaborative care. This ensures patients receive the best care and support for their condition. It leads to better outcomes and a higher quality of Life.
Ankylosing Spondylitis (AS)
Ankylosing Spondylitis (AS) is a chronic inflammatory condition that predominantly impacts the spine, leading to pain and stiffness. AS belongs to the family of diseases known as Spondyloarthritis which involves inflammation in the joints and ligaments – however, AS can affect other parts of your body such as hips shoulders, or peripheral joints as well.
AS has no single cause; however, researchers believe its roots lie within both genetics and environment. HLA-B27 appears to be strongly linked with AS development but not all individuals carrying the marker will manifest symptoms of the condition.
AS is typically diagnosed in early adulthood – typically around the late teens or twenties for men; though children and older adults can also be affected. Males appear more commonly than females.
Individual symptoms vary, though chronic lower back pain, stiffness, reduced range of motion, and morning discomfort/inactivity exacerbated pain/stiffness are typical features; improving with physical activity (like exercise).
AS symptoms extend far beyond spinal symptoms and inflammation to other parts of the body as well. Uveitis (inflammation of the eyes), inflammatory bowel disease, skin rashes, and fatigue are just a few extra-spinal manifestations, though other conditions linked with AS may include increased risks like osteoporosis and cardiovascular disease.
The diagnosis of AS is a combination between clinical evaluations, imaging tests (such as X-rays and magnetic resonance imaging), and blood tests that detect inflammation markers like HLA-B27. Early diagnosis can help provide timely treatments while also helping avoid potential long-term complications.
Treatment for AS is designed to alleviate symptoms, decrease inflammation and enhance function. Multidisciplinary approaches include medication, physical therapy, and lifestyle modifications.
In cases of severe pain or inflammation, biological medication targeting specific molecules that are involved in inflammation is often prescribed. Furthermore, regular postural exercises help maintain flexibility and ease stiffness for improved performance.
Untreated AS can result in complications including spinal fusion (ankylosis), reduced lung function, and involvement of other joints, eyes, or organs.
With proper management and treatment, however, many individuals living with AS are able to lead active lives while living fulfilling lives – ongoing monitoring with healthcare providers helps assess disease activity as needed so treatment plans may be adjusted as necessary.
Definition and Etiology
Ankylosing Spondylitis (AS), is a progressive chronic inflammatory condition that impacts an individual’s spine and the sacroiliac joint of their spinal skeleton, leading to inflammation, stiffness, and pain in affected areas. Over time this may even result in vertebral fusion reducing mobility and flexibility within the spine.
AS has no definitive cause, though researchers believe its development likely involves both genetic and environmental elements. Genetic predisposition has an especially prominent role, as the presence of the HLA-B27 genetic marker has been found strongly linked with AS. But not everyone with HLA-B27 will develop symptoms; other factors must play their part too.
The environment can play an influential role in AS development. Infections caused by certain bacteria (Klebsiella pneumoniae) have been implicated in initiating immune reactions which lead to AS in genetically susceptible individuals; more research must be completed in this field to fully comprehend the role of environmental factors on AS development.
Immunology plays an integral part in the pathogenesis of AS. In genetically susceptible individuals, their immune systems mistakenly identify components of their own tissues like spinal or sacroiliac joints as foreign or pathogenic and activate an inflammatory response which ultimately manifests as the characteristic symptoms and structural changes seen with AS.
AS is an inflammation disease, predominantly impacting its entheses (the sites at which ligaments, tendons, and joint capsules attach to bone). Over time, chronic inflammation may result in bone erosion, new bone formation (ankylosis), or even joint fusion – particularly among spinal joints.
AS is usually diagnosed in early adulthood; however, cases have also been documented among children and elderly individuals. Men tend to be affected more than women; with an approximate 2:1 male-female ratio.
Though its exact cause remains unknown, research continues to uncover its underlying mechanisms and contributing factors. Such knowledge provides key advantages when diagnosing symptoms accurately, creating targeted treatments, improving quality-of-life measures for those living with AS, and ultimately providing greater outcomes and improvements overall for individuals living with the condition.
Degenerative Disc Disease (DDD)
Degenerative Disc Disease (DDD) is a condition characterized by the gradual breakdown and degeneration of the intervertebral discs in the spine.
The intervertebral discs act as cushions between the vertebrae, providing shock absorption and allowing flexibility in the spine. DDD commonly affects the cervical (neck) and lumbar (lower back) regions of the spine.
The exact cause of DDD is often related to the natural aging process, although other factors such as injury, repetitive strain, and genetics can contribute to its development.
As we age, the discs lose water content and become thinner, leading to a reduction in their ability to absorb shocks and distribute forces evenly. This can result in the discs becoming less flexible, which may cause pain and discomfort.
The degeneration of the discs in DDD can manifest in various ways. The outer layer of the disc, called the annulus fibrosus, may develop small tears or cracks, leading to disc herniation or bulging.
The inner gel-like substance of the disc called the nucleus pulposus, may also undergo changes, such as dehydration or breakdown.
The symptoms of DDD can vary widely from person to person. Some individuals may experience no symptoms at all, while others may have chronic pain, stiffness, and reduced mobility.
The pain is often localized in the affected area of the spine and may radiate to the arms or legs, depending on the location of the affected discs. Activities such as bending, lifting, or twisting may worsen the pain.
Diagnosis of DDD involves a combination of clinical evaluation, medical history, and imaging tests such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans. These tests can help visualize the degeneration of the discs, as well as identify any other potential causes of the symptoms.
Treatment for DDD is typically focused on managing symptoms and improving quality of life. Conservative approaches may include rest, physical therapy, and exercises to strengthen the surrounding muscles and improve flexibility.
Pain relief medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or analgesics may be prescribed. In some cases, epidural steroid injections or nerve blocks can be used to provide temporary pain relief.
Surgery is generally considered a last resort for severe cases of DDD that do not respond to conservative treatments. Surgical options may include discectomy (removal of a portion of the damaged disc), spinal fusion (joining two or more vertebrae together), or artificial disc replacement.
It’s important to note that while the degenerative changes in the discs are irreversible, the symptoms of DDD can often be managed effectively through a combination of conservative treatments and lifestyle modifications.

Maintaining a healthy weight, practicing good posture, avoiding smoking, and engaging in regular exercise can also help prevent or slow down the progression of DDD.
Definition and Etiology
Degenerative Disc Disease (DDD) is a condition marked by gradual degradation and degeneration of intervertebral discs located between vertebrae in the spine that serve as shock absorbers, providing cushioning while simultaneously permitting flexibility in movement of the vertebral column.
These discs also play an essential part in providing cushioned protection to vertebrae as shock absorbers for cushioned movement in flexing back the back in different ways – providing cushioning support as well as flexibility between vertebrae in various directions in the flexibility of movement of the spinal column flexibility.
DDD has multiple causes that contribute to its development; age is the main culprit here; as we age, intervertebral discs lose some water content and become dehydrated, decreasing in height and elasticity and becoming susceptible to degeneration; this process is known as disc degeneration.
Other contributing factors for DDD could include age-related factors:
Genes: Studies indicate that genetic factors play a key role in susceptibility to disc degeneration. Certain variants and mutations have been linked to an increased risk for DDD.
Mechanical Factors: Repeated physical stress on the spine can hasten its degeneration. Jobs or activities requiring heavy lifting, bending, or twisting could place excessive strain on intervertebral discs – thus contributing to their degeneration.
Trauma or Injury: Traumatic incidents such as falls, car accidents, and sports-related injuries can damage intervertebral discs quickly and speed up degenerative processes.
Poor Posture: Over time, maintaining poor posture can add additional strain on intervertebral discs and hasten their degeneration. Slouching or sitting hunched for extended periods is likely to damage their health and pose risks to the overall wellness of intervertebral discs.
Smoking: Cigarette smoking has been linked with an increased risk of DDD. The chemicals contained within tobacco smoke may reduce blood supply to intervertebral discs, impairing their ability to receive nourishment and ultimately leading to their degeneration.
Important to keep in mind is that while DDD may be associated with aging, not everyone will show symptoms or significant degeneration of discs. Furthermore, severity can differ among individuals.
Understanding the causes and mechanisms underlying DDD helps develop strategies to prevent and treat it effectively. Lifestyle modifications like maintaining good posture, engaging in regular physical exercise sessions, limiting mechanical strain on the spine, and quitting smoking all play key roles in keeping intervertebral discs healthy while helping slow their degenerative progression.
Differences Between Ankylosing Spondylitis and Degenerative Disc Disease
Here are the key differences between Ankylosing Spondylitis (AS) and Degenerative Disc Disease (DDD):
- Underlying Causes:
- AS: An autoimmune disease with a strong genetic component (HLA-B27), where the immune system attacks the joints and ligaments of the spine.
- DDD: Primarily age-related degeneration of the intervertebral discs, although factors such as genetics, mechanical stress, and injuries may contribute.
- Age of Onset:
- AS: Typically begins in early adulthood, often in the late teens or twenties.
- DDD: More common in older adults as a natural part of the aging process, although it can occur at any age.
- Inflammatory Component:
- AS: Inflammatory condition with chronic inflammation affecting the spine and other joints. Extra-spinal manifestations like uveitis, inflammatory bowel disease, and skin conditions can also occur.
- DDD: Not primarily an inflammatory condition. Inflammation, if present, is usually secondary to degenerative changes and may not be as significant.
- Location and Pattern of Pain:
- AS: Predominantly affects the axial skeleton, particularly the lower back and sacroiliac joints. The pain is often chronic and can be symmetric, with morning stiffness that improves with activity.
- DDD: Commonly affects the cervical and lumbar regions of the spine. Pain is typically localized in the affected disc and may radiate to the arms or legs. Pain can worsen with certain movements or activities.
- Radiographic Findings:
- AS: X-rays and other imaging tests show characteristic findings such as sacroiliitis (inflammation of the sacroiliac joints), syndesmophytes (bony growths), and fusion of the spine.
- DDD: Imaging may reveal disc degeneration, such as disc height loss, disc herniation, or disc bulging. There may also be the presence of osteophytes (bone spurs).
- Extra-Spinal Manifestations:
- AS: Can involve other areas of the body, including the eyes (uveitis), heart, lungs, and gastrointestinal system.
- DDD: Primarily affects the spine, with fewer extra-spinal manifestations.
- Treatment Approaches:
- AS: Treatment focuses on managing inflammation, relieving pain, and preserving mobility. Medications, physical therapy, exercise, and lifestyle modifications are commonly employed. Biologic medications may be used for more severe cases.
- DDD: Treatment aims to manage pain, and improve function, and quality of life. Conservative approaches include physical therapy, exercises, pain medications, and lifestyle modifications. Surgery may be considered for severe cases that do not respond to conservative measures.
Understanding these key differences is crucial for accurate diagnosis, appropriate treatment planning, and optimal management of patients with AS or DDD. It ensures that individuals receive the most suitable interventions and support tailored to their specific condition.
Similarities between Ankylosing Spondylitis and Degenerative Disc Disease
Ankylosing Spondylitis (AS) and Degenerative Disc Disease (DDD) each present with unique characteristics; yet these two conditions share many similarities as well.
Here are a few key similarities:
Spinal Involvement: Both Ankylosing Spondylitis and Degenerative Disc Disease primarily affect the spine. They can cause pain, stiffness, and reduced mobility in the affected areas of the spine.
Chronic Pain: Both conditions can lead to chronic pain. Individuals with Ankylosing Spondylitis and Degenerative Disc Disease may experience persistent discomfort in the back or neck, and the pain may worsen with certain movements or activities.
Impact on Daily Functioning: Ankylosing Spondylitis and Degenerative Disc Disease can both affect a person’s daily functioning and quality of life. The pain, stiffness, and reduced mobility associated with these conditions may limit a person’s ability to perform certain tasks, participate in physical activities, or engage in hobbies and recreational activities.
Management of Symptoms: While the treatment approaches may differ, both Ankylosing Spondylitis and Degenerative Disc Disease aim to manage symptoms and improve the individual’s quality of life. Pain management, physical therapy, exercise, and lifestyle modifications are commonly employed in the management of both conditions.
Impact on Mental Well-being: Living with chronic pain and a potentially debilitating condition can have an impact on an individual’s mental well-being. Both Ankylosing Spondylitis and Degenerative Disc Disease may contribute to feelings of frustration, stress, anxiety, or depression. It is important for individuals with these conditions to receive appropriate support and care for their mental health as well.
While AS is an inflammatory condition with an autoimmune component and DDD is primarily a degenerative process, recognizing the similarities between the two conditions can help healthcare professionals provide comprehensive care and support to individuals affected by these spine-related disorders.
Ankylosing Spondylitis and Degenerative Disc Disease in Tabular Form
Certainly! Here’s a tabular comparison of Ankylosing Spondylitis (AS) and Degenerative Disc Disease (DDD):
| Aspect | Ankylosing Spondylitis (AS) | Degenerative Disc Disease (DDD) |
|---|---|---|
| Underlying Causes | Autoimmune disease, genetic predisposition (HLA-B27) | The aging process, genetics, mechanical stress |
| Age of Onset | Typically starts in early adulthood (late teens to twenties) | More common in older adults, but can occur at any age |
| Inflammatory Component | Inflammatory condition with chronic inflammation | Not primarily an inflammatory condition |
| Location of Pain | Predominantly affects the axial skeleton (lower back, sacroiliac joints) | It commonly affects the cervical and lumbar regions of the spine |
| Radiographic Findings | X-rays may show sacroiliitis, syndesmophytes, fusion of the spine | Imaging may reveal disc degeneration, herniation, osteophytes |
| Extra-Spinal Manifestations | Uveitis, involvement of eyes, heart, lungs, gastrointestinal system | Primarily affects the spine, fewer extra-spinal manifestations |
| Treatment Approaches | Managing inflammation, pain relief, preserving mobility | Pain management, improving function, lifestyle modifications |
| Impact on Daily Functioning | Can limit mobility and affect daily activities | Can limit mobility and affect daily activities |
| Impact on Mental Well-being | Can contribute to frustration, stress, anxiety, depression | Can contribute to frustration, stress, anxiety, depression |
While Ankylosing Spondylitis and Degenerative Disc Disease share several similarities and distinctions, each requires customized diagnosis, treatment, and management in accordance with the unique set of needs and characteristics of its patient.
Conclusion
Ankylosing Spondylitis and Degenerative Disc Disease are two distinct spinal conditions that have similar clinical symptoms but different causes, symptoms, and treatment approaches.
AS is an autoimmune inflammatory condition that predominantly impacts the spine, often beginning in early adulthood and lasting into old age. This chronic inflammation often results in pain, stiffness, and potential vertebral fusion; furthermore, it often exhibits extraspinal symptoms which require multidisciplinary management including medication, physical therapy, and exercise programs for its effective control.
DDD is an age-related process where intervertebral disks degenerate over time. This leads to increased pain, decreased mobility, and possible disc bulging or herniation. More often seen among older adults; treatment typically includes pain management strategies along with physical therapy sessions and lifestyle modifications.
