Definition of Appendicitis and Crohn’s Disease
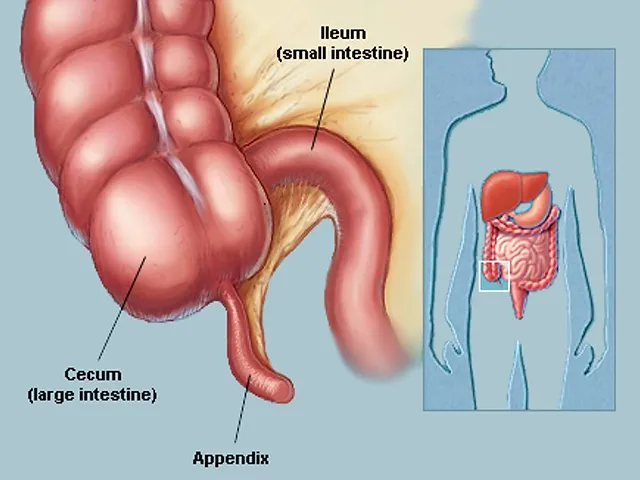
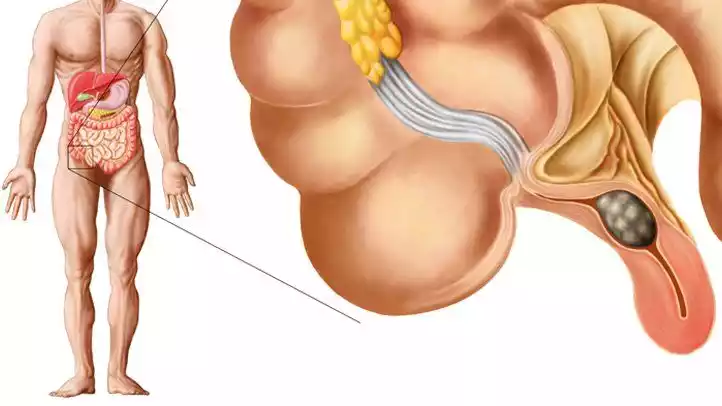
Appendicitis: Appendicitis refers to irritation of the appendix. It is a tiny pouch-like structure that extends from the earliest part of the large intestinal tract (cecum). The precise reason for appendicitis is usually not known, but it could be caused by an obstruction in the appendix as a result of foreign bodies, fecal matter, or, in certain instances, tumors.
The most common symptoms are abdominal pain which is right lower nausea, vomiting, and fever. If untreated the appendix may rupture, resulting in the possibility of a life-threatening illness called peritonitis (inflammation of the abdominal cavity’s lining). Treatment usually involves an operation to eliminate the appendix (appendectomy).
Crohn’s disease: Crohn’s disease is an inflammatory intestinal disease (IBD) that may affect every part of the digestive (GI) tract starting from the mouth and ending at the anus. However, it most often affects the lower part of the small intestine (ileum) and the beginning of the colon.
The root cause of Crohn’s disease is not fully understood, however, it is believed to be an interaction between environmental, genetic as well and immune systems. The illness is characterized by periods of complete remission as well as flare-ups.
The symptoms vary but usually include abdominal discomfort as well as diarrhea (which could be bloody) as well as weight loss and fatigue. There is no cure for Crohn’s disease. However, treatments can help reduce symptoms and keep them in indefinite remission. Treatments may include medication or diet changes, as well as in cases of more severe severity surgery.
The importance of distinguishing between them
The previous model we used in this discussion is no longer available. We’ve redirected you to the most current model which is the default.
Differentiating between appendicitis and Crohn’s disease is crucial for several reasons:
- Different Treatment Strategies: Appendicitis needs immediate surgical intervention to eliminate the appendix inflamed (appendectomy). Failure to treat it promptly can result in a rupture of the appendix, which can lead to life-threatening complications. Contrary to that, Crohn’s Disease is a chronic disease that usually requires long-term medical care including diet and medication. The confusion between these two conditions could result in a wrong treatment and cause damage or worsening of the disease.
- Preventing the need for Surgery: The mistake of diagnosing Crohn’s disease as appendicitis can result in unnecessary surgical intervention. Surgery is not without risk and should not be undertaken when it is needed. If you suffer from Crohn’s disease surgery should be generally reserved for the most serious complications such as intestinal obstructions, fistulas, or abscesses. An accurate diagnosis will help prevent unnecessary surgery.
- The Management of Chronic Condition: Crohn’s disease is an ongoing inflammatory condition that requires continuous treatment. A prompt diagnosis and proper treatment will help patients keep a high level of living, manage symptoms, and decrease the chance of developing complications. The inability to distinguish between two types of conditions can delay the commencement of proper therapy for patients suffering from Crohn’s disease.
- Preventing complications: Appendicitis and Crohn’s disease may cause severe complications, however, these complications are distinct. For instance, untreated appendicitis may result in peritonitis and a ruptured appendix, while Crohn’s disease may cause fistulas, intestinal strictures, as well as an increased chance of developing colon cancer. The identification of the appropriate condition ensures you receive proper treatment and monitoring to avoid certain complications.
- Health and Well-being of Patients: A misdiagnosis could cause anxiety and stress for patients. Patients suffering from chronic illnesses such as Crohn’s disease require support as well as education and an extended treatment plan. Making the mistake of telling a patient they’re suffering from appendicitis when they aren’t could cause anxiety and confusion.
- Healthcare costs: A precise diagnosis is vital to avoid unnecessary medical costs. The wrong treatment can cause further tests, treatments, and hospitalizations, putting a greater cost on patients and healthcare systems.
The distinction between appendicitis as well as Crohn’s disease is vital for ensuring that sufferers receive proper treatment and medical care quickly. It has a significant impact on the outcome of patients, their quality of life, and the quality of healthcare utilization. So, healthcare professionals need to depend on the right diagnostic tools to identify the two conditions with precision.
Appendicitis and Crohn’s Disease in the comparison chart
Here’s a comparison chart highlighting the key differences between appendicitis and Crohn’s disease:
| Characteristic | Appendicitis | Crohn’s Disease |
| Definition | Inflammation of the appendix, a small pouch attached to the large intestine | Chronic inflammatory bowel disease affecting any part of the digestive tract |
| Common Location of Pain | Right lower abdomen | Variable; often in the lower abdomen, but location varies |
| Onset of Symptoms | Sudden and severe | Gradual and chronic |
| Pain Characteristics | Sharp, intense, localized pain | Crampy, intermittent, diffuse pain |
| Associated Symptoms | – Nausea and vomiting – Loss of appetite – Fever – Swelling in the abdomen | – Diarrhea – Blood in stool – Abdominal cramps – Weight loss – Fatigue |
| Causes | Blockage of the appendix (often by fecal matter) or infection | Complex, involving immune system response, genetics, and environmental factors |
| Diagnostic Tests | – Physical examination – Blood tests – Imaging (CT scan, ultrasound) | – Colonoscopy – Blood tests – MRI or CT scan – Stool sample – Biopsy |
| Treatment | Surgical removal of the appendix (appendectomy) | Medications (anti-inflammatory drugs, immunosuppressants), dietary changes; surgery in severe cases |
| Chronic vs. Acute | An acute condition requiring immediate treatment | A chronic condition requiring long-term management |
| Complications | – Ruptured appendix – Abscess – Peritonitis (if not treated promptly) | – Fistulas – Bowel strictures – Malnutrition – Ulcers – Increased risk of colon cancer |
| Prevention | No specific prevention measures | No surefire prevention; managing triggers and maintaining overall health |
| Age of Onset | Most common in young adults and teenagers | Typically diagnosed in late adolescence or early adulthood, but can occur at any age |
| Surgery | Urgent appendectomy is often necessary | Surgery is reserved for severe complications or when medications are ineffective |
| Lifestyle Changes | Not usually a factor | Dietary and lifestyle adjustments may be required |
| Prognosis | Favorable with prompt treatment | Chronic condition with variable outcomes |
| Emotional Impact | Acute, often stressful diagnosis | Chronic, long-term impact on quality of life |
| Healthcare Costs | This may involve immediate surgical costs | Long-term medical management may lead to ongoing expenses |
| Management Approach | Emergency medical/surgical intervention | Long-term medical management and monitoring |

This comparison chart provides a clear overview of the differences between appendicitis and Crohn’s disease in terms of their symptoms, causes, diagnostic methods, treatment, and impact on patients’ lives. It can be a helpful reference for healthcare professionals and patients alike.
Symptoms of Appendicitis and Crohn’s Disease
These are the most common signs of appendicitis and Crohn’s disease.
Appendicitis Symptoms:
- Abdominal pain: The hallmark symptom of appendicitis is the sudden extreme pain that normally begins at the belly button, and later goes to the lower right of your abdomen. The pain can become more severe throughout.
- Vomiting and nausea: Many individuals with appendicitis suffer from nausea and can vomit because of the discomfort and pain.
- Loss of appetite: People with appendicitis frequently lose appetite, and they may not want to eat.
- fever: A low-grade fever could develop due to inflammation.
- Abdomen swelling: The abdomen may be tender and swollen at the point of contact, mainly around the right lower quadrant.
- Inability to pass gas or have a Bowel Movement: Constipation or difficulty getting gas out can be a sign of appendicitis.
- Painful Urination: In certain instances, people suffering from appendicitis can suffer from pain or discomfort when the urination process.
Crohn’s Disease Symptoms:
- Diarrhea: Chronic or intermittent diarrhea is a typical sign of Crohn’s condition. The stool can be watery and loose.
- abdominal Cramps and Pain: Patients with Crohn’s disease typically experience abdominal pain and cramps that may vary in intensity and location. The pain could be more prominent in the lower quadrant of the right.
- Stool Blood: Blood in the stool may be the result of ulcers and inflammation in the digestive tract. This is a characteristic of Crohn’s disease.
- Weight Loss: Chronic inflammation and a lack of nutrients may cause the loss of weight, even when appetite levels are normal.
- Fatigue: The chronic inflammation of the intestines and diarrhea may result in fatigue and a general feeling of weakness.
- The Fever Certain people with Crohn’s disease can experience fever, notably during flare-ups of the disease.
- Reduced Appetite: Loss of appetite may be a sign of Crohn’s disease and contribute to weight gain.
- Joint Pain: Joint pain caused by inflammation is known as arthralgia. It can be experienced by people suffering from Crohn’s disease.
- Skin Issues: Skin issues like ulcers and rashes could be a result of an extra-intestinal manifestation of Crohn’s disease.
- Eye Inflammation: Eye inflammation (uveitis) is a possibility in certain people suffering from Crohn’s disease.
It is important to remember that, while there are a few common symptoms, the main differences between the two are the type of symptoms (sudden or severe with appendicitis in contrast.
chronic, crampy Crohn’s Disease) as well as the site of the pain and the long-term nature of Crohn’s disease as opposed to an acute form of appendicitis. Should you, or anyone you know have symptoms that could be indicative of either it is crucial to get a medical exam as soon as possible to determine the correct diagnosis and proper treatment.
Causes & Risk Factors of Appendicitis and Crohn’s Disease
Below are the risk factors and causes of Crohn’s disease and appendicitis:
Causes and Risk Factors of Appendicitis:
- Obstruction Appendicitis is the most common cause. can be the blockage of the appendix. The obstruction could be because of factors like:
-
- The stool or stool can block the appendix’s opening.
- An increase in lymphoid tissue within the appendix could result from an infection.
- Tumors or foreign bodies can block the appendix.
- An infection: In some cases, an infection of the appendix could cause inflammation. Infections with bacteria can cause the appendix to swell and then become inflamed.
- Age: Appendicitis may occur at any time, however, it is more common among people aged between 10 and 30.
- Genre: Males are slightly more likely than females to get appendicitis.
- family history: There may be an element of genetics, for instance, people with a history of the family of appendicitis could be at a higher risk.
Causes and Risk Factors of Crohn’s Disease:
- The Immune System Response: Crohn’s Disease is thought to result from an autoimmune condition in which your body’s immune system attacks the digestive tract. The precise trigger behind this immune response is not known.
- Genetics: The presence of a Crohn’s Disease-related family lineage can increase the chance of developing. Certain genetic markers have been linked to a higher risk of developing the disease.
- Environmental Factors: Factors in the environment like smoking, diet, and exposure to certain infections could contribute to the development or worsening of the symptoms of Crohn’s condition. Smoking, particularly is a major risk factor for the development of Crohn’s.
- Age: Though Crohn’s disease can affect anyone at any age, however, it usually develops within the age range between 15 to 35.
- Origin: Crohn’s disease is more common in certain ethnic groups, like Ashkenazi Jews.
- Geographic location: It appears that the prevalence of the disease Crohn’s is greater in industrialized nations which suggests a possible connection with modern life as well as environmental factors.
- The diet: A few dietary triggers like a high consumption of processed foods and trans fats as well as the absence of fiber in your diet can increase the risk of developing Crohn’s disease.
- Utilization of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): In the long run, using NSAIDs like ibuprofen may increase the likelihood of developing Crohn’s Disease or aggravating existing symptoms.
It is important to remember that although these elements are linked to an increased likelihood of developing these illnesses they don’t ensure that a person will be diagnosed with Crohn’s or appendicitis disease.
The causes for these diseases may be complicated interactions between environmental, genetic, and immune system-related factors. If you’re concerned regarding your risk of developing any of these conditions or have similar symptoms, it’s recommended to seek out a medical professional to get a proper assessment and advice.
Diagnostic Procedures
The diagnostic procedure for appendicitis and Crohn’s disease may require numerous medical tests and tests to determine the presence of these conditions.
Here are the most common tests for each:
Diagnostic Procedures for Appendicitis:
- Physical Exam: The healthcare provider will conduct an extensive physical exam that focuses on the abdomen. They can employ techniques like the rebound tenderness test in which they press gently onto the abdomen’s lower part, and then let it go to evaluate the response to pain.
- Testing for Blood: Blood tests, such as a complete blood count (CBC) and inflammation markers such as C-reactive protein (CRP) as well as white blood cells, will help you identify the indications of inflammation and infection.
- Urinalysis: The urinalysis test can be performed to rule out urinary tract issues that could be similar to symptoms of appendicitis.
- imaging: Imaging tests are frequently used to confirm the diagnosis:
-
- Ultrasound Non-invasive, non-invasive image technology can see the appendix and look for any signs of inflammation or blockage.
- CT Scans: A computed tomography (CT) scan of the pelvis and abdomen can give detailed images, which aid in the identification of appendicitis as well as its severity.
Diagnostic Procedures for Crohn’s Disease:
- colonoscopy: The colonoscopy procedure is a crucial test for diagnosing Crohn’s disease. In this procedure, the flexible tube that has a camera is introduced through the rectum into the colon, sometimes into the small intestine. The doctor can look at the digestive tract and collect tissue samples (biopsies) to analyze.
- Testing for Blood: Blood tests may detect the signs of anemia, inflammation, and nutritional deficiencies that can be associated with Crohn’s disease. These tests could be used to determine CRP levels, erythrocyte segregation rate (ESR), and total blood count (CBC).
- MRI as well as CT scan: Imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans provide precise photographs of the digestive tract. These scans aid in determining the degree of the inflammation, and its complications, and pinpoint the exact location of affected regions.
- Stomach Samples: A stool sample can be examined to look for indications of bleeding, infection, or inflammation of your digestive tract.
- Capsule Endoscopy: In certain situations, a patient might take a capsule that contains cameras that take pictures while it is traveling through the digestive tract. This provides pictures of small intestinal tracts which cannot be viewed through conventional colonoscopy.
- Double-Balloon Endoscopy: This procedure is specialized and can be utilized to look at as well as biopsy small intestines where conventional methods aren’t sufficient.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP may be performed to assess the bile ducts and pancreas if there is suspicion of complications in these areas.
These diagnostic techniques aid healthcare professionals in identifying Crohn’s disease and appendicitis. They also give valuable information to aid in the treatment plan. A precise diagnosis is essential to make sure that the patients get the right care that is tailored to their specific health condition.
Treatment Options of Appendicitis and Crohn’s Disease
Appendicitis treatment options and Crohn’s disease vary significantly because of the unique nature of these conditions.
Here’s a summary of the treatment options for each of the following:
Treatment Options for Appendicitis:
- Surgery Removal (Appendectomy): The principal treatment for appendicitis involves surgical removal of the appendix that is inflamed. The procedure is known as an appendectomy. There are two ways to perform it:
-
- Laparoscopic Appendectomy: This minimally invasive method involves a small cut with a video camera along with special instruments to eliminate the appendix. The result is typically quicker recovery, with less scarring.
- The Open Appendectomy: In cases when laparoscopy isn’t feasible or if complications occur during the procedure, an open appendectomy can be done using an abdominal incision larger than.
- Antibiotics: Sometimes it is possible to administer antibiotics before surgery in cases where the diagnosis is not clear or there is a delay in the procedure. Surgery is still the main option for treating appendicitis.
Treatment Options for Crohn’s Disease:
- Medicines: Treatment for Crohn’s disease typically involves medication to treat symptoms, decrease inflammation, and keep the disease in a state of remission. Commonly used medications include:
-
- Anti-Inflammatory Drugs: They comprise corticosteroids (e.g. prednisone) as well as 5-aminosalicylates (e.g. mesalamine, for instance) to lessen inflammation in flare-ups.
- Immunosuppressants: The use of medicines such as azathioprine methotrexate, or mercaptopurine can assist in suppressing the immune system’s response to inflammation.
- Biologics: The newer drugs like infliximab or adalimumab are targeted at specific immune system proteins to reduce inflammation.
- Anti-Diarrheal Drugs: Medications like loperamide may help manage diarrhea.
- Pain Relief: Over-the-counter or prescription pain medication can ease abdominal pain.
- Lifestyle and Dietary changes: Changes in diet and lifestyle, such as a low-residue dietary plan in times of flare-ups, or avoiding trigger foods can aid in managing symptoms.
- Nutritional Assistance: In cases of excessive weight loss or malnutrition the use of nutritional supplements, or total parenteral nourishment (TPN) could be recommended to ensure that you get the necessary nutrients.
- The term “surgery” refers to: It is a procedure that can be considered in cases where medication alone isn’t effective, or if complications develop including fistulas or strictures, as well as abscesses. Surgery options include:
-
- Strictureplasty: Utilized to broaden sections of the intestine that have been narrowed.
- Resection: The removal of the damaged section from the digestive tract, and reconnecting healthy portions.
- A colostomy, or Ileostomy: The abdomen is opened temporarily or permanently to allow for the removal of waste if needed.
- Monitoring: Regular check-ups and continuous monitoring are essential to evaluate the severity of illness, adjust medication, and deal with any issues or changes to the health.
The treatment plan for Crohn’s disease can be tailored to the patient’s particular symptoms locations, severity, and location. It usually involves a combination of lifestyle changes, medications and, in certain instances, surgery to control symptoms and sustain an ongoing recovery. Appendicitis on the other of the other hand, generally requires surgical intervention immediately.
Complications of Appendicitis and Crohn’s Disease
Appendicitis as well as Crohn’s disease can result in a myriad of complications, and some may be severe and require medical attention.
Below are some possible issues that can arise with each of the conditions:
Complications of Appendicitis:
- appendix that has ruptured (Perforation): If appendicitis isn’t treated quickly the inflamed appendix may tear or rupture, which can release affected material to the stomach cavity. This could lead to a more severe infection, called peritonitis.
- Peritonitis: The condition is serious swelling of the peritoneum, which is the abdominal cavity’s lining. It is a common cause of inflammation and can be an emergency medical situation.
- Abscess Development: Sometimes, instead of breaking, the appendix could develop an abscess which is an incision of pus. Abscesses need drainage and are treated using antibiotics.
- Small Bowel Obstruction: In rare cases, the loop in the small intestine may be blocked because of adhesions and inflammation caused by appendicitis.
- Sepsis When it is severe the infection that is associated with appendicitis could result in sepsis. This is a life-threatening illness in which the body’s reaction to infection causes extensive inflammation.
Complications of Crohn’s Disease:
- Intestinal Complications:
-
- Strictures: Inflammation in Crohn’s Disease can obstruct the digestive tract, which causes obstructions in the bowel or blockages.
- Fistulas: abnormal connections or tunnels could form between different components within the digestive tract as well as connecting the intestinal tract with the other organs.
- Abscesses: Pus pockets may develop in the abdominal cavity, or within the intestinal wall.
- Nutritional malnutrition: Inflammation chronic in Crohn’s condition can hinder the digestion of nutrition in food, resulting in a deficiency in nutrition and vitamins and minerals.
- Ulcers Chronic inflammation may result in open sores or ulcers on the lining of the digestive tract.
- Perianal Complications Crohn’s disease may cause issues in the anal region such as anal fissures abscesses, as well as fistulas.
- Colon Cancer: Patients with chronic Crohn’s disease that affects the colon have an increased chance of developing cancer of the colon. Regular screening and follow-up are vital.
- Extraintestinal Signs: Crohn’s disease may cause organs and systems to be affected outside that of the digestive tract which can lead to complications like joint inflammation (arthritis) skin issues eye inflammation (uveitis) and liver problems.
- Side Effects of Medication: Certain medications prescribed to treat Crohn’s disease may cause side consequences, such as an increased risk of liver disease, infection, and loss of bone density.
- Quality of Life Impacts: The chronic nature of Crohn’s disease, together with its complications and symptoms can hurt an individual’s mental health as well as their overall quality of life.
Patients with any medical health condition need to collaborate closely with their healthcare providers to monitor their conditions and deal with any issues that might occur. A prompt diagnosis and early intervention could aid in minimizing the impact of these issues and enhance the long-term outcomes for patients.
Prevention and Management
Strategies for prevention and management of Crohn’s disease and appendicitis differ because of their distinct origins and characteristics. This is how each is treated:
Prevention and Management of Appendicitis:
Prevention:
- Appendicitis is usually regarded as an illness that is not preventable since its cause is not recognized. However, general hygiene practices can aid in maintaining general abdominal health, like an appropriate diet, regular exercising, and ensuring good hygiene to lower the risk of infection.
Management:
- Operation (Appendectomy): The most common treatment for appendicitis is surgery to remove the appendix that is inflamed. The procedure is carried out urgently to avoid complications such as rupture.
- Antibiotics: Sometimes it is possible to administer antibiotics before surgery to prevent the infection, particularly if urgent surgery is not feasible.
- Rehabilitation: After surgery, the patient usually recovers in an inpatient hospital for a couple of days, and then they continue to recuperate at home. Following-up treatment from a doctor is crucial.
Prevention and Management of Crohn’s Disease:
Prevention:
Crohn’s disease does not have an identified cure that is 100% certain, however, certain lifestyle changes can lower the risk of flare-ups and complications
-
- The diet: A balanced, low-fat diet with minimal processing and high in vegetables, fruits, and fiber could help with the symptoms.
- Nicotine: If you smoke smoking cigarettes, stopping can reduce the chance of developing Crohn’s or aggravating existing symptoms.
- Hydration: Drinking enough water is vital to avoid dehydration, especially during episodes of diarrhea.
- The Management of Stress: Chronic stress can worsen symptoms, and stress-reduction strategies like relaxation, exercises, and counseling could assist.
Management:
- Medicines: Medications are a fundamental element in the management of Crohn’s disease and are designed to decrease inflammation, ease symptoms, and ensure the state of remission. The medications include anti-inflammatory medicines and immunosuppressants, as well as biologics and anti-diarrheal medicines.
- Dietary Changes: Modifications to your diet may assist in managing symptoms. Some people find relief through avoiding trigger foods or adhering to specific diets such as one that is low in residues during flare-ups. A consultation with an experienced dietitian may prove beneficial.
- Supplemental Nutritional Assistance: Nutritional supplements or total parenteral nutrition (TPN) might be necessary in the event of malnutrition and/or significant loss of weight.
- surgery: It is of course considered as an option when medication is not effective or complications such as strictures fistulas, or abscesses are present. Surgery options include strictureplasty, removal, and the construction of the ostomy.
- Continuous Monitoring: regular checkups and visits with an experienced healthcare professional are essential for assessing the severity of disease adjusting medications and spotting any changes or complications in the health.
- Lifestyle Management: Maintaining an active lifestyle, which includes regular exercise and stress-reducing can ease the symptoms and boost overall well-being.
- Supportive Care: Groups of support and counseling can offer support for emotional issues and aid individuals in dealing with the difficulties of being a patient with a chronic illness such as Crohn’s disease.
The treatment for Crohn’s disease tends to be customized to each person’s symptoms and the location of the disease as well as the severity. It is usually a mix of medication, diet adjustments, and lifestyle changes. Patients must work closely with healthcare professionals to design and implement a customized treatment program.
Conclusion
Crohn’s disease and appendicitis both are medically distinct and have different symptoms, causes diagnosis procedures, and treatment methods. A timely diagnosis, proper management, and regular surveillance are crucial to the overall health of those suffering from these ailments. Knowing the distinctions between them is essential for a precise diagnosis and efficient treatment.
References books
Here are some reference books and medical textbooks that provide comprehensive information on appendicitis and Crohn’s disease:
Books on Appendicitis:
- “Acute Appendicitis: Standard Treatment or Laparoscopic Surgery?” by V. Papadopoulos, C. Sgourakis, and K. Diener.
- “Appendicitis: The Etiology, Hygienic, and Dietetic Treatment” by John H. Tilden, M.D.
- “Appendicitis: The Cause, Symptoms, and Treatment of the Disease” by A. T. Thomson, M.D.
- “Acute Appendicitis: A Clinical Casebook” by Ronny Cohen, M.D., and Jeffrey L. Ponsky, M.D.
Books on Crohn’s Disease:
- “Inflammatory Bowel Disease: Diagnosis and Therapeutics” by Russell D. Cohen, M.D., and Bruce E. Sands, M.D.
- “Crohn’s Disease and Ulcerative Colitis: Everything You Need to Know” by Fred Saibil, M.D., and Joseph Weinstein, M.D.
- “Oxford Textbook of Inflammatory Bowel Disease” edited by Daniel C. Baumgart, M.D., and Simon P.L. Travis, M.D.
- “Crohn’s Disease and Ulcerative Colitis: From Epidemiology and Immunobiology to a Rational Diagnostic and Therapeutic Approach” by Daniel C. Baumgart, M.D., and Walter F. Fazio, M.D.
