An overview of the astrocytoma Glioblastoma
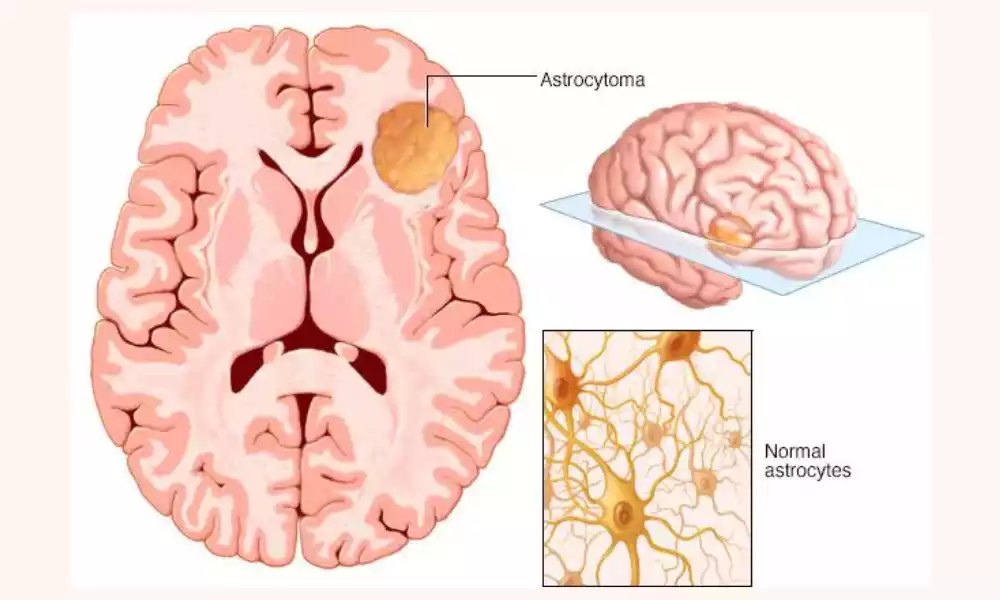
Astrocytoma and Glioblastoma are two kinds of brain tumors that arise from different kinds of glial cells found in the brain. Astrocytomas are cancers that arise from astrocytes. They are a form of glial cell that has a star shape. It gives support and nutrition to brain neurons.
Glioblastomas On the contrary are the most prevalent and invasive kind of brain tumor that originates from the primary brain and originates from glial cells, also known as the astrocytes or oligodendrocytes.
Astrocytomas can be classified into four types according to their severity and the likelihood to develop or recur. Grade I astrocytomas are the most benign, while grade IV astrocytomas or glioblastomas are the most cancerous and have a poor prognosis. Glioblastomas are extremely infiltrating and can rapidly spread throughout the brain which makes them challenging to cure.
Important differences between them
The distinction between astrocytoma and glioblastoma is crucial for a variety of reasons. First, the prognosis and treatments for these two kinds of brain tumors differ dramatically. Glioblastomas are more challenging and challenging to treat while astrocytomas of lower grade are more manageable.
Thus, a precise diagnosis and a proper diagnosis of the cancer are vital to designing a proper treatment plan that will maximize patient outcomes.
The causes and risks for astrocytoma and glioblastoma are different, and this could impact the prevention actions. Through understanding these differences, researchers can identify possible risk factors and formulate strategies to prevent them.
Finally, knowing the difference between astrocytoma versus glioblastoma may aid research efforts that aim to improve treatments and create new treatments.
Understanding the molecular and cellular aspects of the tumors could aid in identifying possible therapeutic targets that improve the survival rate and outcomes for patients.
Definition and Pathology
Astrocytoma and glioblastoma are two kinds of brain tumors that originate from various types of glial cells that reside in the brain.
Astrocytoma: It is a cancer that develops from astrocytes. They are a form of glial cells that have a star shape. They offer support and nutrition to brain neurons. These tumors can form any place in the brain however, they are most often found in the cerebrum which is the most extensive part of the brain.
Astrocytomas can be classified into four categories, based on the World Health Organization (WHO) classification system. Astrocytomas that are grade I, as well as Grade II, are regarded as low-grade tumors. Grade III and Grade IV tumors can be considered high-grade tumors. Astrocytomas of grade IV are called Glioblastomas.
Glioblastoma: Glioblastoma is the most frequent and the most aggressive type of brain tumor that is primary which accounts for 15 percent of brain tumors. Glioblastomas may arise from the astrocytes or the oligodendrocytes which are another kind of glial cell. They are distinguished through their rapid development rate and their ability to invade brain tissues.
Glioblastomas have been classified as tumors of grade IV by the WHO classification system. They are extremely invasive and can spread quickly throughout the brain which makes it difficult for them to be treated.
Glioblastomas are also distinguished by their high level of cell heterogeneity. This means that tumor cells could be genetically diverse and have distinct characteristics, which makes them unresponsive to treatment.
What exactly is Astrocytoma?
Astrocytoma is one type of cancer that develops in the brain or the spinal cord. It is usually a less-grade brain tumor. It is caused by the astrocytes that support neurons within the brain. The signs and symptoms of astrocytoma depend on the site and the extent of the tumor. Astrocytoma found in the brain may result in headaches, seizures, and nausea.
However, Astrocytoma that develops within the spinal cord may result in weakness and impairment of the region affected by cancer. Astrocytoma could be a brain tumor that grows slowly (diffuse Astrocytoma) or an aggressive cancer (anaplastic astrocytoma).
The degree of Astrocytoma is the determinant of its prognosis and treatment options. Sometimes, astrocytoma may result in a more severe brain cancer, known as glioblastoma.
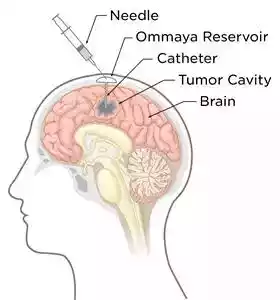
Astrocytoma diagnosis is made by neurologic examinations and diagnostic tests (MRI, CT scan, and PET) as well as biopsies. There are various types of treatment strategies used to treat astrocytoma. A brain surgeon can eliminate as much Astrocytoma as possible by surgery.
Radiation therapy utilizes high-energy beams, such as protons or X-rays to destroy brain cancers such as Astrocytoma. In addition, chemotherapy drugs, such as temozolomide is used to treat astrocytoma.
What exactly is Glioblastoma?
Glioblastoma is a more advanced brain cancer that develops in the spinal cord and brain. This is by far the most severe kind of cancer that occurs in the brain. The exact cause of glioblastoma remains unknown.
However, there are a variety of risks, such as genetic diseases like neurofibromatosis Li-Fraumeni syndrome tuberous sclerosis Turcot syndrome, and prior radiation treatment.
Around five percent of glioblastoma sufferers develop due to low-grade astrocytoma. Other risks include smoking or exposure to pesticide workers in petroleum refining or rubber manufacturing. In addition, glioblastoma is been linked to diseases caused by viruses like SV40 as well as HHV-6 and Cytomegalovirus.

Glioblastoma is classified into the categories of primary (IDH wild-type) and secondary Glioblastoma (IDH mutation). The signs of glioblastoma could include mood changes, headaches nausea, stroke symptoms, and insanity. The diagnosis is usually made through CT images, MRIs as well as tissue biopsies.
Additionally, treatment options for glioblastoma include radiation therapy, surgery chemotherapy (temozolomide), and specific drug therapy (bevacizumab) as well as the tumor treatment field (TTF) treatment.
differentiates In Astrocytoma and Glioblastoma
Astrocytoma and glioblastoma are two kinds of brain tumors that result from different kinds of glial cells that reside in the brain. Although they share some commonalities, they differ in some significant ways.
- Grade One of the most important: Grade One of the most important distinctions between glioblastoma and astrocytoma are their degrees. Astrocytomas are classified into four grades depending on the severity of their tumors and their potential to develop or be recurrence-prone.
- Astrocytomas of grade I or II are regarded as low-grade tumors: Grade III and Grade IV astrocytomas are regarded as high-grade tumors. Glioblastomas are tumors of grade IV and are considered to be the most malignant and aggressive form of tumor in the brain.
- Aggressiveness: A key distinction between glioblastoma versus astrocytoma is their aggressiveness. Glioblastomas are very aggressive and they can quickly spread throughout the brain making them extremely difficult to manage. Astrocytomas on the other side, are typically less invasive, and the lower grade astrocytomas are often easier to treat.
- Prognosis: The outlook for glioblastoma and astrocytoma could differ quite significantly. Glioblastomas have an extremely poor prognosis with an average survival of 15 months. Astrocytomas with lower grade may be more likely to survive and some patients can live for years with proper treatment.
- Treatment: Options for the treatment of Astrocytoma and Glioblastoma are different by the degree and the location where the cancer is located. Treatment options include radiation therapy, surgery, and chemotherapy are the most common treatment options to treat these cancers.
However, glioblastomas can be unresponsive to treatment, and novel treatments are required to improve the outcomes for patients suffering from this cancerous tumor.
The distinct characteristics of the two types of glioblastoma illustrate the importance of an accurate diagnosis and the proper diagnosis of various brain tumors. Understanding the specific characteristics of these tumors can assist healthcare professionals in developing effective treatment plans and improving the outcomes of patients.
Causes and risk factors
The precise causes of astrocytoma or glioblastoma tumors are not completely identified. However, scientists have identified various risk factors that could increase the chance of developing these cancers.
- Age: The likelihood of developing glioblastoma or astrocytoma increases as you the advancing years. Glioblastomas tend to be more prevalent among adults between 45 and 70 years, whereas Astrocytomas of low grade can be found in young people and children.
- Genetics: Genetic mutations inherited from the parents, for example, modifications to the TP53 gene or the NF1 gene, could increase the chance of developing brain tumors.
- Radiation exposure: Experiments with Ionizing radiation, for example, radiation treatment for cancer, increase the chance of developing tumors in the brain, especially gliomas.
- Environmental factors: Exposure to certain chemicals, for example, formaldehyde and vinyl chloride, can increase the risk of developing brain tumors.
- Family history: A history of family members of brain tumors can increase the chance of developing tumors.
- Inhibition of immune systems: People who have compromised immune systems, for instance, people with HIV or those who have had organ transplants, could be at an increased chance of developing brain tumors.
It is crucial to remember that a lot of people who have these risk factors are unlikely to be diagnosed with a brain tumor and a lot of people who do not have these risk factors could have brain tumors. The reasons for the tumors are complicated and many factors could be at play in their
Life Expectancy and Prognosis
The prognosis and the survival rates for glioblastoma or astrocytoma could vary greatly based on the degree and site of the tumor and also the health and age that the person.
Astrocytoma: The outlook for astrocytoma may range between good and poor depending on the severity of the tumor. Astrocytomas that are grade I as well as Grade II are regarded as low-grade tumors and could be more likely to survive and some patients can live for a long time with the right treatment.
Astrocytomas: Astrocytomas that are graded III, as well as Grade IV, have been classified as high-grade tumors with less of a chance of survival, with the median survival of 2 to 3 years for astrocytomas of grade III or less than 2 years with grade IV Astrocytomas.
Glioblastoma: Glioblastoma has an extremely poor prognosis, having a median survival of approximately 15 months when treated appropriately. However, certain patients suffering from Glioblastoma can live for a longer time by undergoing more aggressive treatment strategies like radiation therapy, surgery, and chemotherapy.
In general, the outlook for brain tumors is difficult to determine because every patient’s experience is unique. The size and location of the tumor along with the overall health and age of the patient influence the prognosis as well as survival rates.
The treatment options can also differ by the characteristics of the tumor as well as the objectives of the patient and the healthcare team. Families and patients must cooperate with healthcare professionals to design a personalized treatment plan and monitor the effectiveness of treatment as time passes.
Conclusion
Astrocytoma and glioblastoma are the two types of brain tumors that may differ significantly in severity, aggressiveness, prognosis, as well as treatment options. Both tumors originate from glial cells within the brain and can be difficult to treat, accurate diagnosis and the right treatment are crucial to improve the outcomes of patients.
The distinct characteristics of these tumors emphasize the importance of continuing study into the genetics and biology of brain tumors as well as the creation of new treatments and strategies to improve the survival rate and the quality of life for those suffering from these difficult conditions.