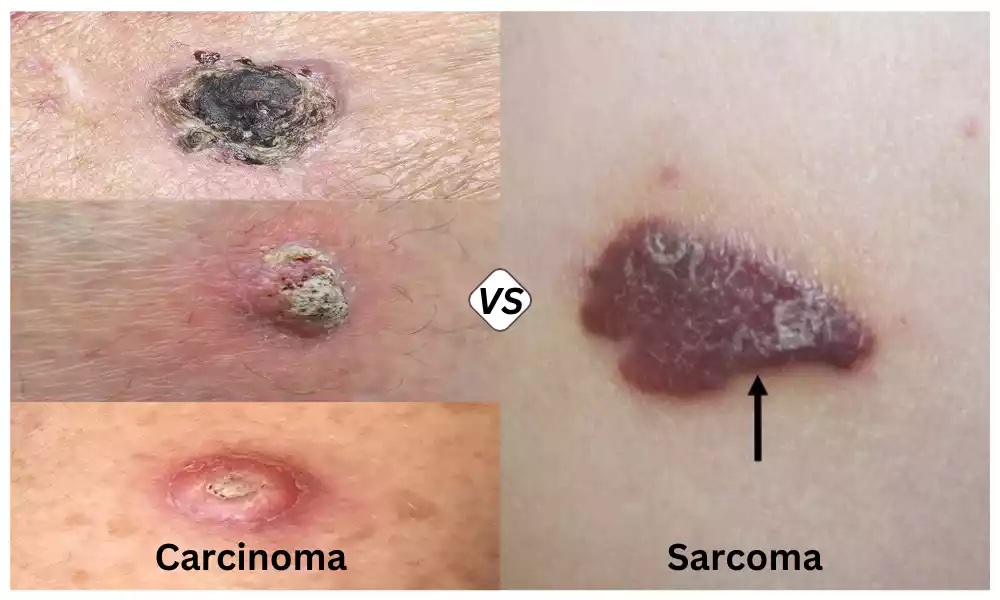
Carcinoma and Sarcoma, Both carcinoma (epithelial cancer) and sarcoma (connective tissue cancer) are primary types of cancer that arise from different tissues in the body. Carcinoma is a cancer that develops from epithelial tissue, while sarcoma occurs in connective tissues.
These differences have a profound impact on their behavior, diagnosis, and treatment. This overview will highlight the unique characteristics of sarcoma and carcinoma in oncology.
Definition of Carcinoma
Carcinoma, a form of cancer, is a type that develops in the epithelial tissue of the body. The epithelial tissue is found in the skin and mucous membranes as well as the linings of organs and glands.

The uncontrolled proliferation and growth of abnormal cells within this epithelial tissue is what defines a cancer. They can form solid tumors, and they can invade nearby tissues. In some cases, metastasis may spread to distant areas of the body.
The most common form of cancer, carcinomas, can affect many organs including the skin, lungs, prostate, colon, and breast. The treatment and prognosis of carcinoma are dependent on the location, grade, and stage.
Definition of Sarcoma
Sarcomas are cancers that originate in connective tissues of the body, such as muscles, tendons, and cartilage. They can also affect nerves and blood vessels. Sarcomas are different from carcinomas which develop in epithelial tissue.
They form in the mesenchymal connective tissues that support the body and link the various parts. Sarcomas, which are often tumors, are caused by uncontrolled growth in connective tissue.

Sarcomas are found in many parts of the human body. They can be classified according to the type of connective tissue affected. Subtypes of sarcomas can include, among others, osteosarcomas (affecting bone tissue), liposarcomas (arising from fat tissue), and leiomyosarcomas (developing within smooth muscle tissue).
Sarcomas can invade adjacent tissues, and in some cases spread to other parts. Sarcomas are diagnosed, treated, and given a prognosis based on factors like the subtype, the location, the stage, and the grade of cancer. Sarcomas, while less common than carcinomas, are a serious category of cancers with unique challenges and characteristics.
Key Differences of Carcinoma and Sarcoma
There are two main differences between Carcinoma (carcinoma) and Sarcoma:
- Tissue Origin:
- Carcinoma: This cancer arises from epithelial tissue, including the skin, mucous tissues, and the linings in organs and glands.
- Sarcoma: This cancer develops in connective tissue, including bones, muscles and tendons. It can also affect nerves and blood vessels.
- Common Locations:
- Carcinoma is a cancerous growth that occurs in epithelial-lined organs such as the skin, lungs, prostate, breast, and colon.
- Sarcomas: These are cancerous tumors that develop in the connective tissue of the body. They can affect soft tissues, muscles, or bones.
- Tumor Characteristics:
- Carcinoma: Solid tumors that often appear glandular under the microscope.
- Sarcomas: These tumors develop in connective tissue and vary in appearance depending on their subtype.
- Metastatic Potential:
- Carcinoma tends to spread more often to distant organs and regional lymph nodes than sarcoma.
- Sarcoma: It is less likely to spread than carcinoma, but it can still affect other parts of the body.
- Histological Features:
- Carcinoma: Histologically speaking, carcinomas usually display features like glandular formations (in squamous-cell carcinomas) or keratinization. These characteristics reflect their epithelial origin.
- Sarcomas: The histological characteristics vary depending on the subtype. They can include round or spindle-shaped cell patterns, as well as other distinct patterns.
- Incidence and prevalence:
- Carcinoma is the most common cancer worldwide.
- Sarcomas: These are less common and account for a lower percentage of cancer diagnoses.
- Treatment Options:
- Depending on the type of cancer and its stage, treatment options may include radiation therapy, chemotherapy, and targeted therapy.
- Sarcoma Treatment usually involves surgery to remove the tumor and radiation therapy or chemotherapy. In some cases, it may also include immunotherapy.
- Prognosis:
- Carcinoma: The prognosis can vary widely, depending on its type, location and stage. It may be highly curable or very aggressive.
- Sarcoma: The prognosis depends on various factors, including the subtype, stage, and location. Some sarcomas have relatively good outcomes, while others can be more difficult to treat.
Understanding the key differences between carcinoma and sarcoma is crucial for accurate diagnosis and treatment planning. It also helps predict outcomes.
Similarities
Although carcinoma and sarcoma have many differences between them, they share some similarities.
- Both are forms of cancer:
- Both cancerous tumors (carcinoma and Sarcoma) are caused by the uncontrolled growth of abnormal cells in the body.
- Local Invasion Potential:
- As they grow, both carcinoma and sarcoma may invade nearby tissues and structures and cause damage.
- Treatment Modalities:
- Both cancer types can be treated using a combination of methods, such as surgery, radiotherapy, chemotherapy, and, in some cases targeted therapy or immune therapy, depending on specific tumor characteristics and stage of disease.
- Symptoms:
- Both cancers can cause similar symptoms. These include pain, swelling, a mass or lump at the site of the tumor, and in some cases symptoms relating to organ dysfunction, if the tumor has affected critical structures.
- Diagnostic Methods:
- Both carcinoma and sarcoma are diagnosed and staged using diagnostic techniques such as imaging (e.g. CT scans MRIs, or PET scans), biopsy, and histopathological analysis.
- Risk Factors:
- Although risk factors vary depending on the subtype, certain general factors such as genetic predisposition and exposure to carcinogens can contribute to both carcinoma and Sarcoma.
- Need for early detection and intervention:
- Early diagnosis and intervention are critical to better treatment outcomes for both carcinoma and Sarcoma.
- Metastasis Potential:
- Both cancers have the potential for metastasis, but carcinomas are more likely to do so than sarcomas.
- Multidisciplinary Care:
- Multidisciplinary teams of healthcare professionals are often required to treat patients with carcinoma or sarcoma, including oncologists and surgeons as well as radiologists and pathologists.
While there are similarities between the two, it’s important to remember that despite their similarities, they are different entities that require specific treatment and diagnostic strategies.
How cancers and sarcomas are spread
A process known as metastasis can cause cancer, such as sarcomas and carcinomas. Metastasis refers to the spreading of cancer cells away from the primary tumor and into other parts of the human body. Different types of cancer can have different mechanisms for spreading cancer cells.
This is a general overview of how cancers can spread, including sarcomas:
- Local invasion: Cancerous cells usually begin their journey by invading tissues and structures nearby. Cancer cells can invade nearby structures or organs when they break through tissue barriers. Local invasion can cause symptoms and complications in the affected area.
- The lymphatic system: Many cancers (especially carcinomas) can spread through the lymphatic system to nearby lymph nodes. The lymph nodes are tiny, bean-shaped structures that filter the lymphatic fluid. Cancer cells may enter lymphatic vessels, travel to nearby nodes, and cause swelling.
- Bloodstream: Cancer cells can enter the bloodstream through capillaries near the primary tumor. Cancer cells can travel to distant areas of the body once they are in the bloodstream. Cancer cells can travel to distant organs and tissues when they enter the bloodstream.
- Seeding and Implantation: In certain cases, cancerous cells can be shed from a primary tumor. They may then “seed” or implant on nearby organs and structures in the body cavity. It can cause secondary tumors (metastases) to form on organ surfaces such as the liver, peritoneum, or pleura.
- Direct Expansion: Cancer may also spread by physically spreading into adjacent structures. A primary colon tumor may spread directly to adjacent organs such as the abdominal wall or bladder.
- Perineural spread: In certain cases, cancer cells may follow nerves to other sites.
The likelihood of metastasis varies widely depending on the cancer type and stage. The spread of cancer can also differ between sarcomas and carcinomas, due to the differences in their tissue origins.
Cancer spread is a complex phenomenon that depends on many factors. These include the biology of the tumor, the health of the patient, and the efficacy of the treatment. For managing and preventing cancer spread, early detection, accurate staging, and appropriate treatment is crucial.
Diagnosis and Staging
Both carcinomas and sarcomas require a diagnosis and staging. These processes can help to determine the extent and severity of the cancer, provide information on treatment options, and give a prognostic. This is an overview of the typical way that cancer diagnosis and staging is conducted:
Diagnosis:
- Clinical Assessment: A healthcare provider will often begin the diagnostic process by taking a detailed medical history and performing a physical examination. They will ask about symptoms, risk factors, and family history.
- Imaging studies: Different imaging techniques can be used to assess the tumor’s size, location, and involvement of nearby tissues. X-rays are the most common imaging modality, followed by CT scans and MRIs.
- Biopsy: A biopsy is done to confirm the cancer’s presence and type. A biopsy involves the collection of tissue from a suspected cancerous tumor or site. A pathologist examines the tissue under a magnifying glass to determine cancer cells’ characteristics and identify them.
- Histopathological Exam: Tissue obtained from the biopsy undergoes histopathological examination, which includes the evaluation of cellular characteristics, grade, and subtype. This information is used to confirm the diagnosis and plan appropriate treatment.
Staging:
The process of staging is used to determine the extent and severity of cancer. The staging system helps to describe the cancer’s location, size, whether or not it has spread to nearby nodes, and whether it metastasized into distant organs and tissues. Although the staging system for sarcomas and carcinomas can vary, it generally follows the same principles.
- TNM System TNM stands for Tumor Nodes and Metastasis. It involves:
- T (Tumor Size and Extension of Primary Tumor)
- If cancer has spread to lymph nodes nearby, N is the answer.
- M (Metastasis), if cancer has spread to distant organs and tissues.
- Grouping of stages: Once the T, N, M, and stage categories have been determined, they can be combined to give an overall stage. This is usually expressed in Roman numerals, I, II, III, or IV. Higher stage numbers represent more advanced diseases.
- Grading: Certain cancers also receive a grade that reflects their aggressiveness. Grading is important for sarcomas and can involve grading from G1 (low grade) to G3(high grade).
- Clinical Staging vs. pathological staging: Clinical staging is based upon the findings before surgery or treatment. However, pathological staging includes additional information gathered during surgery or pathology reports.
For selecting the best treatment, predicting the prognosis, and monitoring response to therapy, accurate diagnosis and staging are critical. Additional tests may be performed on patients, such as genetic or blood tests, to better characterize cancer and help guide treatment decisions. The stage and grade of cancer will have a significant impact on the treatment options and outlook of the patient.
Treatment
Treatment of both carcinomas (cancers) and sarcomas is dependent on several factors. These include the type of cancer and its location, the stage of the disease, the overall health of the patient, and the individualized treatment plan. The following is an overview of common treatment options for these types of cancers.
Treatment of Carcinomas with:
- Surgery: The primary treatment of localized carcinomas is usually surgical removal of the tumor. To ensure a complete excision, surgeons remove the tumor as well as some healthy tissue surrounding it. In certain cases, minimally invasive procedures can be used.
- Radiotherapy: The use of high-energy X-rays and other radiation sources is used to destroy cancer cells. This treatment can be used either before or after surgery to shrink tumors or treat cancer cells that remain.
- The use of chemotherapy involves drugs that kill cancer cells or slow their growth. It is usually administered systemically. This means that it affects all cancer cells in the body. The chemotherapy may be combined with radiation and surgery.
- A Targeted Treatment: A targeted therapy is a drug that targets specific molecules or pathways in cancer cell growth and spread. They are used for certain types of cancers that have specific molecular defects.
- Anti-Cancer Drugs: Immunotherapy drugs help the immune system of the body to attack and recognize cancer cells. Immunotherapy drugs, such as immune checkpoint inhibitors have shown promising results in the treatment of certain carcinomas.
- The use of hormone therapy for cancers that are dependent on hormones such as breast or prostate cancers. It is designed to block hormones that promote cancer cell growth.
Treatment of Sarcomas with:
- Surgery: The primary treatment of localized sarcomas is surgical resection. The aim is to remove the tumor while preserving as many nearby structures and functionalities as possible. Rarely is amputation necessary.
- Radiotherapy: The use of radiation therapy can be done before or after surgery to shrink tumors or treat cancer cells that remain. Sarcomas in difficult anatomical locations are often treated with radiation therapy.
- Treatment with chemotherapy: The treatment of certain sarcomas is chemotherapy, particularly high-grade and metastatic types. It can be given before or after surgery to reduce tumor size or treat metastatic disease.
- Targeted Treatment: Certain targeted therapies are being investigated for specific subtypes of sarcomas. These drugs are intended to disrupt the molecular processes driving cancer growth.
- Anti-cancer Immunotherapy: Although immunotherapy is used less often for sarcomas than carcinomas, research is being conducted to examine its potential.
- Supportive care: Sarcoma treatments often involve a multidisciplinary treatment approach that includes physical therapy, occupational therapists, and psychosocial support to help patients cope with the emotional and functional challenges of the disease.
The treatment plan depends on several factors, including the subtype of cancer, its stage, patient health, and the individualized treatment plans created by a healthcare team.
Treatment can involve a combination, and it may evolve depending on the patient’s response or disease progression. A personalized treatment plan and early detection are essential for improving the outcomes of individuals with carcinomas or sarcomas.
Prognosis
The prognosis of both sarcomas and carcinomas can be affected by several factors. These include the type of cancer and its stage, the location of tumors, the quality of the cancerous cells, as well as the overall health of the patient, and the effectiveness and efficiency of treatment. The following is a general overview of the prognosis of these cancers.
Prognosis of Carcinomas:
- Early detection: The prognosis for many carcinomas can be favorable, especially if they are detected in an early stage. Early-stage cancers can often be cured with the right treatment. The five-year survival rate is also relatively high.
- Stage: The stage plays an important role in the prognosis. A poorer prognosis is generally associated with advanced-stage carcinomas which have spread to distant structures or organs.
- Types and Locations: The type of carcinoma, and the location within the body where it is located also affects prognosis. Early treatment of some carcinomas like skin cancers can lead to excellent outcomes. Other cancers such as pancreatic cancer have a less favorable prognosis.
- Grade: The grade reflects the aggressiveness in the cancer cells. The prognosis of high-grade carcinomas is worse than that of low-grade cancers.
- Response To Treatment: The prognosis can be affected by the response of cancer to treatment. This includes surgery, chemotherapy, and radiation therapy. Effective treatment can improve outcomes.
- Overall health: The prognosis of a patient can be affected by their general health, and the ability to tolerate treatments. Patients with good health overall often have better results.
The Prognosis of Sarcomas:
- Types and Subtypes: There are many subtypes of sarcomas and the prognosis varies greatly between them. Some sarcomas are associated with better prognoses, while others have a worse outlook.
- Stage: The stage of sarcoma, as with carcinomas is an important factor in the prognosis. Early-stage sarcomas localized at the primary site have better outcomes.
- Grade: The cellular characteristics of sarcomas are often used to grade them. High-grade Sarcomas are more aggressive, and their prognosis is worse than low-grade Sarcomas.
- Location: The location can affect the prognosis. Sarcomas that occur in specific areas such as the extremities are more easily treated than those located in difficult anatomical sites.
- Surgery: The extent and success of the surgical resection, as well as the removal of the tumor with no residual disease, can affect the prognosis. Clear surgical margins are essential.
- Treatment Response: The response to treatment such as chemotherapy, radiation therapy, and targeted therapy may have a significant impact on the prognosis of sarcomas.
- Metastasis: The presence at diagnosis of distant metastases can drastically worsen the prognosis of sarcomas.
The fact that cancer research and treatments have advanced has improved the outcomes of many people with sarcomas and carcinomas. Individual responses to treatment may also vary. Some patients can achieve a long-term remission, or even cure, despite initial unfavorable predictions.
To make informed decisions, patients should speak with their healthcare team about their prognosis and their treatment options.
Conclusion
Sarcoma and carcinoma are two different types of cancer. They differ in their origins, behaviors, diagnoses, and treatments. Early detection and personalized treatment plans can improve the prognosis for both cancer types.
The importance of continuing efforts in cancer management and care is highlighted by the advances in medical research and treatment.