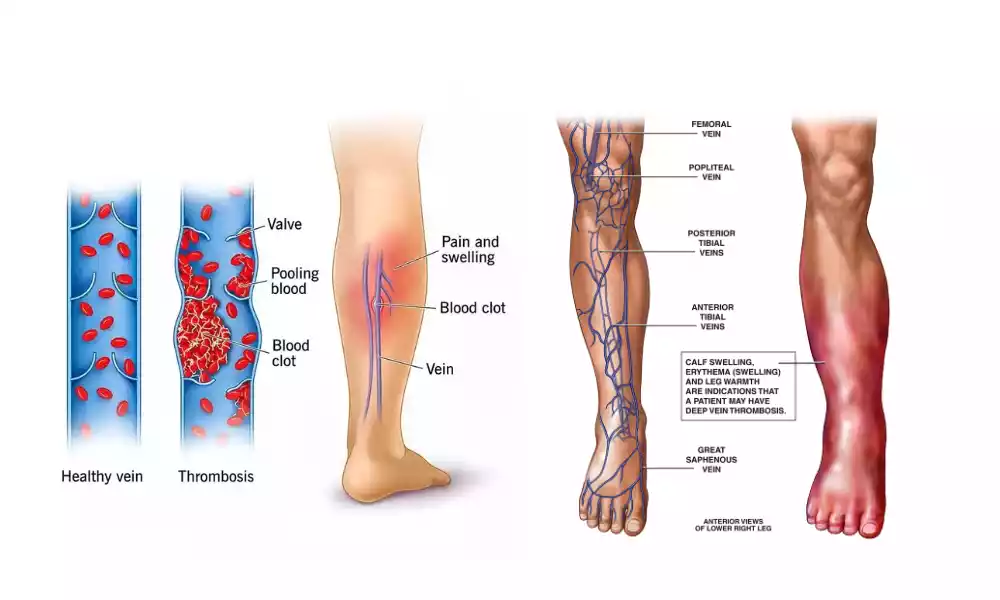
Overview of thrombophlebitis and phlebothrombosis
Thrombophlebitis (blood clots in veins) and phlebothrombosis (blood clots in the veins) are two similar vascular disorders. They share similarities but also have different characteristics and clinical implications.

This is a brief overview of the two conditions:
Thrombophlebitis:
- Definition: A thrombophlebitis is an inflammatory condition that involves the swelling of a vein and the formation of blood clots (thrombosis).
- Etiology:
- Inflammatory component (Phlebitis): Phlebitis is a condition that begins with an inflammation of the vein. This can be caused by trauma, infection or irritation due to intravenous catheters.
- Formation of Blood Clots: The inflammation activates the body’s cascade of clotting, resulting in the formation of blood clots within the affected vein.
- Risk Factors:
- Injury or trauma to a vein.
- Infections of the veins or surrounding them
- Prolonged immobility, or venous stasis.
- Use of IV catheters and medications
- Clinical Features:
- Local Symptoms: Pain, swelling, redness, and warmth are common symptoms at the site of the vein.
- Systemic symptoms: Fever and malaise are common systemic symptoms.
- Diagnosis:
- On examination, doctors may detect tender or inflamed veins.
- Imaging: An ultrasound or venography may confirm the presence of blood clots within the vein.
- Treatment:
- Treatment: Warm compresses and anti-inflammatory medication.
- Anticoagulation therapy: blood thinners (anticoagulants), to prevent the clot from spreading.
- In severe cases, it may be necessary to remove the clot from the affected vein or perform surgery.
- Prognosis and Complications: Untreated thrombophlebitis may lead to complications, such as deep-vein thrombosis or pulmonary embolism. A favorable prognosis is usually achieved by prompt treatment.
Phlebothrombosis:
- Definition: A phlebothrombosis, or blood clots in veins is similar to thrombophlebitis. It lacks the significant inflammation seen in thrombophlebitis.
- Etiology:
- The main cause of phlebothrombosis is the formation of blood clots in veins. This condition often occurs without any associated inflammation.
- Risk Factors:
- Hypercoagulable disorders are conditions that can increase the risk of blood clots.
- Venous stasis is a slow blood flow in veins.
- Endothelial Injury (damage of the inner linings of veins).
- Clinical Features:
- The phlebothrombosis can be asymptomatic, or only present with local symptoms.
- The risk of clot embolization is of primary concern. This occurs when the clot breaks free and travels to other parts of your body. It can cause serious complications.
- Diagnosis:
- To detect blood clots in veins, imaging techniques like ultrasound and computed tomography (CT scans) are used.
- Diagnostic tests such as D-dimer or coagulation studies can also be used.
- Treatment:
- Anticoagulation Treatment: To prevent the spread of clots and embolization, anticoagulant treatment is the primary treatment.
- Thrombolysis is used in severe cases to dissolve the blood clot.
- Complications & Prognosis: The primary concern with phlebothrombosis involves the risk of embolization. This can lead to pulmonary emphysema or organ damage. Early anticoagulation treatment usually yields positive outcomes.

Both thrombophlebitis (blood clots in veins) and phlebothrombosis (clots without inflammation) involve the formation of blood clots. However, thrombophlebitis has an associated inflammation, whereas phlebothrombosis is predominantly thrombosis. Both conditions require an accurate diagnosis and the appropriate management to avoid complications.
Definition and significance of vascular disorders
Definition: Vascular Disorders refer to a grouping of medical conditions that affect blood vessels including capillaries, veins, and arteries. These disorders can cause blood flow to be disrupted and have serious health implications.
Importance: Vascular diseases are important because they can lead to a variety of health problems, such as heart disease, strokes, deep vein thrombosis, and peripheral arterial disease. Worldwide, they are the leading cause of mortality and morbidity. Early diagnosis and management are essential to reduce complications and improve health outcomes.
Thrombophlebitis and Phlebothrombosis comparison table
Here’s a comparison table highlighting the key differences between thrombophlebitis and phlebothrombosis:
| Characteristic | Thrombophlebitis | Phlebothrombosis |
|---|---|---|
| Definition | Inflammation of a vein along with the formation of a blood clot within the affected vein. | Formation of blood clots within veins, often without significant inflammation. |
| Etiology | – Inflammatory component (phlebitis) – Formation of blood clots (thrombosis) | Primarily results from blood clot formation within veins, often without inflammation. |
| Risk Factors | – Trauma or injury to the vein – Infections – Venous stasis – Use of IV catheters or medications | – Hypercoagulable disorders – Venous stasis – Endothelial injury |
| Clinical Features | – Local symptoms (pain, redness, warmth, swelling) – Systemic symptoms (fever, malaise) | – May be asymptomatic or present with minimal local symptoms – Risk of clot embolization |
| Diagnosis | – Physical examination (tender, inflamed veins) – Imaging (ultrasound, venography) | – Imaging techniques (ultrasound, CT scans) – Laboratory tests (D-dimer, coagulation studies) |
| Treatment | – Conservative management (elevation, warm compresses) – Anticoagulation therapy – Surgical intervention (in severe cases) | – Anticoagulation therapy (primary treatment) – Thrombolysis (in severe cases) |
| Complications | – Deep vein thrombosis (DVT) – Pulmonary embolism – Infection (if present) | – Risk of embolization (clot breaking free and traveling to other body parts) – Pulmonary embolism – Organ damage (if clot embolizes) |
| Prognosis | Generally favorable with prompt treatment. | Good outcomes with timely anticoagulation therapy. |
This table provides a concise overview of the main differences between thrombophlebitis and phlebothrombosis, including their definitions, etiology, clinical features, diagnosis, treatment, complications, and prognosis.
Importance of distinguishing between the two conditions
It is important to distinguish between thrombophlebitis (blood clots) and phlebothrombosis for several reasons.
- Treatment Method: It is important to differentiate between these two conditions because the treatment methods can differ significantly. Thrombophlebitis is characterized by inflammation and requires specific interventions that address the clot as well as inflammation. Phlebothrombosis, on the other hand, requires primarily anticoagulation therapy in order to prevent clot expansion and embolization. The right treatment can help improve outcomes for patients and prevent complications.
- Risk assessment: An accurate diagnosis allows healthcare providers to assess the patient’s risk. Thrombophlebitis can be caused by conditions such as infections or intravenous caths, whereas phlebothrombosis often results from hypercoagulable disorders. Understanding the risk factors can help prevent and manage future episodes.
- Preventing complications: Both conditions may lead to serious complications when left untreated. Thrombophlebitis may progress to deep-vein thrombosis or pulmonary embolism. Phlebothrombosis is associated with a risk of embolization. Correct diagnosis and treatment reduce the risk of life-threatening complications.
- Resource allocation: Accurate diagnoses ensure that healthcare resources are allocated appropriately. Patients with thrombophlebitis, for example, may need more localized interventions such as the removal of an intravenous tube, while patients with phlebothrombosis might require anticoagulation treatment. The efficiency of healthcare is improved by the proper allocation of resources.
- Patient Management and Education: Understanding the specific condition is helpful in educating patients on their condition, treatment alternatives, and prevention measures. Knowing the type of vascular disorder can help patients better understand how important it is to adhere to treatment plans and make lifestyle changes.
- Data Collection and Research: Accurately identifying thrombophlebitis from phlebothrombosis in clinical practice is important for the collection of accurate data. These data are valuable for research, as they allow for a better understanding of the prevalence, risk factors, and outcome of these conditions.
- Documentation and Legal Purposes: It is important to correctly diagnose and differentiate between these conditions for legal and medical purposes. This ensures that the medical records accurately represent a patient’s health, treatment, and progress. This can be crucial for insurance claims and legal liability.
It is important to distinguish between thrombophlebitis (or phlebothrombosis) and thrombophlebitis in order to tailor appropriate treatments. This will reduce the risk of complications and optimize resource allocation. This ultimately leads to improved patient care and healthcare outcomes.
Clinical Scenarios and Differential Diagnosis
Differential diagnosis and clinical scenarios are crucial in determining the difference between thrombophlebitis (or phlebothrombosis) and thrombophlebitis.
Considerations for differential diagnosis and clinical scenarios:
Clinical Scenario #1: A patient with a painful, red, and swollen leg
- Differential Diagnosis:
- Thrombophlebitis: Thrombophlebitis is often accompanied by local symptoms, such as redness, swelling, and warmth at the affected vein. This diagnosis should be considered if there has been a recent history of trauma or IV catheter usage.
- Phlebothrombosis: Although less common, local symptoms can be caused by phlebothrombosis. This should be taken into consideration, especially if hypercoagulable disorders are suspected.
Clinical Scenario #2: A patient with fever and pain in the arm following IV catheter placement
- Differential Diagnosis:
- Thrombophlebitis: The presence of an IV can cause irritation of the veins. If the patient has local symptoms such as fever and arm pain, it is important to consider thrombophlebitis.
- Cellulitis: Infections may also cause localized redness and pain. Physical examinations and imaging studies should be performed to rule out cellulitis.
Clinical Scenario #3: Asymptomatic Patient With a History Of Blood Clotting Disorders
- Differential Diagnosis:
- Phlebothrombosis: Even asymptomatic or minimally asymptomatic blood clots in veins can indicate phlebothrombosis. This is especially true for individuals with hypercoagulable disorders.
- Thrombophlebitis: Thrombophlebitis is more likely to occur in asymptomatic patients unless they have evidence of inflammation.
A patient with acute shortness of breath and chest pain
- Differential Diagnosis:
- Pulmonary Embolization: Both thrombophlebitis or phlebothrombosis may lead to pulmonary embolism if clots embolize. A pulmonary embolism can be a serious complication of either condition. It should always be suspected when there is chest pain and acute shortness of breath.
- Thrombophlebitis and Phlebothrombosis: The focus in this scenario is to identify the source of embolism. This may require additional imaging or diagnostic testing.
Clinical Scenario #5: A Patient With a History Of Venous Stasis Ulcers
- Differential Diagnosis:
- Phlebothrombosis: Recurrent thrombosis in veins should be considered by patients who have a history of venous ulcers. This is especially true if the patient does not show signs of active inflammation. This condition could be caused by underlying venous failure.
- Thrombophlebitis: Inflammation and redness can be present at the site of an ulcer. Thrombophlebitis may contribute to this.
These clinical scenarios demonstrate the importance of considering a variety of factors in the differential diagnosis between thrombophlebitis, phlebothrombosis, and patient history. This emphasizes the importance of a thorough evaluation that may include a physical exam, imaging studies, and laboratory tests to distinguish between these two conditions.
Conclusion
In clinical practice, it is important to distinguish between thrombophlebitis (also known as phlebothrombosis) and thrombophlebitis. Although these vascular disorders have some similarities, they also differ in their causes, symptoms, and treatment methods.
Accurate diagnoses are essential to provide appropriate care, prevent complications, and improve patient outcomes. To make the right diagnosis, healthcare professionals must conduct thorough evaluations and carefully review clinical scenarios. This will ensure that patients receive effective treatment and interventions tailored to their condition.