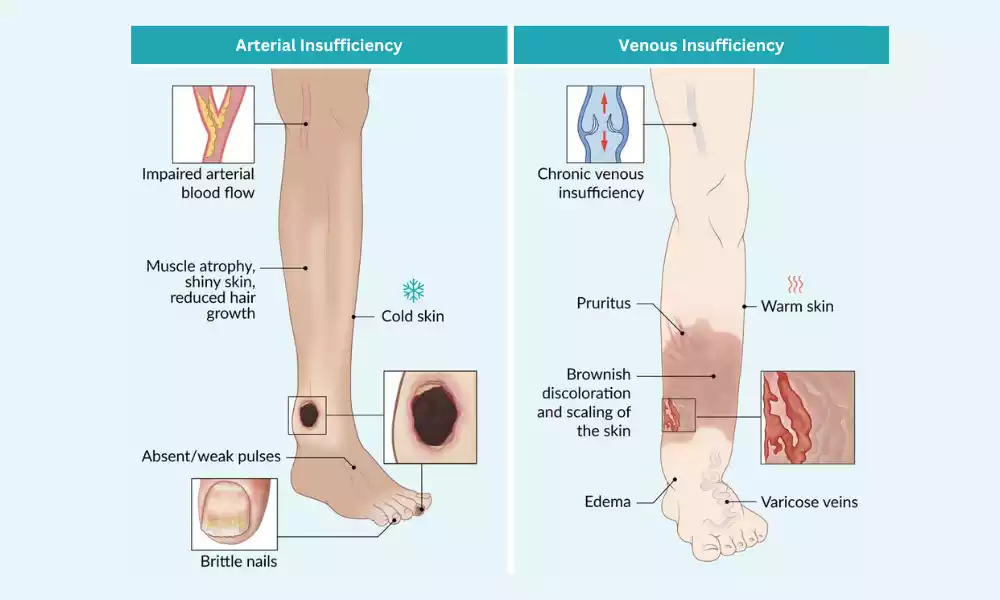
Definition of Venous Insufficiency
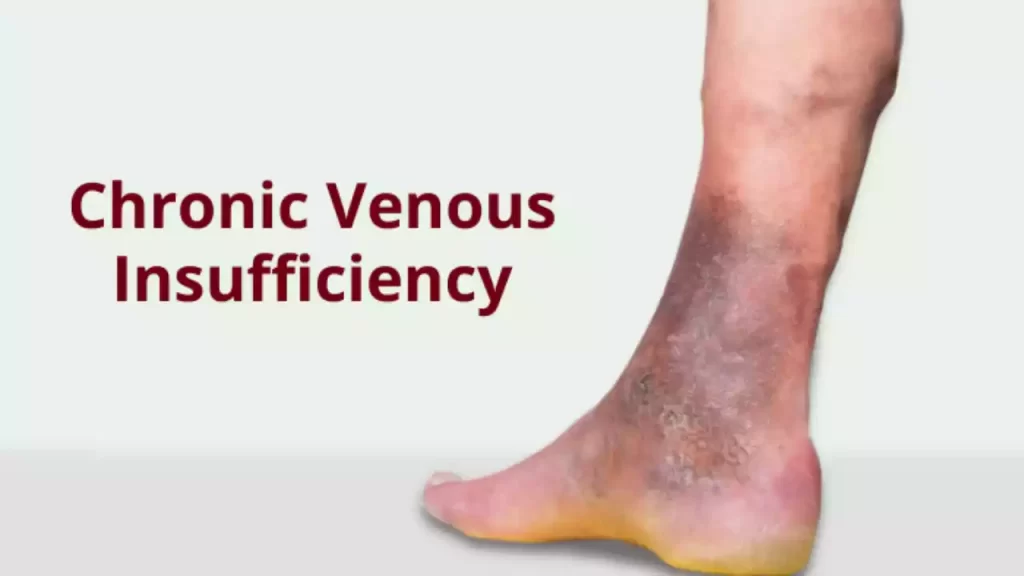
Venous insufficiency is a medical condition that is caused by an insufficient function of the venous systems in the legs. The veins have difficulty returning blood efficiently from the extremities, usually the legs, to the heart.
The impaired blood flow may cause swelling, pain, changes in the skin, and even venous ulcers. Venous insufficiency can be caused by problems with the one-way vein valves that prevent blood from flowing backward. These valves can malfunction and cause blood to pool in veins. This is what causes venous insufficiency symptoms.
Definition of Arterial Insufficiency
Arterial insufficiency is also known as arterial obstruction disease or peripheral artery disease (PAD). It is a medical disorder characterized by an insufficient flow of blood through the arteries.
This occurs when the arteries supplying oxygen-rich blood into these areas narrow or become blocked because of the buildup or other vascular problems. Reduced blood flow can cause a variety of symptoms including cramping, pain, numbness, and coldness.
In severe cases, arterial insufficiency may cause tissue damage, ulcers, and gangrene. This condition is associated with cardiovascular events such as heart attacks and strokes. It is important to have a proper diagnosis and treatment plan in order to avoid complications and improve the patient’s quality of life.

Venous and Arterial Insufficiency comparison chart
Here’s a comparison chart highlighting the key differences between Venous Insufficiency and Arterial Insufficiency:
| Aspect | Venous Insufficiency | Arterial Insufficiency |
|---|---|---|
| Definition | Inadequate function of the venous system, leading to poor blood return from extremities. | Insufficient blood flow through arteries, often due to blockages or narrowing. |
| Location | Primarily affects the veins, commonly in the legs. | Primarily affects the arteries, commonly in the legs, arms, or other extremities. |
| Causes | – Venous valve dysfunction – Deep vein thrombosis (DVT) – Obesity – Aging – Pregnancy | – Atherosclerosis (buildup of plaque) – Smoking – Diabetes – Hypertension – High cholesterol |
| Symptoms | – Edema (swelling) – Varicose veins – Skin changes (hyperpigmentation, dermatitis) – Venous ulcers | – Intermittent claudication (pain during activity) – Cold extremities – Skin changes (pallor, ulceration) |
| Diagnostic Methods | – Doppler ultrasound – Venous duplex scan – Clinical examination | – Ankle-brachial index (ABI) – Angiography – Clinical examination |
| Complications and Long-Term Effects | – Venous ulcers – Cellulitis – Chronic venous insufficiency – Deep vein thrombosis (if untreated) | – Gangrene – Limb amputation – Cardiovascular events (e.g., heart attack, stroke) |
| Treatment | – Compression therapy – Elevation of legs – Lifestyle modifications (e.g., weight loss, exercise) | – Revascularization procedures (e.g., angioplasty, bypass surgery) – Medications (e.g., antiplatelets) – Lifestyle changes (e.g., smoking cessation, blood pressure management) |
| Prognosis | Generally better with proper management. | Can be serious, with the risk of limb loss or cardiovascular complications if untreated. |
| Prevention Strategies | – Regular exercise – Weight management – Leg elevation – Compression stockings | – Smoking cessation – Diabetes management – Blood pressure control – Healthy diet |
This comparison chart provides a concise overview of the main differences between venous insufficiency and arterial insufficiency in terms of their causes, symptoms, diagnostic methods, complications, treatment, and prevention strategies. It’s important to note that both conditions require medical attention and proper management to prevent complications and improve the patient’s quality of life.
Importance of Distinguishing Between the Two
It is important to distinguish between arterial and venous insufficiency in medicine.
- Selecting the Right Treatment: These two conditions require very different treatments. Venous insufficiency is often treated with compression therapy, lifestyle changes, and medications. Arterial insufficiency can be treated by surgical intervention or medication to improve blood circulation. Accurate diagnosis improves the chances that patients will receive targeted and effective treatment.
- Complications Prevention: Left untreated, both conditions can cause serious complications. Venous insufficiency may cause painful ulcers or chronic skin changes. Arterial insufficiency could lead to tissue damage and amputation of limbs. Early diagnosis can reduce the risk of complications, and improve the quality of life for the patient.
- Risk assessment: Differentiating between the two conditions can help healthcare providers assess their patient’s overall cardiovascular health. Arterial insufficiency can be associated with an increased risk of cardiovascular events such as strokes and heart attacks, which could require more extensive management. Venous insufficiency can have its own risks and implications. Addressing them quickly is important.
- Patient education: It is important to communicate clearly with patients regarding their condition and the implications of it. This will help them understand and adhere to their treatment plan. Patients who are properly informed as to whether they suffer from venous or aortic insufficiency are more likely than others to adhere to recommended lifestyle changes and treatments.
- Resource Allocation: Medical Resources, such as healthcare professionals’ time, diagnostic tools and medical resources are limited. It is important to differentiate between arterial and venous insufficiency so that resources can be used effectively. Prioritizing patients with arterial insufficiency can help reduce the risk of serious complications.
- Data Collection and Research: An accurate diagnosis is crucial for research since it allows the collection of precise statistics on the incidence, prevalence, and outcomes of the conditions. These data are vital to improving healthcare and advancing medical research.
- Legal Considerations and Insurance: In certain cases, the distinction made between arterial and venous insufficiency can have legal or insurance implications. Medical billing and insurance coverage are dependent on the correct documentation of the condition.
It is important to distinguish between venous insufficiency and arterial insufficiency for a number of reasons, including providing the best treatment, preventing complications, and assessing vascular health. This will also help with educating patients and allocating resources effectively, as well as addressing insurance and legal issues. This ultimately leads to improved patient outcomes and healthcare practices.
Anatomy and Physiology
Anatomy, physiology, and biology are closely related fields that study the structure and functions of living organisms.
Anatomy: Anatomy is a branch of biology that focuses on the organization and structure of living organisms. The study and description of physical structures of both the internal and external parts of an organism is part of anatomy. Anatomy includes:
- Gross anatomy: This is the study of large structures that are visible without a microscope. Examples of gross anatomy include the skeleton, major organs, and muscles.
- Microscopical Anatomy: This branch of anatomy, also known as histology or microscopic anatomy, deals with tissues and cells on a microscopic scale. The use of microscopes is required to study cellular structure and organization.
- Comparative anatomy: This field compares anatomical structures to identify similarities and differences. It is useful in understanding the evolutionary relationships among organisms.
- Developmental anatomy: This section explores changes in the structure of an organism from conception to adulthood. It focuses on embryonic development and the evolution of structures over time.
Biology: The study of biology is concerned with the way living organisms work and perform their biological processes. It is the study of mechanisms that enable organisms to maintain their homeostasis and respond to stimuli. The key aspects of physiology are:
- Cellular Biology: This branch examines processes such as cell metabolism, the transport of molecules, and cell signaling.
- Organ Biology: This focuses on specific organs in the body such as the brain, heart, lungs, and kidneys. The study of organ physiology focuses on how the various organs function and interact.
- Systemic Biology: This section explores the ways in which different organ systems work together to maintain body functions. The respiratory system, the nervous system, and the cardiovascular system are all examples of systems.
- pathophysiology: The study of abnormal physiological processes that occur during illness or injury. It is useful in understanding the mechanisms behind various health conditions.
Anatomy is closely related to physiology because it’s essential to understand how an organism functions in order for you to fully grasp its structure (anatomy). Together, they form a comprehensive framework to study the complexity of living organisms and the mechanisms that control their form and function.
Diagnostic Methods
When diagnosing venous and arterial insufficiency, healthcare professionals utilize various diagnostic methods and tests to accurately identify and differentiate between the two conditions.
Here are the key diagnostic methods for each:
Diagnostic methods for Venous Insufficiency :
- Clinical Assessment:
- A comprehensive physical examination includes an assessment of the patient’s symptoms and medical history.
- Duplex Ultrasound:
- This imaging technique combines Doppler and traditional ultrasound to show veins, blood flow, and other features.
- It can help identify varicose and venous veins, as well as deep vein thrombosis.
- Venous Doppler ultrasound:
- Doppler ultrasound focuses on the assessment of blood flow in veins.
- The device can be used to detect abnormalities and the direction of blood circulation in the veins.
- CT Scan or MRI:
- In more complex cases, these imaging tests can be used to obtain detailed images of the vein system and surrounding tissue.
Diagnostic Methods of Arterial Insufficiency :
- Clinical Assessment:
- A thorough physical examination includes a review of the medical history of the patient and an evaluation of their symptoms.
- Ankle Brachial Index:
- Test that measures blood flow by comparing blood pressure in the ankle with the arm.
- A low ABI is indicative of arterial insufficiency.
- Doppler ultrasound:
- This test is similar to the venous Doppler and can assess blood flow. However, it focuses more on the arterial system.
- This test can detect blockages, stenosis, or reduced blood circulation in the arteries.
- Angiography:
- Injecting a contrast dye in the arteries and then imaging with X-rays is a more invasive technique.
- This provides detailed images of arterial blood vessels, which can be used to locate blockages or stenosis.
- Magnetic Resonance Angiography and Computed Tomography Angiography:
- Imaging techniques using MRI or CT to create detailed images that help identify blockages, stenosis, or aneurysms.
- Pulse volume recording (PVR):
- Tests that measure blood volume in specific body parts, such as toes and fingers, are used to determine arterial blood flow.
If you suspect arterial or venous insufficiency, it’s important to speak with a medical professional. The healthcare professional will combine these diagnostic methods based on the severity and clinical presentation of the condition to make an accurate diagnosis. Both venous and arterial insufficiency can be effectively managed with early diagnosis and intervention.
Prognosis and Outlook
The outlook and prognosis for people with venous or arterial insufficiency depend on several factors. These include the severity of the disease, the timely diagnosis and treatment of the condition, the overall health of the patient, and their adherence to lifestyle changes.
This is a summary of the prognosis for each condition:
Venous Insufficiency:
- Prognosis of mild to moderate cases:
- The prognosis for venous insufficiency can be favorable when it is detected and treated early.
- Symptoms like swelling and pain are often improved or controlled with the right treatment such as compression therapy, lifestyle changes, and other treatments.
- The majority of people can live a fairly normal life, without major complications.
- The prognosis of severe cases or untreated Venous Insufficiency:
-
- If venous failure progresses untreated, complications such as venous ulcers may develop.
- Severe venous Ulcers are difficult to treat. They may require wound care that is specialized and an extended healing period.
- Early intervention is essential to avoid complications and improve the outlook.
- Long-Term Management:
- Even if venous insufficiency can be successfully managed, it is a chronic disease that requires ongoing treatment.
- It is important to follow up with your healthcare provider regularly in order to monitor your condition and make any necessary adjustments.
Arterial Insufficiency :
- Prognosis of Mild Cases:
- Early diagnosis and management can improve the prognosis in mild cases of arterial dysfunction.
- With lifestyle changes, medication, and regular monitoring, you can alleviate symptoms and improve circulation.
- The prognosis of severe cases or untreated arterial insufficiency is:
- A more cautious prognosis can be given for severe arterial insufficiency. This is especially true when it’s complicated by conditions such as gangrene and limb-threatening ischemia.
- A delayed or insufficient treatment may lead to the amputation of a limb.
- Long-Term Management:
- Arterial insufficiency is often a lifelong condition, especially when atherosclerosis has been the cause.
- To maintain blood flow in the affected limbs, lifestyle modifications, medications, and revascularization (such as angioplasty, bypass surgery or angioplasty) procedures may be required.
- Complications:
- The quality of life of an individual can be significantly affected by complications of arterial insufficiency. These include tissue loss and amputation.
- It is important to follow up with a vascular expert regularly in order to avoid or treat complications.
Early diagnosis and appropriate treatment are key in both venous and artery insufficiency. This will improve the outlook and prognosis. To manage their condition, patients should work closely together with their healthcare provider to create a customized treatment plan. They should also follow the lifestyle changes recommended by their healthcare provider. Individuals with venous or arterial insufficiency can maintain their health and well-being by following treatment recommendations and regularly monitoring.
Prevention Strategies
Prevention strategies for Venous Insufficiency :
- Regular Physical Activity: Exercise regularly to improve blood circulation and strengthen your legs.
- Maintaining a Healthy Body Weight: Avoid Obesity, as excessive weight can cause venous strain.
- Elevate Legs: Elevate legs while resting or sleeping in order to reduce swelling.
- Compression stockings: Use the compression stockings prescribed by your healthcare provider to improve venous blood circulation.
- Do not stand or sit for long periods of time: Change positions and take breaks regularly to avoid blood pooling.
Prevention strategies for arterial insufficiency:
- Stop Smoking: Smoking damages the arteries and worsens arterial disease. It is important to quit.
- Reduce the Risk of Atherosclerosis by Managing Hypertension and High Cholesterol Levels: Manage hypertension levels and high cholesterol levels.
- Regular Exercise: Promoting arterial health through regular aerobic exercise.
- Healthy diet: Eat a balanced, low-fat diet rich in fruits and vegetables.
- Adherence to Medication: Take prescribed medication to manage underlying diseases like diabetes or hypertension.
- Foot care: Check your feet regularly and keep them clean. Address any injuries promptly.
- Regular Checkups: Seek regular vascular health assessment from a healthcare provider, especially if you are at risk.
These strategies can reduce the risk of developing venous and arterial insufficiency, as well as improve overall vascular function.
Conclusion
It is important to differentiate between venous insufficiency and arterial insufficiency for an early diagnosis and efficient management. Venous insufficiency is often characterized by swelling and varicose veins, whereas arterial insufficiency can be characterized by pain and non-healing injuries.
A favorable outcome is dependent on timely diagnosis, and appropriate treatment including lifestyle changes and medical interventions. Individuals can maintain their vascular health and reduce their risk by following preventative strategies and receiving regular medical care.