Importance of differentiating between Dengue IgG, IgM, and NS1
The differentiation between Dengue IgG, IgM, and NS1 is crucial for accurate diagnosis and management of dengue fever.
Here are the key reasons why it is important to distinguish between these markers:
- Early diagnosis: Differentiating between IgG, IgM, and NS1 helps in the early detection of dengue infection. Each marker has a specific timeline of appearance in the bloodstream, allowing for timely diagnosis. Early identification of dengue infection enables healthcare providers to initiate appropriate treatment and monitoring measures promptly.
- Disease staging: The presence and levels of IgG, IgM, and NS1 markers provide valuable information about the stage of dengue infection. IgM antibodies are typically detected during the acute phase of the disease and can help confirm recent infection. IgG antibodies, on the other hand, appear later and persist for a longer duration, indicating past exposure or immunity. Early-stagedetection of the NS1 antigen may assist in diagnosing primary dengue infections.
- Differential diagnosis: Dengue fever shares clinical symptoms with other febrile illnesses, such as malaria or chikungunya. The differentiation between IgG, IgM, and NS1 markers helps distinguish dengue fever from other similar diseases, allowing for appropriate management and treatment.
- Epidemiological surveillance: Accurate identification and tracking of dengue cases are essential for monitoring disease prevalence and implementing control measures. Differentiating between IgG, IgM, and NS1 markers facilitates the surveillance of dengue infections in a population, aiding in the early detection of outbreaks and the assessment of disease burden.
- Patient management: The differentiation between these markers plays a crucial role in determining the appropriate patient management strategy. For instance, patients with positive NS1 results may require closer monitoring for potential complications, such as severe dengue. IgG and IgM results can help assess the patient’s immune status and guide follow-up care.
Distinguishing between Dengue IgG, IgM, and NS1 is essential for early diagnosis, disease staging, differential diagnosis, epidemiological surveillance, and effective patient management.
This differentiation enables healthcare professionals to provide appropriate care, monitor disease progression, and implement timely interventions to prevent complications associated with dengue fever.
A brief overview of dengue fever
Dengue fever is caused by a virus known as dengue that spreads via Aedes mosquito bites that harbor infected with it. It is a significant public health concern, particularly in tropical and subtropical regions of the world.
Key points about dengue fever include:
- Dengue fever: is characterized by sudden onset symptoms such as high fever, severe headaches (usually behind your eyes), muscle and joint pain, fatigue, and mild bleeding like nosebleeds and easy bruises. Some individuals may experience more severe symptoms, leading to dengue hemorrhagic fever or dengue shock syndrome.
- Disease progression: Dengue fever is characterized by distinct phases. The initial febrile phase lasts for about 2-7 days, during which the individual experiences high fever and other associated symptoms. This is followed by a critical phase, typically around days 3-7, where there may be a drop in temperature, leading to an increased risk of complications. The recovery phase follows, during which the fever subsides, and the individual gradually recovers.
- Diagnosis: Dengue fever is diagnosed through laboratory tests, including the detection of dengue-specific antibodies (IgM and IgG) or the viral NS1 antigen. Molecular tests like polymerase chain reaction (PCR) can also be used to detect the presence of the dengue virus. Clinical assessment and the patient’s travel history are also important factors in the diagnosis.
- Treatment: There is no specific antiviral treatment for dengue fever. Management focuses on relieving symptoms and providing supportive care, such as rest, hydration, and pain relief with acetaminophen (paracetamol). Aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided due to an increased risk of bleeding complications.
- Prevention: Preventing mosquito bites is the most effective way to prevent dengue fever. This includes using mosquito repellents, wearing protective clothing, and using bed nets. Eliminating stagnant water sources where mosquitoes breed is also crucial in controlling the mosquito population.
- Dengue Fever Complications: For severe dengue infections, dengue fever can develop into dengue hemorrhagic (DHF) fever or dengue shock syndrome (DSS), marked by massive blood loss, organ damage, and decreased blood pressure.
Dengue fever is a viral infection transmitted by mosquitoes, causing flu-like symptoms. While most cases resolve on their own with supportive care, severe forms of the disease can be life-threatening. Early diagnosis, appropriate management, and preventive measures can significantly lower the effects of dengue fever on individuals and communities alike.
Understanding Dengue Fever
Dengue fever is caused by a virus from the Flaviviridae family. Dengue fever is transmitted primarily through bites from infected Aedes mosquitoes – most frequently Aedes Aegypti – which bite humans. Dengue fever has become an increasing public health threat in areas where such mosquitoes thrive, which poses serious public health concerns.

Dengue fever is a serious disease that can be understood by understanding the following key points:
- Transmission: The dengue Virus is transmitted to humans primarily through the bites of female Aedes mosquitoes infected with the dengue virus. The mosquitoes are infected by a bloodstream-carrying dengue virus. The virus multiplies within the mosquito and can then be spread to other people through mosquito bites.
- Dengue fever symptoms are sudden: The most common symptoms are high fever, severe headaches (often behind your eyes), fatigue, joint and muscle pains, rash, and mild bleeding such as nosebleeds and easy bruises. Some people may develop more severe cases of the disease such as dengue hemorrhagic (DHF) and dengue shock syndrome. These can be life-threatening.
- Dengue fever: Dengue fever develops gradually through several distinct phases. Initial febrile symptoms typically include high fever. Next comes the critical phase, usually occurring on days 3-7 and marked by decreased temperatures and an increase in complications; and finally comes the recovery phase where fever subsides gradually and the person recovers over time.
- clinical symptoms: Dengue fever can be diagnosed based on laboratory testing, and travel history. The detection of dengue-specific antibodies (IgM or IgG), as well as the viral NS1 Antigen, are among the laboratory tests. Dengue virus can be detected using molecular tests such as polymerase chain reactions (PCR).
- Dengue fever is not treated with antiviral drugs: The management focuses on relieving the symptoms and providing supportive treatment. Rest, hydration (to prevent dehydration), and acetaminophen, or paracetamol, are all important. Aspirin and NSAIDs can increase bleeding complications.
- Dengue fever: can be prevented by preventing mosquito bites. Use mosquito repellents and bed nets. It is important to eliminate stagnant water where mosquitoes can breed.
- Dengue fever has a global impact: Millions of people are affected every year, particularly in tropical and subtropical areas. Dengue fever cases have increased dramatically due to factors including urbanization, travel, and climate changes.
Understanding dengue fever’s symptoms, diagnosis and prevention is critical to controlling its spread while providing appropriate care to those affected. Public health initiatives focused on mosquito control, early diagnosis, and prompt management can reduce its negative impacts.
Dengue IgG
Dengue IgG refers to immunoglobulin G antibodies produced by the immune system in response to dengue virus infection. Immunoglobulins, also known as antibodies, are proteins produced by the immune system to help recognize and neutralize foreign substances, such as viruses or bacteria.
Here are some critical points about Dengue IgG:
- Production: After being exposed to dengue virus infection, our immune systems respond by producing various kinds of antibodies including IgG. Dengue IgG antibodies are generated as a result of the immune system’s recognition and response to the dengue virus antigens.
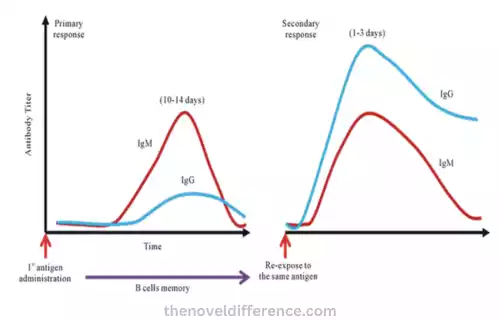
- Timeline: IgG antibodies typically appear in the bloodstream after the acute phase of dengue infection. They begin to rise a few days after the onset of symptoms and can persist for months or even years after the infection has resolved.
- Clinical significance: The presence of Dengue IgG antibodies indicates past exposure or previous infection with the dengue virus. It suggests that the individual has developed an immune response to the virus. Dengue IgG antibodies are not typically useful for diagnosing acute or recent dengue infections, as they take time to develop and may persist for an extended period after the infection.
- Interpretation of test results: Dengue IgG tests are often used in combination with other diagnostic tests to assess a person’s dengue infection status. A positive result for IgG antibodies indicates previous exposure or infection, but it does not indicate the current infection status. The interpretation of Dengue IgG test results should take into account the individual’s clinical history, symptoms, and other laboratory findings.
- Immunity: The presence of Dengue IgG antibodies suggests some level of immunity to future dengue virus infections. It is important to remember that a dengue infection of one serotype will not protect you against other serotypes for the rest of your life. There are four distinct serotypes of the dengue virus, and subsequent infections with different serotypes can still occur, potentially leading to more severe forms of dengue.
Dengue IgG testing plays a role in assessing the immune status of individuals and can contribute to epidemiological surveillance and research studies. However, it is not typically used as a standalone test for diagnosing acute dengue infections.
Clinical evaluation, other laboratory tests (such as Dengue IgM and NS1), and the overall presentation of the patient are essential in making a comprehensive diagnosis of dengue fever.
Dengue IgM
Dengue IgM refers to immunoglobulin M antibodies produced in response to dengue virus infections by our immune systems. Antibodies, commonly referred to as immunoglobulins, help recognize and neutralize foreign substances such as viruses or bacteria entering our bodies by producing proteins called immunoglobulins that identify them and neutralize their harmful effects.
Here are a few key aspects of Dengue IgM:
Production: When infected with the dengue virus, our immune systems respond by producing IgM antibodies as part of their defense mechanisms against dengue antigens. These responses include IgM production as an immediate reaction.
Timeline: Dengue IgM antibodies often first appear during the acute phase of infection with the dengue virus and are among the first produced by our immune systems in response. They should become detectable within days after starting symptoms and continue for some time thereafter.
Clinical Significance: Dengue IgM antibodies indicate recent or acute infection with the dengue virus, suggesting an individual was recently exposed and their immune system is actively creating antibodies to fight off infection. They serve as diagnostic indicators early in dengue fever cases to confirm the diagnosis.
Interpretation of Results: Dengue IgM tests are frequently used to detect recent dengue virus infections; a positive result for IgM antibodies indicates an active or recent dengue infection; however, false positives may arise and confirmatory testing may be required before conclusively diagnosing dengue IgM results. When interpreting Dengue IgM results it should take into account clinical symptoms, history, and laboratory findings for accurate interpretation.
Immunity: Dengue IgM antibodies indicate a successful immune response against dengue virus infections and may signal that individuals may be making strides toward immunity against future dengue virus outbreaks; however, the mere presence of IgM antibodies cannot ensure full protection; immunity depends on multiple factors related to both individual response as well as certain serotypes of dengue viruses.
Dengue IgM testing: This can play an instrumental role in the early diagnosis of dengue fever. Healthcare providers use it to quickly identify recent infections and implement appropriate management and monitoring regimens; however, for best results and assessment it should be used alongside additional diagnostic tests or clinical evaluations to confirm its accuracy and determine its severity.
Dengue NS1
Dengue NS1 stands for non-structural protein 1 antigen of dengue virus infection and release into the bloodstream early during infection. This glycoprotein protein is produced early during infection with the dengue virus and released into circulation as soon as it forms.
Here are a few important details about Dengue NS1:
Production and Detection: NS1 antigen is released by dengue virus-infected cells at an early stage of infection, secreted into the bloodstream, and can be detected long before specific antibodies develop; its presence serves as an early diagnostic indicator of dengue infection.
Clinical Relevance: NS1 antigen detection can be particularly helpful in the early detection and management of acute dengue infections, allowing for prompt management and appropriate patient care. NS1 antigen can typically be detected within several days after the illness has started and may help identify primary cases of dengue infection.
Test Methods: There are various diagnostic tests available to detect Dengue NS1 antigen. This includes enzyme-linked immunosorbent assays (ELISAs) and rapid diagnostic tests (RDTs), both of which provide results quickly. Furthermore, other dengue diagnostic tests such as IgM/IgG antibody tests should also be run alongside these ELISA/RDT combo tests for a more comprehensive assessment of infection status.
Interpreting Test Results: When looking at Dengue NS1 antigen test results, positively indicates the presence of dengue virus and acute dengue infection; however, false positives may arise and further testing may be required for confirmation purposes. When interpreting these test results, clinical evaluation, patient history review, and laboratory findings must all be taken into consideration before reaching a decision on them.
Clinical Utility: NS1 antigen detection can not only serve a diagnostic role but can also identify individuals at higher risk for severe dengue, such as those with elevated NS1 levels. Early identification allows for timely monitoring and necessary medical interventions that could prevent complications.
Dengue NS1 antigen testing is an invaluable way to quickly and accurately identify dengue fever infections in their early stages, providing timely care and management of this serious viral illness. However, as part of an overall approach, it should be combined with additional diagnostic tests and clinical assessments in order to confirm and assess severity.
Differences Among Dengue IgG, IgM, and NS1 Antibodies
Dengue IgG, IgM, and NS1 markers are three commonly used to detect dengue fever. Here are their main differences:
Timing of Appearance for Dengue IgM: Dengue IgM antibodies typically appear within three days after symptoms begin, often being detectable within days and persisting for up to several weeks after.
Dengue IgG Antibodies: Dengue IgG antibodies typically appear later during an infection’s course and typically begin accumulating several days post-symptom onset; they can continue producing antibodies months or even years after symptoms have subsided.
Dengue NS1 Antigen: Dengue NS1 antigen can be detected early in infection, even before antibodies form. Usually present during the initial days or so of illness and for up to one week afterward.
Diagnostic Importance of IgM Antibodies in Dengue Fever: Positive results on an IgM test indicate recent or acute dengue infection, making this test useful in early diagnosis and confirmation of dengue fever. A positive IgM result may also signal an ongoing immune response against this virus.
Dengue IgG: Antibody detection by IgG testing indicates past exposure or infection with the dengue virus. IgG tests help assess a person’s immunity status and history of dengue infection; positive IgG results suggest prior immunity against it.
Dengue NS1 Antigen Detection: Early diagnosis of dengue infection using the NS1 antigen detection test can be particularly useful, providing rapid confirmation early in an illness’s course, often before antibodies have formed and have had time to produce their immune responses. A positive result for active dengue infection.
Duration of Presence for IgM Antibodies in Dengue Fever: Dengue IgM antibodies typically remain detectable for several weeks during the acute phase of infection and may continue to persist for up to several months or even longer afterward.
Dengue IgG Antibodies: Dengue IgG antibodies appear later during infection and may remain for months or even years after its resolution.
Dengue NS1 Antigen: NS1 antigen can typically be detected during the early days of illness, typically up to approximately one-week post-infection, but may no longer be present in your bloodstream during later stages.
Interpretation of test results: Dengue IgM results can provide evidence of recent or acute dengue infection and are frequently combined with clinical symptoms and laboratory findings for accurate dengue diagnosis.
Dengue IgG Results: Positive results indicate exposure or past infection with dengue virus; it does not represent current infection status but instead serves as evidence that you may have immunity against further outbreaks of dengue virus infection.
Dengue NS1 Test Results: A positive NS1 result indicates an active dengue infection, making it ideal for early diagnosis during the early stages of illness.
Dengue IgM can be used to detect recent or acute dengue infections; Dengue IgG indicates past exposure or past infection; while Dengue NS1 provides early diagnostic support during the initial stages of infection. Together these markers offer a comprehensive analysis of dengue infection status.
Dengue IgG vs IgM vs NS1 in Tabular Form
Here’s a tabular form comparing Dengue IgG, IgM, and NS1 based on their key characteristics:
| Characteristic | Dengue IgG | Dengue IgM | Dengue NS1 |
| Timing of appearance | Appears later in the infection | Appears early in the infection | Early detection of the infection |
| Diagnostic significance | Indicates past exposure or previous infection | Indicates recent or acute dengue infection | Confirms acute dengue infection |
| Duration of presence | Can persist for months to years | Can persist for several weeks | Present during the first few days of illness |
| Interpretation of test results | Indicates immunity to the virus | Confirms current infection | Confirms current infection |
| Use in diagnosis | Assesses immune status and history of infection | Confirms recent infection | Early diagnosis in the acute phase |
| Clinical significance | Past exposure, history of infection | Recent infection, active immune response | Early confirmation of infection |
Please note that the information provided in this table is a general overview, and individual cases may vary. It is essential to consult healthcare professionals for accurate interpretation and diagnosis based on specific circumstances.
What Are the Similarities Between Dengue IgG IgM and NS1?
Although Dengue IgG, IgM, and NS1 each exhibit unique qualities, there are similarities among them that should not be ignored. Here are these shared traits:
Diagnostic Markers for Dengue Fever: IgG, IgM, and NS1 antibodies serve as reliable indicators of dengue infection while simultaneously measuring an individual’s immune response to dengue fever infection.
Indicators of Dengue Infection: Three markers–IgG, IgM, and NS1–are indicators of dengue virus infection used to detect and diagnose dengue fever among individuals.
Blood-based detection: Dengue IgG, IgM, and NS1 antibodies can be detected in blood samples by laboratory tests performed to identify them as present markers for dengue infection.
Importance in Dengue Diagnosis: Dengue IgG, IgM, and NS1 antibodies can provide healthcare professionals with an accurate evaluation of infection status as they make accurate diagnoses and determine stages.
Interpretation In Conjunction With Clinical Evaluation: Interpreting Dengue IgG, IgM, and NS1 results should be combined with clinical assessment, patient history review, and any relevant laboratory results to achieve an accurate picture of dengue infection status.
Dengue IgG, IgM, and NS1 all play vital roles in diagnosing dengue fever. All three help identify and manage its spread more easily.
Conclusion
Differentiating Dengue IgG, IgM, and NS1 antibodies is integral in diagnosing and managing dengue fever:
Dengue IgM antibodies appear early during infection to confirm current or acute dengue fever outbreaks. They serve to verify any ongoing or recent dengue issues that might exist.
Dengue IgG antibodies appear later during an infection’s course and indicate past exposure or previous infection with the dengue virus, making IgG testing useful in evaluating an individual’s immunity status and possible history of dengue infection.
Dengue NS1 antigen can be detected early in an infection’s course even prior to producing antibodies and provides an early marker of acute dengue infections.
Timing, duration, and significance of these markers vary significantly; thus utilizing IgG, IgM, and NS1 tests in combination with clinical evaluation and laboratory findings provides a thorough assessment of dengue infection status.
