When it comes to understanding the complexities of pharmacology, it’s critical to get a handle on the contrasts between different medicate impacts. We’ll examine the fundamental dissimilarities between cholinergic and anticholinergic impacts. By delving into the distinctive mechanisms of these effects, we aim to provide you with a comprehensive understanding of how these two pharmacological actions differ and their significance in medical applications.
Definition of cholinergic and anticholinergic
- Cholinergic: Cholinergic alludes to the actuation or incitement of the cholinergic framework within the body. The cholinergic framework may be a portion of the autonomic anxious framework and is characterized by the discharge, activity, or impact of the neurotransmitter acetylcholine. Cholinergic substances or operators upgrade the impacts of acetylcholine by officially enacting cholinergic receptors. Incitement of the cholinergic framework ordinarily leads to expanded smooth muscle compression, glandular emissions, and enactment of the parasympathetic apprehensive framework. Cholinergic drugs can be utilized remedially to upgrade cholinergic movement in conditions such as Alzheimer’s infection and myasthenia gravis.
- Anticholinergic: Anticholinergic alludes to the blocking or hindrance of the cholinergic framework. Anticholinergic substances or specialists act by blocking the activity of acetylcholine at cholinergic receptors, in this way decreasing or hindering the impacts of acetylcholine. Anticholinergic drugs are commonly utilized to square the parasympathetic apprehensive framework and restrain the impacts of intemperate cholinergic action. They can cause relaxation of smooth muscle, reduce glandular secretions, and have various other effects such as drying of secretions, dilation of pupils, and sedation. Anticholinergic solutions are utilized within the treatment of conditions such as overactive bladder, movement affliction, and certain sorts of gastrointestinal clutters.
Cholinergic substances improve the impacts of acetylcholine, whereas anticholinergic substances hinder or square the effects of acetylcholine within the body.
Importance of cholinergic and anticholinergic systems in the body
Cholinergic and anticholinergic frameworks play pivotal parts within the body, especially in controlling different physiological forms.
Here are the key reasons for the significance of these frameworks:
Cholinergic Framework:
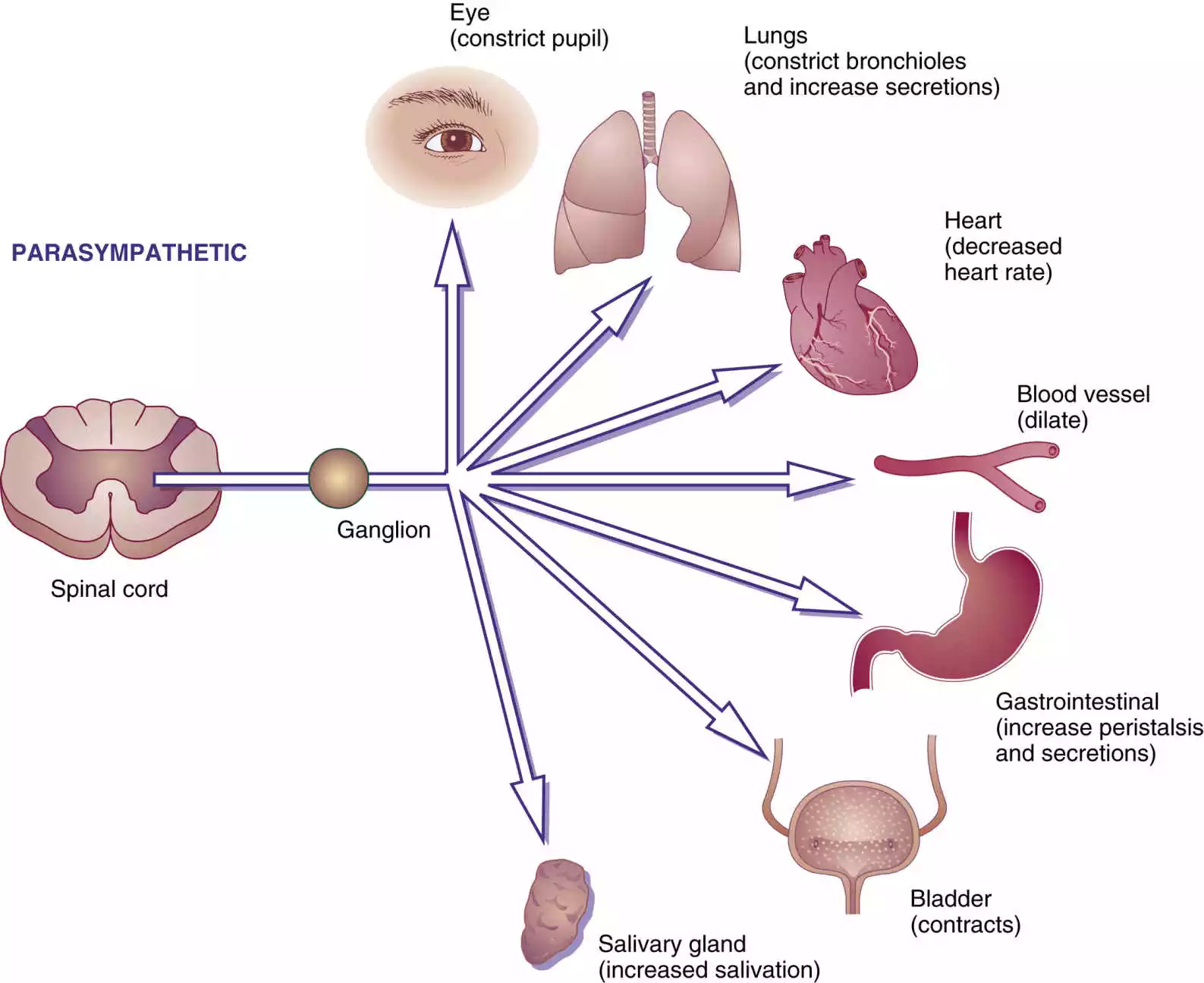
- Autonomic Nervous System: The cholinergic framework could be a major component of the autonomic apprehensive framework, which controls automatic substantial capacities. It works in opposition to the sympathetic nervous system. Enactment of cholinergic receptors intercedes the parasympathetic reaction, capable of capacities like assimilation, salivation, abating heart rate, and withdrawal of smooth muscles within the gastrointestinal tract.
- Cognitive Functions: The essential neurotransmitter within the cholinergic framework, is significant for cognitive forms such as learning, memory, consideration, and excitement. Cholinergic neurons project to areas involved in these functions, including the hippocampus and cerebral cortex. Disturbances in the cholinergic movement are related to cognitive disarranges such as Alzheimer’s malady.
- Neuromuscular Junction: The cholinergic framework plays an imperative part at the neuromuscular intersection, where acetylcholine is discharged to transmit signals from engine neurons to skeletal muscles. This process initiates muscle contractions required for movement and locomotion.Anticholinergic System:
- Balance of Autonomic Functions: Whereas the cholinergic framework advances parasympathetic reactions, the anticholinergic framework counterbalances this by repressing or lessening cholinergic action. This dynamic interplay between the two systems ensures the proper regulation and balance of autonomic functions in the body.
- Medicinal Applications: Anticholinergic drugs have diverse therapeutic uses. They can be utilized to treat conditions such as overactive bladder, movement affliction, unremitting obstructive pneumonic infection (COPD), asthma, gastrointestinal clutters, and Parkinson’s malady. By blocking cholinergic receptors, these medications help alleviate symptoms associated with excessive cholinergic activity in specific organs or systems.
Understanding the cholinergic and anticholinergic frameworks is fundamental for healthcare experts, as the awkward nature or dysfunctions in these frameworks can contribute to different obsessive conditions. By modulating cholinergic and anticholinergic activity, it becomes possible to manage and treat several disorders and improve overall well-being.
What is Cholinergic System?
The cholinergic framework could be a component of the autonomic apprehensive framework, which is mindful of directing automatic substantial capacities. It essentially includes the discharge, activity, and impact of the neurotransmitter acetylcholine (ACh). The cholinergic framework plays an imperative part in different physiological forms all through the body.
Key components of the cholinergic framework incorporate:
- Cholinergic Neurons: These are specialized nerve cells that synthesize and discharge acetylcholine. Cholinergic neurons are found in particular districts of the central apprehensive framework (CNS), such as the basal forebrain, hippocampus, and brainstem, as well as in fringe apprehensive framework ganglia.
- Cholinergic Receptors: These are proteins located on the surface of target cells that bind acetylcholine, initiating a response within the cell. There are two essential sorts of cholinergic receptors: nicotinic receptors and muscarinic receptors. Nicotinic receptors are found within the CNS, autonomic ganglia, and neuromuscular intersections, whereas muscarinic receptors are essentially found in target organs innervated by the parasympathetic apprehensive framework.
- Functions and Effects: The cholinergic system has widespread effects on various bodily functions.
- a. Autonomic Functions: Enactment of cholinergic receptors within the parasympathetic apprehensive framework advances rest and assimilation, controlling capacities such as heart rate, gastrointestinal motility, salivation, and glandular discharges.
- b. Neuromuscular Junction: Acetylcholine is discharged at the neuromuscular intersection, where it ties to nicotinic receptors on skeletal muscles, starting muscle withdrawals required for the development.
- c. Cognitive Functions: Acetylcholine plays a pivotal part in cognitive forms such as learning, memory, consideration, and excitement. Cholinergic projections from particular brain locales, such as the basal forebrain, balance cortical action and contribute to cognitive capacities.
- d. Sensory Processing: The cholinergic framework is included in tangible preparing, counting visual handling, consideration of jolts, and control of torment recognition.
Awkward nature or dysfunctions within the cholinergic framework can contribute to different disarranges, such as Alzheimer’s malady, myasthenia gravis, and autonomic dysfunctions. Restoratively, drugs that influence the cholinergic framework, such as cholinesterase inhibitors, are utilized to oversee conditions like Alzheimer’s infection and improve cholinergic action.
Role of acetylcholine in the cholinergic system
Acetylcholine (ACh) could be a key neurotransmitter within the cholinergic framework and plays a vital part in transmitting signals between nerve cells and facilitating various physiological forms.
Here are the essential parts of acetylcholine within the cholinergic framework:
- Neurotransmission: Acetylcholine acts as a chemical delivery person that empowers communication between nerve cells (neurons). It is released from the presynaptic neuron into the synapse, the small gap between neurons, upon neuronal activation. Acetylcholine atoms at that point tie to particular receptors on the postsynaptic neuron, starting a reaction within the target cell.
- Autonomic Nervous System: Acetylcholine could be an essential neurotransmitter within the parasympathetic department of the autonomic apprehensive framework. It is released by parasympathetic neurons to transmit signals to target organs and regulate various involuntary functions, including heart rate, digestion, glandular secretions, and smooth muscle contraction in the gastrointestinal tract.
- Neuromuscular Junction: Acetylcholine plays an imperative part within the neuromuscular intersection, which is the association between engine neurons and skeletal muscles. When a motor neuron is sanctioned, acetylcholine is released into the neuromuscular crossing point, where it ties to nicotinic acetylcholine receptors on the surface of muscle cells. This binding triggers a series of events that lead to muscle contraction, enabling voluntary movement.
- Cognitive Functions: Acetylcholine is involved in numerous cognitive processes, including learning, memory, attention, and arousal. Cholinergic neurons beginning within the basal forebrain extend to regions such as the hippocampus and cerebral cortex, which are pivotal for memory arrangement and cognitive capacities. Disturbances within the cholinergic framework, especially a decrease in acetylcholine levels, are related to cognitive clutters such as Alzheimer’s illness.
- Sensory Processing: Acetylcholine also plays a role in sensory processing. In the visual system, cholinergic projections from the brainstem to the visual cortex modulate visual processing and attention to visual stimuli. Acetylcholine is included within the direction of torment recognition and tweak of tangible inputs.
Acetylcholine acts as a neurotransmitter within the cholinergic framework, transmitting signals between neurons and impacting different physiological forms, counting autonomic capacities, neuromuscular action, cognitive capacities, and tangible handling. Its balanced release and regulation are essential for maintaining proper bodily functions.
Effects of cholinergic stimulation
Cholinergic incitement alludes to the enactment or upgrade of the cholinergic framework within the body, regularly by expanding the discharge or activity of acetylcholine (ACh) or by specifically fortifying cholinergic receptors.
The impacts of cholinergic incitement can be watched in different organs and frameworks all through the body. Here are some of the key effects:
- Smooth Muscle Contraction: Cholinergic stimulation leads to the contraction of smooth muscles present in organs such as the gastrointestinal tract, urinary bladder, bronchi of the lungs, and blood vessel walls. This effect promotes digestion, helps propel food through the digestive system, assists in urine expulsion, and aids in respiration.
- Glandular Secretions: Cholinergic stimulation increases the secretion of various glands, including salivary glands, lacrimal glands (tear production), and glands in the respiratory and gastrointestinal tracts. This increase in glandular secretions helps maintain moisture and lubrication in these areas, facilitating digestion, respiration, and visual clarity.
- Parasympathetic Nervous System Activation: The cholinergic framework is related to the parasympathetic department of the autonomic anxious framework. Cholinergic incitement actuates the parasympathetic reaction, driving a diminish in heart rate, choking of students (miosis), incitement of assimilation, and unwinding of the urinary bladder.
- Cognitive Effects: Acetylcholine is included in cognitive forms such as learning, memory, consideration, and excitement. Cholinergic incitement in particular brain locales, especially the basal forebrain, can upgrade cognitive capacities, counting memory combination, and attentional center.
- Other Effects: Cholinergic stimulation can also influence other physiological processes, including regulation of blood pressure, modulation of pain perception, modulation of sensory inputs, and regulation of sleep-wake cycles.
Cholinergic incitement can be utilized to improve cholinergic movement in certain therapeutic conditions. Cholinergic drugs or cholinesterase inhibitors are utilized to oversee Alzheimer’s malady, myasthenia gravis, and conditions related to decreased cholinergic transmission.
It’s imperative to note that intemperate cholinergic incitement can lead to antagonistic impacts such as over-the-top salivation, expanded sweating, stomach spasms, loose bowels, bradycardia (moderate heart rate), and bronchoconstriction. The balance and regulation of cholinergic stimulation are crucial to maintaining optimal bodily functions.
What is Anticholinergic System?
Anticholinergic specialists work by authoritative to cholinergic receptors without actuating them. By occupying the receptor sites, they prevent ACh from binding and exerting its effects. This blockade leads to a reduction or inhibition of cholinergic activity in various organs and systems.
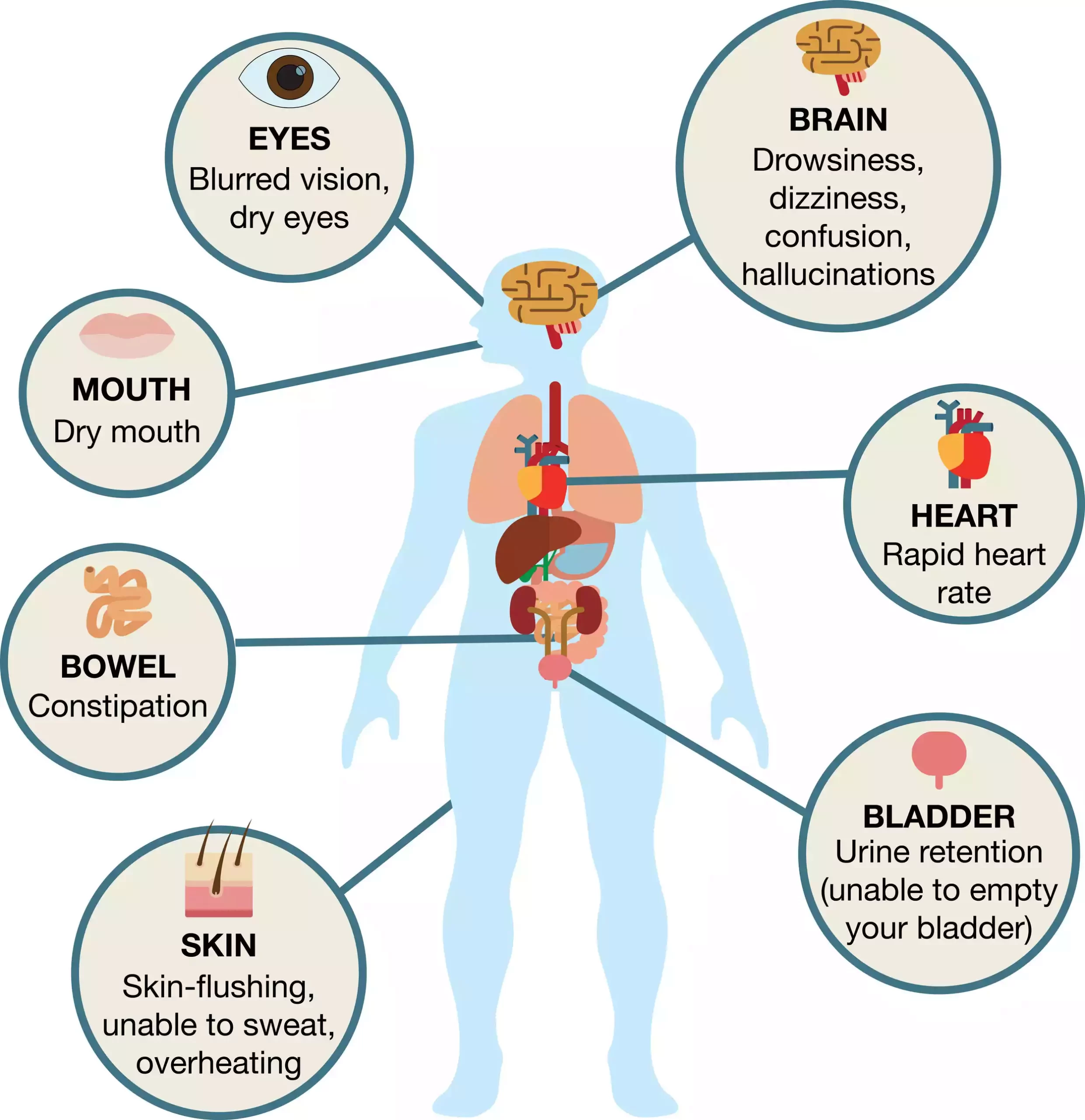
The effects of anticholinergic substances include:
- Relaxation of Smooth Muscle: Anticholinergics cause the relaxation of smooth muscles found in the gastrointestinal tract, urinary bladder, and respiratory system. This effect can help alleviate spasms and reduce hyperactivity in these organs.
- Reduction in Glandular Secretions: Anticholinergic drugs can decrease secretions from glands such as salivary glands, lacrimal glands (tears), and mucous glands in the respiratory and gastrointestinal tracts. This drying effect can be beneficial in conditions such as excessive salivation or excessive nasal and bronchial secretions.
- Inhibition of Parasympathetic Nervous System: The essential target of anticholinergic specialists is the parasympathetic department of the autonomic anxious framework. By blocking the effects of ACh, they reduce parasympathetic activity and counterbalance excessive cholinergic stimulation. This may lead to impacts such as expanded heart rate, student expansion (mydriasis), diminished gastrointestinal motility, and unwinding of the urinary bladder.
- Influence on Cognitive Functions: Anticholinergic substances can have central nervous system effects, including impairment of cognitive functions. They can cause side impacts such as disarray, memory challenges, laziness, and diminished consideration.
- Other Effects: Anticholinergics can also affect other physiological processes, such as raising body temperature by interfering with sweat production and dilation of blood vessels.
It is imperative to note that whereas anticholinergic operators can be useful in certain therapeutic conditions, they can moreover have side impacts, particularly in tall dosages or delayed utilization. These side impacts may incorporate dry mouth, obstruction, obscured vision, urinary maintenance, cognitive disability, and expanded heart rate.
Role of anticholinergic substances in blocking acetylcholine
Anticholinergic substances play a crucial portion in blocking the impacts of acetylcholine (ACh) inside the body. They work by binding to cholinergic receptors without activating them, thus preventing ACh from binding to and activating the receptors. This blockade inhibits the actions of ACh and reduces or blocks cholinergic activity in various organs and systems.
Here are the key roles of anticholinergic substances in blocking acetylcholine:
- Cholinergic Receptor Blockade: Anticholinergic substances, moreover known as anticholinergic operators or opponents, competitively tie to cholinergic receptors. By occupying the receptor sites, they effectively block ACh from binding and exerting its effects. This bar can happen at both muscarinic receptors (found in target organs innervated by the parasympathetic apprehensive framework) and nicotinic receptors (found in autonomic ganglia and the neuromuscular intersection).
- Counteracting Excessive Cholinergic Stimulation: Anticholinergics are commonly used to counteract the effects of excessive cholinergic activity or to selectively block the parasympathetic nervous system. In conditions like an overactive bladder, anticholinergic drugs can repress the intemperate withdrawals of the bladder’s smooth muscle that result from expanded cholinergic action.
- Relaxation of Smooth Muscle: By blocking cholinergic receptors, anticholinergic substances cause the relaxation of smooth muscles present in organs such as the gastrointestinal tract, urinary bladder, bronchi of the lungs, and blood vessel walls. This relaxation effect can help alleviate spasms, reduce hyperactivity, and promote bronchodilation.
- Reduction in Glandular Secretions: Anticholinergics can decrease the secretion of various glands, including salivary glands, lacrimal glands (tears), and mucous glands in the respiratory and gastrointestinal tracts. This drying effect can be useful in conditions such as excessive salivation or excessive nasal and bronchial secretions.
- Modulation of Autonomic Functions: Anticholinergic substances selectively block the parasympathetic branch of the autonomic nervous system, which is primarily mediated by cholinergic transmission. By restraining cholinergic action, they can lead to impacts such as expanded heart rate, student widening (mydriasis), diminished gastrointestinal motility, and unwinding of the urinary bladder.
- Medicinal Applications: Anticholinergic drugs have therapeutic uses in various medical conditions. They can be endorsed to oversee overactive bladder, movement affliction, gastrointestinal disarranges (e.g., crabby bowel disorder), inveterate obstructive aspiratory infection (COPD), asthma, and certain neurological conditions. By blocking cholinergic receptors, these medications help alleviate symptoms associated with excessive cholinergic activity in specific organs or systems.
It’s imperative to note that the utilization of anticholinergic substances ought to be done under restorative supervision, as they can have side impacts and intuitive with other solutions. The balance and regulation of cholinergic activity are essential for maintaining optimal bodily functions, and anticholinergic substances provide a means to selectively block or inhibit these effects when needed.
Effects of anticholinergic blockade
Anticholinergic blockade insinuates the inhibitory effect of anticholinergic substances on the cholinergic system by blocking the exercises of acetylcholine (ACh). This blockade leads to a reduction or inhibition of cholinergic activity in various organs and systems throughout the body.
Here are some of the effects commonly associated with anticholinergic blockade:
- Smooth Muscle Relaxation: Anticholinergics cause relaxation of smooth muscles found in the gastrointestinal tract, urinary bladder, bronchi of the lungs, and blood vessel walls. This relaxation effect can alleviate spasms, reduce hyperactivity, and promote bronchodilation.
- Reduction in Glandular Secretions: Anticholinergic substances decrease the secretion of various glands, including salivary glands, lacrimal glands (tears), and mucous glands in the respiratory and gastrointestinal tracts. This drying effect can be useful in conditions such as excessive salivation or excessive nasal and bronchial secretions.
- Inhibition of Parasympathetic Nervous System: The essential target of anticholinergic operators is the parasympathetic department of the autonomic apprehensive framework. Block this will lead to impacts such as expanded heart rate, understudy expansion (mydriasis), diminished gastrointestinal motility, and unwinding of the urinary bladder.
- Cognitive Effects: Anticholinergic substances can have central nervous system effects, including cognitive impairment. They can cause side impacts such as disarray, memory challenges, diminished consideration, and tiredness. These impacts are especially noteworthy with tall measurements or delayed utilization of anticholinergics.
- Other Effects: Anticholinergic blockade can influence various other physiological processes, including raising body temperature by interfering with sweat production, decreasing saliva production, causing dry mouth, and affecting the dilation of blood vessels.
It’s vital to note that whereas anticholinergic bars can be useful in certain restorative conditions, such as within the treatment of overactive bladder or respiratory disarranges, they can too have side impacts, particularly in tall measurements or delayed utilization. These side impacts may incorporate dry mouth, obscured vision, urinary maintenance, obstruction, cognitive impedance, expanded heart rate, and diminished sweating.
The impacts of anticholinergic bars ought to be carefully checked and overseen by healthcare experts to guarantee an adjustment between helpful benefits and potential side impacts.
Comparison Chart
Sure! Here’s a comparison chart highlighting the key differences between cholinergic effects and anticholinergic effects:
| Aspect | Cholinergic Effects | Anticholinergic Effects |
|---|---|---|
| Smooth Muscle | Contraction | Relaxation |
| Glandular Secretions | Increase | Decrease |
| Parasympathetic System | Activation | Inhibition |
| Cognitive Effects | Enhances cognitive functions (e.g., memory, attention) | Impairs cognitive functions (e.g., memory, attention) |
| Sensory Processing | Modulates sensory processing (e.g., visual processing, pain) | May affect sensory processing |
| Heart Rate | Decreases | Increases |
| Pupils | Constricts (miosis) | Dilates (mydriasis) |
| Gastrointestinal | Stimulates digestion and increases motility | Reduces motility |
| Urinary Bladder | Promotes relaxation | Promotes relaxation |
| Sweating | May increase | May decrease |
| Salivation | Increases | Decreases |
| Cognitive Effects | Enhances cognitive functions | Can cause cognitive impairment |
| Other Effects | Modulates sensory inputs, arousal | Can cause dry mouth, blurred vision, constipation, etc. |
Please note that this chart provides a general overview of the differences between cholinergic and anticholinergic effects. The specific effects may vary depending on the context, dosage, and individual response to medications or physiological conditions.
Conclusion
Understanding the distinction between cholinergic and anticholinergic impacts is basic for healthcare experts and people looking for experiences in pharmacological activities. While cholinergic effects involve the activation or enhancement of the cholinergic system, anticholinergic effects inhibit or block its actions. By comprehending these distinct mechanisms, we can better appreciate the medical applications and therapeutic significance of drugs acting on the cholinergic and anticholinergic systems.
