Brief Overview of MS and Lyme Disease
Multiple Sclerosis (MS): Multiple Sclerosis (MS) is an incurable neurodegenerative disorder that affects neurological and spinal cord function and requires proper management to ensure longevity. It is classified as an autoimmune disorder. This means that our immune system attacks healthy tissues of the body.
In MS your immune system targets the coating of nerve fibers known as myelin. Myelin assists in the transmission of nerve impulses, which allows for efficient transmission between brain cells and various other areas in the body. The body’s immune system attacks and destroys myelin cells, which results in scar tissue (sclerosis) across multiple parts of the CNS which can disrupt nerve signals.
Researchers are still unable to fully comprehend what causes multiple sclerosis (MS) However, a lot of believe that a combination of genetic and environmental causes. Most of those affected include young people between 20 to 40. Women are at a higher risk for cancer-related problems than males.
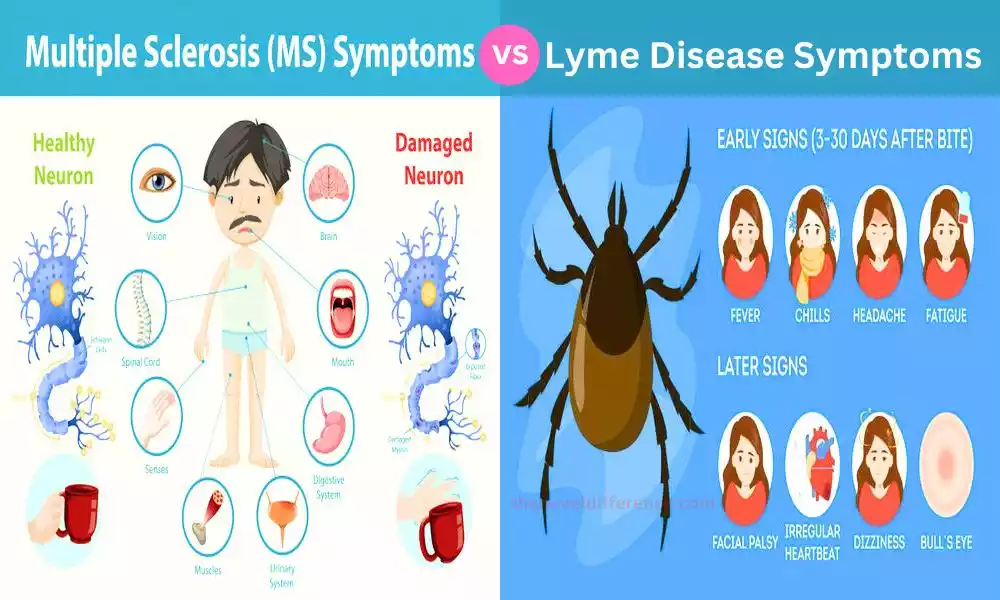
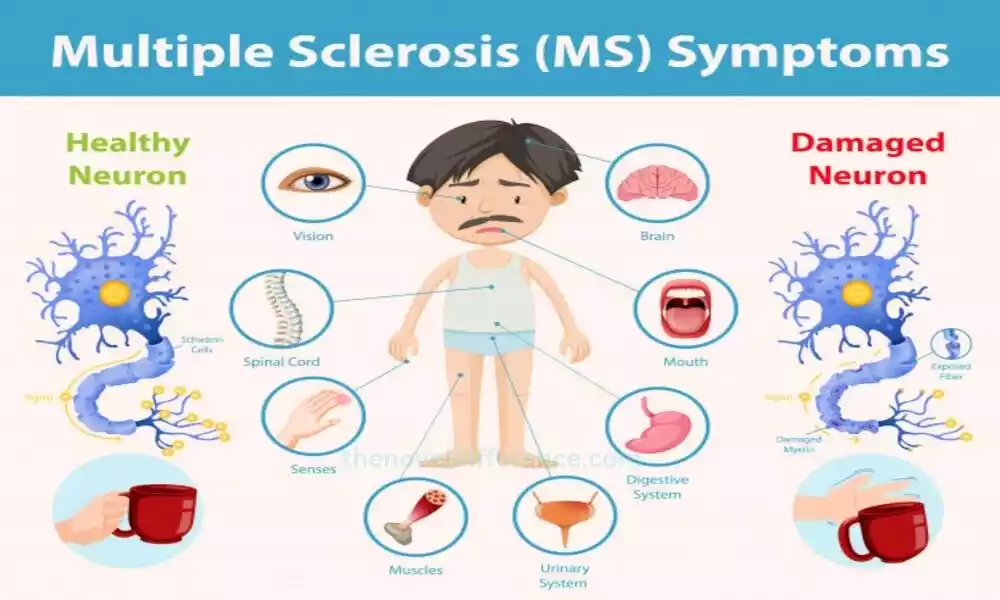
The signs and symptoms of MS differ widely based on the extent and location of damage to nerves. Common symptoms may include muscle weakness, fatigue during walking and difficulties walking; numbness/tingling sensation; issues related to balance/coordination/vision issues/bladder or bowel issues/cognitive impairment, and mood disorders are some common indicators.
Determining whether you have Multiple Sclerosis can be challenging due to no definitive test available to detect it. Doctors usually rely on symptoms combined with neurological examinations, medical history reviews, and imaging tests such as an MRI to make accurate diagnoses and determine any issues or diseases, or problems.
There remains an unsolved challenge surrounding MS, although many treatments exist that aim to manage its symptoms, slow its progress, and enhance the quality of life for sufferers.
This could include treatments that target disease to lower inflammation and activity of the immune system as well as symptom-management medication as well as rehabilitation therapies and treatment for supportive conditions.
MS is a complicated and unpredictably recurring disease, with every patient having a distinct course of illness. Certain people might experience minimal symptoms and periods of remission, whereas others might have more severe and more progressive types in the course of their disease. Research is ongoing to better understand the fundamental mechanisms that cause MS better and to develop more efficient treatment options.
Lyme Disease: Lyme Disease, more formally known as Borrelia burgdorferi, can be spread via tick bites; deer ticks can directly transmit Lyme through their bites. Lyme disease was first identified in Lyme, Connecticut where its first case was first detected back in the 1970s.
Lyme Disease can only be spread between humans via these bites from infected black-legged ticks that carry this bacteria causing the bites.
Disease cases have been found across North America, Europe, and Asia where ticks that carry bacteria are prevalent. Ticks become infected with B. burgdorferi by feeding on infected animals such as mice, birds, or deer. Once an infected tick bites a human, the bacteria it contains can spread and lead to Lyme Disease.
The clinical presentation of Lyme Disease can vary and typically occurs in three stages.
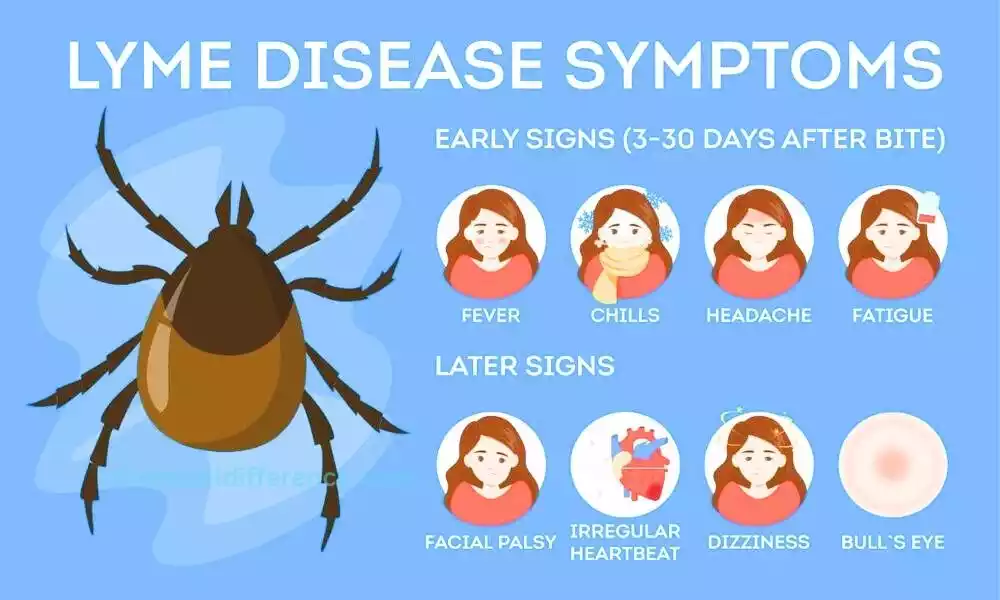
Early Localized Stage: Within a few days to weeks after the tick bite, an expanding red rash called erythema migrans (EM) may appear at the site of the tick bite. The rash is often circular or oval-shaped and can expand over time. Flu-like symptoms including fever, fatigue, headache, muscle and joint ache as well as swollen lymph nodes may also be evident.
Early Disseminated Stage: Left untreated, an infection may spread rapidly through your body causing more widespread symptoms and leading to further illness. These may include additional EM rashes appearing in different areas, neurological symptoms such as facial paralysis, meningitis, numbness or tingling in the extremities, and cardiac abnormalities.
Late Disseminated Stage: If the infection remains untreated for an extended period, it can progress to the late disseminated stage. At this stage, patients may experience persistent joint pain and swelling as well as neurological symptoms like memory issues, difficulty focusing, neuropathy, and more uncommon manifestations affecting skin, eyes, and organs.
Diagnosing Lyme Disease can be challenging due to symptoms overlapping with those from other conditions and laboratory tests often failing to confirm them in early stages. A diagnosis typically relies on clinical symptoms, history of tick exposure, and (if required) blood tests designed to detect antibodies against B. burgdorferi bacteria.
Treatment for Lyme Disease typically involves antibiotics. Antibiotic treatments depend upon the stage and severity of infection. Early diagnosis and prompt treatment are key to stopping its progress and limiting complications from emerging.
Individuals may experience persistent symptoms even after appropriate treatment, a condition known as post-treatment Lyme Disease syndrome (PTLDS). PTLDS remains unclear and research efforts continue to uncover and manage this condition more fully.
Prevention is essential in reducing the risk of Lyme Disease. This includes taking precautions when spending time in areas where ticks are prevalent, such as wearing protective clothing, using tick repellents, and conducting thorough tick checks after outdoor activities.
Understanding Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is an incapacitating neurological disease that attacks central nerve structures – particularly the spinal cord and brain. It’s considered an auto-immune condition and means that the immune system targets healthy tissues by itself.
In MS the immune system can target the myelin, a type of nerve fiber that is found in. Myelin aids in communication between nerve signals and facilitates effective communication between the brain as well as various other parts of the human body.
The immune system tries to destroy and damage myelin cells, which results in scar tissue (sclerosis) throughout the various areas of the CNS which can disrupt nerve signals.
Researchers do not yet fully comprehend what triggers Multiple Sclerosis; however, many think its origin could lie in both genetic and environmental. It’s thought to result due to an abnormal immune response, triggered by unidentified triggers, such as due to a virus or environmental triggers.
MS is most commonly a problem for young adults, usually between 20 to 40. Moreover, women are more frequently affected than males. But, the condition can also occur at any time.
The signs of MS can vary greatly based on the area and severity of damage to nerves. Common symptoms are weakness of muscles, fatigue, difficulty walking and sensations of numbness or tingling in various body or localized areas, imbalance and coordination issues as well as visual issues (double vision/blurred vision/bowel/bladder dysfunction etc) cognitive deficits/compulsions as well as mood changes.
MS is a multi-factorial disease which means it manifests differently in different people. There are many forms of MS such as Relapsing-remitting MS (RRMS) which is the most well-known type with a pattern of relapses that are followed by periods of recovery.
Other types are the primary form of MS (PPMS) in which there is a gradual progression of symptoms beginning at the time of onset and then secondary progressive MS (SPMS) that starts as relapsing-remitting MS and then progresses to an advanced course.
Locating MS can be challenging since there is no single method for diagnosing it. Doctors usually rely on symptoms, medical history review, neurological testing (such as MRI imaging tests) as well as cerebrospinal fluid tests to establish whether there is indeed an issue and arrive at an accurate diagnosis.
There is currently an unsolved issue with MS There are a myriad of treatment options that are available to treat the symptoms, stop the progression of disease, and enhance the quality of life.
They could include therapies that modify disease to decrease inflammation and immune system activity, symptoms medication for management (such as those for spasticity, fatigue, or pain), and rehabilitation treatments (such as occupational therapy and physical therapy) as well as supportive treatment.
MS is a nebulous and amorphous disease, with every patient having a distinct course of illness. Certain people might experience minimal symptoms and periods of remission, whereas others might be more severely affected and develop types during their disease. The ongoing research is aimed at helping comprehend the mechanisms behind MS and to develop more effective treatment options.
Definition and basic characteristics
(MS) is a neurological condition caused by abnormal immune system reactions which attack myelin – the protective layer surrounding nerve fibers within the central nervous system. This immune-mediated damage leads to the formation of scar tissue (sclerosis) in multiple areas of the, disrupting the normal transmission of nerve signals.
The basic characteristics of MS include:
Autoimmune Disorder: MS is considered an autoimmune condition because the immune system mistakenly attacks and destroys myelin sheath – essential for nerve fiber health – mistakenly targeting it for attack by mistake. Immune system responses often lead to inflammation, demyelination, and nerve fiber damage.
Central Nervous System Involvement: MS primarily attacks the CNS, including both the brain and spinal cord. Immune-mediated damage may affect various regions of the CNS and cause various neurological symptoms.
Relapsing-Remitting Nature: The most common form of MS is relapsing-remitting MS (RRMS), characterized by episodes of relapses or exacerbations, during which new or worsening neurological symptoms appear. These relapses are followed by periods of remission, where symptoms partially or completely improve.
Heterogeneity of Symptoms: MS can manifest with various symptoms depending on the location and extent of nerve damage. Common symptoms may include fatigue, muscle weakness, coordination or balance issues, numbness/tingling sensations in different parts of the body, vision problems, bladder/bowel dysfunction issues, cognitive changes, or mood disturbances – although severity will depend on individual situations.
Variable Disease Course: MS can have different disease courses. Relapsing-remitting MS is just one type of MS. Other forms include primary progressive MS (PPMS), which involves gradual worsening from initial symptoms; and secondary progressive MS (SPMS), which initially presents as relapsing-remitting but then develops into progressive disease later.
Unpredictable Progression: MS progression can vary significantly between individuals. Some people experience mild symptoms with long periods of remission, while others may have more severe and rapidly progressing diseases. The course of MS is difficult to predict, making it challenging to determine the long-term prognosis for each person.
Impact on Quality of Life: MS is a chronic condition that can significantly diminish an individual’s quality of life, from mobility issues and daily functioning challenges, and employment relationships, to depression symptoms that decrease overall wellness and well-being.
Not every individual will present with MS in the same way; its course can differ according to genetic predisposition, environmental triggers, and individual immune system reactions.
Understanding Lyme Disease
Lyme Disease, caused by Borrelia burgdorferi bacteria found in tick bites, can be an infectious tick-borne condition with serious health implications. The name is derived from Lyme, a town in Lyme, Connecticut, where it was first discovered around the year 1970.
Lyme Disease is primarily transmitted to humans by the bite of black-legged ticks. They are also referred to as deer ticks. These ticks carry the bacteria.
The main things to know regarding Lyme Disease include:
Causative Agent: Lyme Disease is caused by the spirochete bacteria Borrelia Burgdorferi. These bacteria can infiltrate different animals, such as rodents and deer, which serve as reservoir hosts for tick populations.
Transmission: Its primary method of transmission to humans takes place via the bite of black-legged ticks. Ticks contract B. burgdorferi after feeding on animals that are infected. Humans may contract the disease if being bitten by infected ticks usually when they are outdoors in areas with grass or woods.
Geographical Distribution: Lyme Disease is widespread in specific areas of North America, Europe, and Asia in which the ticks which carry the bacteria are discovered. The incidence of the disease may vary across these areas, and there are localized hotspots that could be present.
Clinical Stages: Lyme Disease typically appears in three distinct stages. Initial Localized Stage A couple of days to a few weeks following the bite of a tick the rash, which is red and growing known as erythema migrans (EM) could appear near the spot that the bit. It can be accompanied by symptoms of flu-like headache, fatigue, fever muscle and joint pains and swollen lymph nodes can be present. occur.
b. The early stage of dissemination: If untreated, the illness may spread to other areas in the body leading to more severe symptoms. Other EM eruptions can occur in various areas and neurological signs, like facial paralysis, meningitis, numbness and extreme tingling, and cardiac issues, can appear.
c. late disseminated stage: in situations in which the infection does not get treated and untreated, it may advance into the stage of disseminated late. The stage can be characterized by constant joint swelling and pain or neurological symptoms like memory issues, difficulties concentrating, and neuropathy, and also less well-known symptoms affecting the eyes, skin as well as other organs.
Diagnostics: Diagnosing Lyme Disease isn’t always easy because symptoms can overlap with other ailments and tests in the laboratory aren’t always conclusive, particularly in the beginning stages. The diagnosis is usually dependent on symptoms in the clinical setting and the previous exposure to ticks and when necessary testing in the laboratory, like blood tests that detect the presence of antibodies to B. Burgdorferi.
Treatment: Treatment of Lyme Disease is antibiotics. The type of antibiotic that is used and the time to treat is influenced according to the intensity and duration of the condition. Rapid diagnosis and prompt treatment are essential to slow the progression of the disease as well as to decrease the chance of complications.
Post-Treatment Lyme Disease Syndrome (PTLDS): In some cases, patients may have persistent symptoms even with proper treatment, a condition called PTLDS. The reason behind PTLDS isn’t fully identified, and research is underway to gain a better understanding and control of this condition.
prevention: Prevention is essential in reducing the chance of Lyme Disease. It is vital to take precautions while in areas that are prone to ticks including wearing protective clothes, using tick repellents, and performing thorough tick tests after out in the outdoors.
You must seek out medical help if suspect that you’ve had contact with ticks and you develop symptoms that could be indicative of Lyme Disease. Early diagnosis and treatment may improve outcomes and decrease the chance of complications.
Definition and basic characteristics
Lyme disease, which is caused by Borrelia burgdorferi bacteria may be transferred from human to human through ticks with infected black legs (commonly known as deer ticks) which have carried them for an infection from a bite (known by the name of Lyme Tick in certain regions of North America and Europe).
The basic characteristics of Lyme disease include:
Causative Agent: Lyme disease is caused by Borrelia burgdorferi bacteria. Borrelia bacteria are transmitted to humans through tick bites.
Tick-Borne Transmission: The primary mode of transmission to humans occurs through the bite of infected ticks. Ticks become infected with the bacteria after feeding on infected animals, such as rodents and deer. Humans can contract the disease when bitten by these infected ticks.
Lyme Disease Is Found Globally: Lyme disease can be found throughout North America, Europe, and Asia. The prevalence and risk of Lyme disease can vary within these regions, with higher incidence rates reported in specific areas where infected ticks are more prevalent.
Clinical Presentation: Lyme disease can manifest in several stages, and the symptoms can vary widely. The disease is often categorized into three stages:
a. Early Localized Stage: Within days to weeks after a tick bite, a characteristic expanding red rash called erythema migrans (EM) may develop at the site of the bite. The signs of influenza may include fever, fatigue headaches, joint or muscular pains along with swelling of lymph nodes.
b. Early Disseminated Stage: Without treatment, bacteria can spread throughout your body and lead to further symptoms. These can include multiple EM rashes appearing in different areas, neurological symptoms such as facial paralysis, meningitis, and peripheral neuropathy, as well as cardiac abnormalities.
c. Late Disseminated Stage: In some cases, if left untreated, Lyme disease can progress to the late disseminated stage. At this stage, symptoms could include chronic joint pain and swelling; neurological effects like cognitive impairments, memory issues, and sensory disturbances; as well as less commonly observed manifestations such as skin, eye, or organ issues.
Diagnostic: Lyme disease can be difficult to identify early on due to nonspecific symptoms that could potentially overlap with other conditions. Healthcare providers typically consider clinical symptoms, and history of tick exposure, and may conduct laboratory tests such as blood tests to detect antibodies against the bacteria. At various stages, different tests may be utilized.
Treatment Options for Lyme Disease: Antibiotics such as Doxycycline, Amoxicillin, or Cefuroxime tend to be effective first-line therapies against Lyme disease. Antibiotic selection and duration depend upon several factors including disease progression, severity of symptoms, and other variables. Early treatment is crucial to prevent complications and more severe manifestations.
Prevention: Preventive measures play an essential role in mitigating Lyme disease risk. These measures include avoiding tick-infested areas, using tick repellents, wearing protective clothing (long sleeves, pants, etc.), performing thorough tick checks after outdoor activities, and promptly removing attached ticks.
Lyme disease has various symptoms and affects multiple body systems if left untreated. Early diagnosis, effective treatments, and preventive measures are key elements in effectively managing any disease and lessening its impact on individuals’ health.
Differences Between MS and Lyme Disease
There are several key distinctions between Multiple Sclerosis (MS) and Lyme Disease. These differences lie in their underlying causes, disease progression, clinical presentation, diagnostic approaches, treatment modalities, and long-term effects.
Here are some of the main differences:
Etiology and Causative Agents:
MS: MS is an auto-immune disease in which the immune system attacks the myelin sheath that surrounds nerve fibers that are located in the central nervous system. The precise cause of MS is unclear, however environmental and genetic factors have been suggested to be a factor.
Lyme Disease: Lyme Disease is caused by Borreliaburgdorferi bacteria that are spread through bites of ticks that are infected.
Disease Progression:
MS: MS can have different disease courses, including relapsing-remitting, primary progressive, and secondary progressive. The progression of MS varies widely among individuals, and symptoms can fluctuate over time.
Lyme Disease: If left untreated, Lyme Disease can progress through stages, including early localized, early disseminated, and late disseminated. However, not all individuals with Lyme Disease progress to later stages, and the disease course is generally more linear.
Clinical Presentation:
MS: MS symptoms can vary widely depending on the location and extent of nerve damage. Common symptoms may include fatigue, muscle weakness, coordination difficulties, balance difficulties; numbness/tingling sensation; vision problems; bladder/bowel dysfunction issues; cognitive changes, as well as mood disturbances, are among them.
Lyme Disease: Early symptoms of Lyme Disease often include a characteristic expanding red rash called erythema migrans (EM) along with flu-like symptoms. As the disease progresses, additional EM rashes may appear, and neurological symptoms, joint pain, and other manifestations may occur.
Diagnostic Approaches:
MS: Diagnosing MS requires a combination of clinical evaluation, medical history review, neurological exam findings, imaging studies such as an MRI scan, and sometimes cerebrospinal fluid testing. There is no single definitive test for MS.
Lyme Disease: Diagnosis of Lyme Disease can be challenging due to overlapping symptoms with other conditions. It relies on clinical evaluation, history of tick exposure, and sometimes serological tests to detect antibodies against Borrelia burgdorferi.
Treatment Modalities:
MS: Treatment for MS aims to manage symptoms, slow disease progression, and modify the immune response. This may involve disease-modifying therapies, symptomatic treatments, rehabilitation, and supportive care.
Lyme Disease: Treatment for Lyme Disease primarily involves antibiotics to eliminate the bacteria. Antibiotic selection and duration will depend upon the stage and severity of an infection.
Long-Term Effects:
MS: MS is a debilitating condition that can wreak havoc on all aspects of one’s life – mobility, cognition, and quality of life being among them. The progression and long-term effects of MS vary greatly between individuals.
Lyme Disease: When diagnosed and treated promptly, most individuals with Lyme Disease recover fully. However, in certain instances symptoms may persist or return after Lyme Disease treatment has concluded, leading to post-treatment Lyme Disease Syndrome (PTLDS).PTLDS can cause ongoing symptoms and functional limitations.
Consult healthcare professionals to receive accurate diagnosis and management of either condition as their symptoms can overlap or differ significantly, which requires professional evaluation for effective management.
What are the similarities Between MS and Lyme Disease?
While Multiple Sclerosis (MS) and Lyme Disease are distinct conditions with different underlying causes and characteristics.
There are a few similarities worth noting:
Neurological manifestations: Both MS as well as Lyme Disease can affect the nervous system, which can cause numerous neurological manifestations. This could include numbness or burning sensations as well as muscle weakness, problems in balance and coordination, emotional changes, and troubles. However, the specific presentation and progression of these symptoms can differ between the two conditions.
Fluctuating Symptoms: MS and Lyme Disease can exhibit symptoms that fluctuate over time. Relapses and remissions characterize the disease course, with periods of exacerbations followed by partial or complete improvement. Similarly, in Lyme Disease, symptoms can wax and wane, especially during the early disseminated stage.
Overlapping Symptoms: Some symptoms of MS and Lyme Disease can overlap, leading to diagnostic challenges. Both conditions can present with fatigue, muscle and joint pain, and vision problems. This overlap can make it difficult to differentiate between the two states based solely on symptoms.
Differential Diagnosis: Due to the potential overlap in symptoms, healthcare providers may consider Lyme Disease in the differential diagnosis of individuals with suspected MS, especially in regions where Lyme Disease is prevalent. This is particularly important to ensure appropriate management and treatment decisions.
Effect on Quality of Life Effect on Quality of Life: Both Multiple Sclerosis (MS) and Lyme Disease can significantly diminish individuals’ quality of life because of the long-term character of both conditions as well as their associated symptoms as well as the potential for long-term adverse impacts that can affect mobility, daily activities work relationships, as well as general wellbeing.
Although MS and Lyme Disease share similarities, it’s essential to remember they are separate conditions with separate causes that necessitate distinct approaches for diagnosis and management based on individual symptoms, medical histories, and diagnostic tests.
Consultation with healthcare professionals should always be sought to receive accurate diagnostic advice and appropriate management plans suited for each case.
Side-by-Side Comparison – MS vs Lyme Disease in Tabular Form
Sure! Here is a comparison between Multiple Sclerosis (MS) and Lyme Disease presented as tabular data:
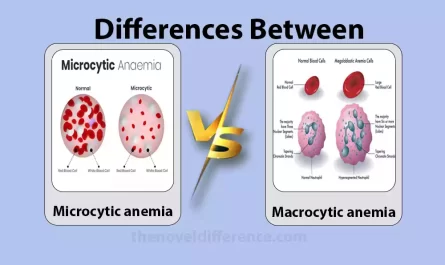
| aspect | Multiple Sclerosis (MS) | Lyme Disease |
|---|---|---|
| Etiology | Autoimmune disorder attacking the myelin sheath | Bacterial infection (Borrelia burgdorferi) |
| Disease Progression | Relapsing-remitting, primary progressive, | Early localized, early disseminated, late |
| secondary progressive | disseminated | |
| Common Symptoms | Fatigue, muscle weakness, coordination | Fatigue, muscle, and joint pain, headaches, |
| and balance problems, numbness or tingling, | fever, flu-like symptoms, swollen lymph | |
| vision problems, bladder/bowel dysfunction | nodes | |
| Diagnostic Approaches | Clinical evaluation, medical history, | Clinical evaluation, history of tick |
| neurological examination, imaging studies, | exposure, serological tests | |
| cerebrospinal fluid analysis | ||
| Treatment | Disease-modifying therapies, symptomatic | Antibiotics (doxycycline, amoxicillin, |
| treatments, rehabilitation, supportive care | cefuroxime) | |
| Long-Term Effects | Can lead to disability, impact the quality of life | Most individuals recover fully, but in |
| In some cases, post-treatment Lyme Disease | ||
| syndrome (PTLDS) can cause persistent | ||
| symptoms and functional limitations | ||
| Geographic Distribution | Worldwide, the varying prevalence of different | Predominantly in regions where infected |
| regions | ticks are prevalent |
Please note that this is a simplified comparison, and individual experiences with these diseases can vary. It is important to consult with healthcare professionals for accurate diagnosis and personalized management.
Overlapping Symptoms and Challenges in Diagnosis
Overlapping symptoms and challenges in diagnosis can occur between Multiple Sclerosis (MS) and Lyme Disease due to similarities in certain clinical presentations.
Some of the overlapping symptoms and challenges in diagnosis include:
Fatigue: Both MS and Lyme Disease can cause fatigue, which is a common symptom in both conditions. Fatigue may be related to multiple sclerosis itself or Lyme disease infection itself, or both conditions could produce fatigue as part of their immune responses to infection.
Neurological Symptoms of MS and Lyme Disease: Numbness or Tingling Sensations, Muscle Weakness, Coordination issues, and Cognitive changes may all be symptoms associated with either disease. These shared symptoms can make it challenging to differentiate between the two conditions based solely on clinical presentation.
Visual Disturbances: Vision problems, such as blurred vision or double vision, can occur in both MS and Lyme Disease. Optic neuritis, inflammation of the optic nerve, can be a specific symptom of MS, but it can also occur in Lyme Disease.
Diagnostic Challenges: Diagnosing MS and Lyme Disease can be challenging due to overlapping symptoms and the need for careful evaluation. Symptoms alone may not provide a conclusive diagnosis; additional testing may be required to distinguish between both conditions.
Geographic Considerations: The geographic distribution of Lyme Disease overlaps with areas where MS is prevalent. This overlap can create challenges in diagnosing patients who present with symptoms common to both conditions, especially in regions where Lyme Disease is endemic.
Healthcare providers may consider various factors when approaching these challenges, including medical history, exposure to ticks and geographic location; diagnostic tests (blood, imaging, or cerebrospinal fluid analysis); consultation with specialists as necessary, and blood samples as samples to make accurate diagnoses.
It’s crucial for individuals experiencing overlapping symptoms or residing in areas where Lyme Disease is prevalent to provide comprehensive medical histories to healthcare professionals. This can help guide the diagnostic process and ensure appropriate treatment decisions are made.
Conclusion
Conclusion Multiple Sclerosis (MS) and Lyme Disease are distinct conditions with distinct root causes, disease courses, and treatment approaches. MS is an autoimmune condition caused by immune cells attacking myelin sheath in the central nervous system while Lyme Disease results from Borrelia Burgdorferi bacteria found on tick bites that spread infection between people.
While there are some overlapping symptoms and diagnostic challenges between MS and Lyme Disease, careful evaluation and consideration of various factors can help differentiate between the two conditions. Diagnostic tests, medical history, exposure to ticks, and geographic considerations play important roles in reaching an accurate diagnosis.